Shoulder Instability | Diagnosis & Treatment for Physiotherapists

Shoulder Instability | Diagnosis & Treatment for Physiotherapists
The shoulder joint has a tremendous degree of mobility, which renders it prone to instability. While muscle forces control stability in mid-ranges of motion, clinical instability presents itself at end range of motion (Doukas et al. 2001). It is defined as abnormal motion of the humeral head on the glenoid, which presents as pain and/or a sense of fear of displacement. Functional stability, which can be defined as maintenance of the humeral head centered within the glenoid fossa during shoulder motion, is achieved through synchronous coordination of static and dynamic components. These include negative intra-articular pressure, glenohumeral bony geometry, the capsulolabral complex, and synergistic muscle balance (Doukas et al. 2001).
The rotator cuff muscles serve to center the humeral head in the glenoid, thereby counteracting the translational forces that are generated by the prime movers of the shoulder. The glenoid labrum is known to increase the depth of the glenoid socket by approximately 50% in all directions and increases surface area as well.
Traumatic instability can range from violent forces that can frankly dislocate the joint to more subtle forces that lead to plastic deformity of the static restraints.
The mechanism of anterior dislocation is typically an abrupt abduction/external rotation force about the shoulder, while posterior most often happens due to seizures, fits, or electrocutions. It is also seen in sports with falls on the elbow, as well as tackling with an outstretched arm and a force into a posterior direction as is the case in rugby tackling.
In case of a dislocation, the following injuries are commonly seen:
- Glenoid fractures in 15 – 21% of cases (Kraeutler et al. 2018, Griffith et al. 2008)
- Bankart lesion: Detachment of the IGHL from the anterior glenoid and labrum in 84-97% of anterior dislocations (Kraeutler et al. 2018, Sedeek et al. 2014)
- Hill-Sachs lesion: Impression on the dorsal side of the humeral head after anterior dislocation in 41-83% (Kraeutler et al. 2018, Ozaki et al. 2014)
- Rotator cuff tears in 1,2% of patients in a study with a mean age of 24 (Kraeutler et al. 2018) up to 33.4% prevalence for rotator cuff tears and/or fractures of the greater tuberosity in a study with mean age of 47.6 years (Robinson et al. 2012)
- Neural injury to the axillary nerve and/or other parts of the brachial plexus in 13,5% (Robinson et al. 2012)
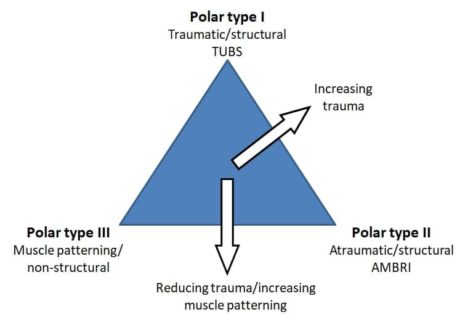 Jaggi et al. (2017) propose the Stanmore classification for the rehabilitation of shoulder instability. They mention that both structural (rotator cuff, surface area of contact, capsulolabral complex) and non-structural (central and peripheral nervous system) components are contributing to shoulder instability and stress that a continuum exists between pathologies.
Jaggi et al. (2017) propose the Stanmore classification for the rehabilitation of shoulder instability. They mention that both structural (rotator cuff, surface area of contact, capsulolabral complex) and non-structural (central and peripheral nervous system) components are contributing to shoulder instability and stress that a continuum exists between pathologies.The structural elements may be congenitally abnormal, comprise abnormal collagen, acquired micro traumatic lesions over time (atraumatic structural), or be damaged by extrinsic factors (traumatic structural). The non-structural elements can be congenitally abnormal or acquired over time as perturbations of neuromuscular control.
The Stanmore classification is as follows:
Pole I: Traumatic (TUBS = Traumatic, unilateral, Bankart lesion, surgery)
Pole II: Atraumatic (AMBRI = atraumatic, multidirectional, bilateral, rehabilitation, inferior capsular shift)
Pole III: Neuromuscular
Epidemiology
Shields et al. (2017) retrospectively examined collected trauma databases and found an incidence rate of 21.9 dislocations per 100.000 people in an urban population. They report a peak incidence of 42.1 and 50.9 in the 15-24 and ≥85 age group for males and a peak of 45.7 for females in the age group between 65 and 74.
Finhoff et al. (2004) constitute that more than 75% of cases of shoulder instability are due to trauma, with the remaining 25% categorized as non-traumatic.
Blomquist et al. (2012) report that around 75% of instabilities are in the anterior direction, most of them as a result of sports injuries or trauma.
Posterior instabilities make up around 20%, most often due to fits, seizures, or electrocutions, although sports injuries or trauma can play a role here as well.
The remaining 5% of multi-directional instability is most often seen in people with hypermobility.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
It’s important to evaluate the following items in your patient history:
- Age: below or above 25?
- Mechanism of injury: torn (TUPS), worn (AMBRI), or born (muscle patterning / non-structural)
- The direction of instability: anterior, posterior, or multi
- Severity: dislocation or subluxation?
- Frequency: primary or recurrent
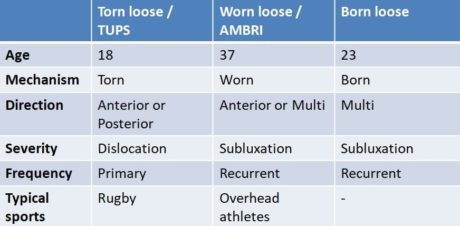
Depending on the answers, you are able to place your patient somewhere on the continuum between the 3 poles as described earlier by Jaggi et al. (2017).
It’s important to realize that psychological components like fear, anxiety and avoidance do play a role and should be evaluated as well.
Examination
After a thorough history that includes onset, circumstances, direction, frequency, and magnitude, the clinical examination is the essential first step in determining the pattern and degree of instability.
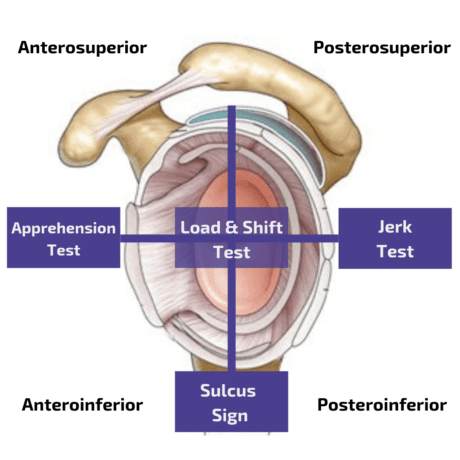
Anterior instability
In order to evaluate anterior instability, a combination of the Apprehension and the Relocation Test yields a sensitivity of 67% with a specificity of 98%, thus basically confirming the presence of anterior structural instability (Hegedus et al. 2012).
The apprehension test is usually directly followed by the relocation test:
An additional orthopedic test that is often performed as a follow-up to the Apprehension and Relocation Test is the Release Test.
Posterior instability
Postereroinferior instability is best assessed with the Jerk Test, which is a very accurate test with a sensitivity of 90% and a specificity of 85% (Kim et al. 2004). The authors also describe that a painful Jerk Test was a predictor of failure of conservative treatment. At the same time, in the painless jerk group (with a positive test due to a clunk) 93% responded to the rehabilitation program after a mean of 4 months.
Other orthopedic tests for posterior instability are:
Inferior instability
In order to evaluate inferior instability, you can perform the Sulcus Test or Sulcus Sign. However, no sensitivity or specificity values are known for this test. At the same time, the test reached only moderate inter-rater reliability with a Kappa value of к=0.43 in a study done by Eshoj et al. (2018).
Another orthopedic test for inferior instability is the Gagey Test. In order to assess multidirectional instability, the Load and Shift Test can be performed.
In case your patient falls into the ‘Born Loose’ category, you should also assess for hypermobility. The Beighton score together with the Brighton Criteria is a method to determine if your patient is suffering from congenital hypermobility syndrome.
TWO MYTHS BUSTED & 3 KNOWLEDGE BOMBS FOR FREE
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
The aim of physiotherapy in the treatment of shoulder instability is to restore pain-free and normal motor control of the affected shoulder by using several distinct techniques that are applied in an appropriate and timely manner suited to the individual patient. Successful treatment is highly dependent upon the correct clinical diagnosis, identification of anatomical structural defects, and abnormal movement patterns so that rehabilitation programs can be designed accordingly (Jaggi et al. 2017).
Shoulder dislocations have high recurrence rates of up to almost 90% in some populations and a low return to activity rate of sometimes below 50%. While surgery seems to be effective in young males who partake in physically demanding sporting activities, Eljabu et al. (2017) report superior outcomes of conservative treatment compared to surgery in many other cases.
The treatment aim in the non-acute setting for shoulder instability is to minimize the risk of recurrence and improve pain and function. Physiotherapy usually starts after 4-12 weeks but can start as soon as the patient can tolerate exercise.
In this video below we will present you with exercise examples for the early and mid-stage rehab and part 2- will show you exercises and drills for late-stage rehab and return to sport. Closed-kinetic chain exercises provide several benefits for patients suffering from shoulder instability: They decrease joint shear and translation, they increase joint proprioception via joint compression and they improve muscle activation.
In part 1 of this video series, we presented closed and semi-closed kinetic chain exercises to rehab shoulder instability in the early and mid-phase of rehab. In the following video we will continue with more advanced closed-chain exercises and open-chain and dynamic drills.
In case your patient is able to tolerate closed and semi-closed kinetic chain exercises, he or she is able to move on to more advanced closed-kinetic chain exercises and open chain perturbations. This is usually the case after around 2 months.
So when do you know if your patient is ready to return to play?
Generally, patients should be able to have a full pain-free range of motion and feel psychologically ready to return to sports. On top of that, strength in all planes should at least be 90% compared to the healthy side. A test that you can use to help guide return-to-play decision-making is the y-balance test for the upper quarter.
At last, proprioception is often reduced in the unstable shoulder when compared to the uninjured side. Shoulder Joint Positioning Sense Assessment can help you to detect and rehab impairments.
Do you want to learn more about Shoulder Instability? Then check out the following resources:
- Physiotutors Podcast Episode 50: The Unstable Shoulder with Anju Jaggi
- Predicting Recurrent Instability of the Shoulder (PRIS) after First-Time Traumatic Anterior Dislocation
- Neuromuscular Exercises for Anterior Shoulder Dislocation
- Short-term effectiveness of high-load strengthening in patients with hypermobile shoulders
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
It’s Time to Stop Nonsense Treatments for Shoulder Pain and To Start Delivering Evidence-based Care
What customers have to say about this course
- Tineke De Vries26/01/25Goede cursus. Goede cursus, gericht op de praktijk Veel geleerd. Met name wat betreft de opbouw van de oefeningenDempsey Thiele02/01/25Overzichtelijk en praktisch! Ik heb de cursus met plezier afgemaakt. Ik denk dat dit een relevante cursus is voor iedere fysiotherapeut die meer inzicht wil krijgen over de huidige evidence omtrent schouder rehabilitatie. Alle informatie wordt overzichtelijk aangeboden.
Ik kan weer kritisch aan de slag mijn patiënten te helpen in de toekomst! - Carlijn Duursma27/12/24Goede cursus Veel verdieping. duidelijke uitleg. misschien wat tekeningen toevoegen voor extra verduidelijking. Veel geleerd.Vanessa Burnet22/12/24Leerzame cursus Opfrissing van kennis wat is weg gezakt.
- Paul Mensink15/12/24Paul Mensink High level literature composed course, videos are perfect examples for used techniques and exercisesFrank Kleyn12/12/24CRSP Ik kan bovengenoemde cursus zeer aanbevelen , nieuwste inzichten , zin en onzin van Subacromiale ruimte , de duidelijke vertaling naar de praktijk en de behandeltafel .
- Marty26/11/24RCRSP CURSUS Niet heel veel nieuws maar wel een goed overzicht en duidelijke uitleg over biomechanica.
Goede filmpjes van Filip en technieken ook goed uitgelegd.
Goede toetsen die de lesstof vrij compleet behandeld..
Website werkt naar mijn mening niet goed. Nogal onoverzichtelijk…
Vergt wat tijd om er mee om te gaan maar voordeel van de cursus is de gunstige prijs per accreditatie punt. Netjes.maria Kramer01/11/24goede cursus voor rcrsp Goede cursus met veel praktische vaardigheden en oefeningen die je direct kunt toepassen, aanrader. - Erik Versluis13/08/24Rotator Cuff Related Shoulder Pain RCRSP by Filip Struijf
State of the art course and very useful for physiotherapists with shoulder expertise or who want to further develop their skills in research and treatment of patients with shoulder complaints. A nice addition is a shoulder case in which you can process the knowledge you have recently acquired.
A major advantage is the possibility to read the course material offered and to watch the video material again.Birgit Schmitz28/04/24Rotator Cuff Related Shoulder Pain RCRSP
Ik vond het een waardevolle cursus met onderbouwd wetenscahppelijk onderzoek dat ondersteunt in mijn praktisch handelen. Ik heb al een nieuwe cursus uitgezocht. 🙂 - Thijs de Jager22/04/24Rotator Cuff Related Shoulder Pain GOEDE RCRSP CURSUS.
Over het algemeen een goede cursus waarbij ik veel ben opgestoken. Goede, evidence based informatie met hier een daar wat uitleg video’s die zeker helpvol waren. Het is ook fijn dat je onder de cursusonderdelen vragen kan stellen en hier een antwoord op kan verwachten van Filip zelf. 4 sterren i.p.v. 5 sterren omdat ik graag meer duidelijkheid en uitleg in video format over de oefeningen had willen zien. Er worden een hoop oefeningen getoond maar het is aan de cursist zelf om te bedenken welke in te zetten in de praktijk.Larson de Neve16/04/24Rotator Cuff Related Shoulder Pain GOOD COURSE
Good theoretical and practical course with exercises that you can immediately use in practice. - Beppeke Molenaar13/04/24Rotator Cuff Related Shoulder Pain OVERALL A GREAT COURSE
This is a very informative and comprehensive course.
Some of the quiz answers that are correct are counted as incorrect, which is a pity.
(Comment Physiotutors: We are currently doing an overhaul of our quizzing system and have fixed this issue now.)Willem Zee28/01/24Rotator Cuff Related Shoulder Pain PRIMA CURSUS!
goed te doen, uiterst praktisch - Jason Pearson11/01/24Rotator Cuff Related Shoulder Pain RCRSP COURSE
Very satisfied with this course. Provides a great framework with which to build your assessment and rehabilitation strategiesMichal Wajdeczko09/01/24Rotator Cuff Related Shoulder Pain Ik ben super blij ermee.
Het was een zeer interessante training. Het cursus was rijk met ge-update informatie, alles wordt volledig en transparant uitgelegd. Ik moet ook toevoegen dat deel van nuttige sets oefeningen briljant is! Veel nuttige tips en combinaties om rotator cuff pijn te kunnen verminderen en alle spieren efficiënt te trainen. Ik ben er trots op dat ik weer mijn kennis en competenties kon ontwikkelen en om mijn patiënten een professionele benadering van schoudercomplexe aandoeningen te kunnen bieden.
Super bedankt!! - Ante Houben30/12/23Rotator Cuff Related Shoulder Pain RCRSP
This course is well designed and based on solid evidence. The information is presented in a structured manner, using text, images and videos to enhance understanding. In addition, I appreciated the course’s emphasis on effectively conveying this information to patients. However, I wished the exercise therapy was more extensive.
Naomi Tiller20/12/23Rotator Cuff Related Shoulder Pain RCRSP COURSE
Fantastic course that’s easy to follow, up to date and evidence based. I’ve immediately been able to implement what I’ve learnt in to my own work which has given me a lot more confidence as well as made it more enjoyable! A good refreshed for me on how the rotator cuff works, a better understanding of how to treat these problems and better communicate with my patients as well as exercise inspiration (always appreciated!). Overall very happy to have done this course!
Super bedankt!! - Stijn de Loof17/12/23Rotator Cuff Related Shoulder Pain GOOD THEORY, LESS EXERCESIS
I liked the theoretical part of the course. A good refresher about the shoulder and rotator cuff with new insights
I was a bit disappointed in the part ‘exercises’. They were super basic and without explinations.Mehdi Benkirane24/11/23Rotator Cuff Related Shoulder Pain REVIEW
Très bon cours, je le recommande pour se remettre à jour sur les tendinopathies de l’épaule.




