Shared decision making in physiotherapy: what, when, how and why?

Chris has a frozen shoulder and is unsure whether he should go to a physiotherapist, go for an injection or wait for improvement to come by itself. Linda rolled her ankle and was told by her physiotherapist that based on the negative Ottawa Ankle rules, no fracture was present and there was thus no need to refer for further imaging, nor for immobilization in a cast. She is surprised as several years ago she also had an ankle sprain and then her doctor recommended going to the Emergency Department for imaging. She wants to better understand why her physio gave this advice and what the pros and cons are of having imaging. These are two examples of the decision-making scenarios faced by patients and their physiotherapists daily. Ideally, in patient-centered care, decisions regarding treatment should be made together. This blog article dives deeper in shared decision making in physiotherapy and answers the questions: what, when, how and why?
What?
Shared decision making is a process in which the patient and his relatives are involved in making decisions about available treatment options and the associated benefits and risks. To be able to be involved in this decision, the best-available evidence, including pros and cons of the options should be discussed. When, how and why should shared decisions be made?
Shared decision making is a process in which the patient and his relatives are involved in making decisions about available treatment options and the associated benefits and risks.
Why?
To begin with the last question, decisions should be made together as this is a way to improve patient satisfaction and as it is an essential part of patient-centered care. Preferences of the patient are discussed and concerns can be addressed. This way, communication between both parties can be improved, resulting in higher satisfaction with care. Next to this, by communicating with your patient, you can get a better idea of what is going on in their mind, and their beliefs and expectations or maybe some misconceptions they have about treatment can be addressed appropriately. By altering their misbeliefs, patients get better informed and this can help to reduce (the demand for) low-value care.
When is making a shared decision appropriate?
In case many different treatment options exist, it may be difficult to choose which way to go. When one option is clearly better than the other, less doubt and uncertainty exists. We certainly know now that bed rest is detrimental in nonspecific low back pain and rather an active approach should be favored. Or we know that imaging someone’s ankle after an acute sprain isn’t necessary if the Ottawa Ankle rules are negative. Unfortunately, in our profession of physiotherapy, it is not usually the case that one approach is clearly better than another. When different options have about the same effectiveness, other factors such as the benefits and harms should be kept in mind. For example, associated costs, the types of benefits and the types of harms can be discussed with your patient in order to enable him to make an informed value judgment.
The Assessment Book – Physiotutors Guide to Orthopedic Physical Assessment
How can this shared decision making come about?
By listening to your patient, and giving space to share thoughts, you can create a ‘safe’ environment where the patient feels free to address their uncertainties and concerns. The figure below discusses the key elements of shared decision making.
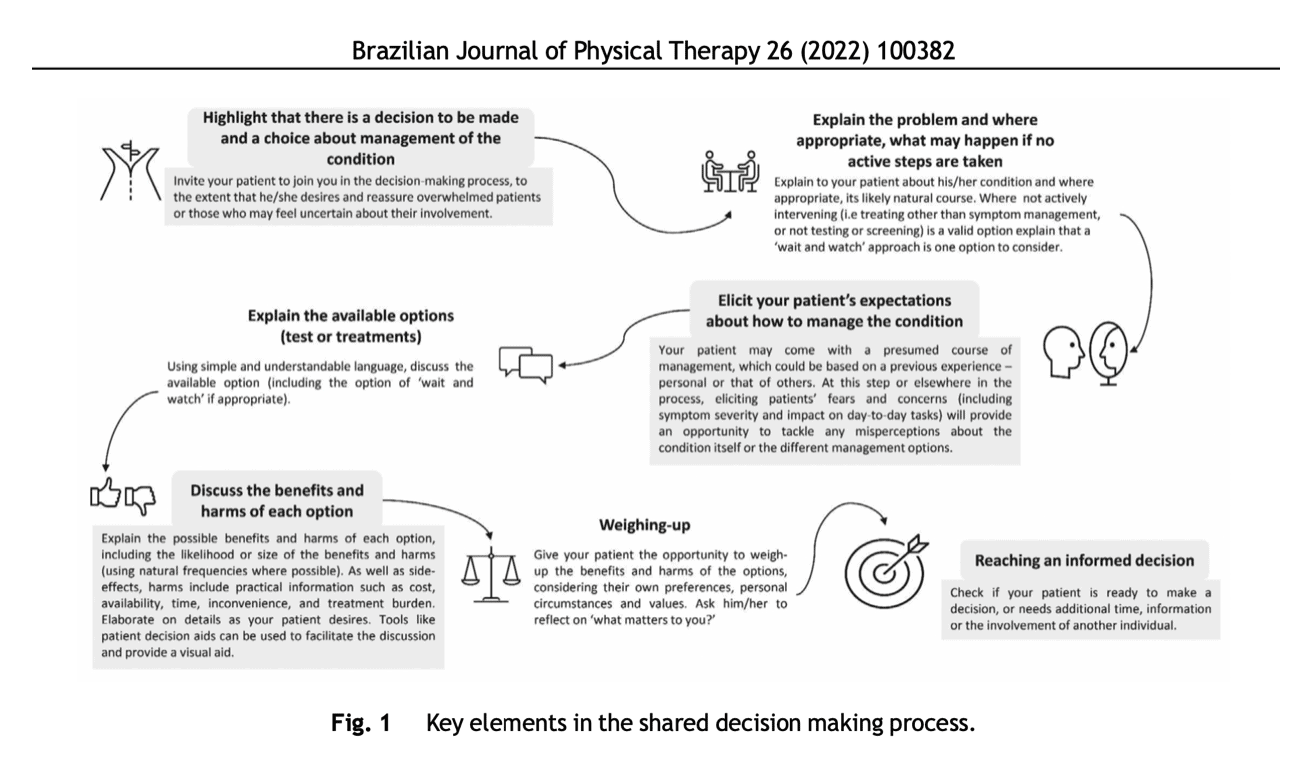
To help with this, you can make use of patient decision aids or option grids, containing information about the condition, treatment options with their pros and cons, and other relevant information such as the associated costs. At the following links, several patient decision aids can be found: https://decisionaid.ohri.ca/AZinvent.php and https://www.med-decs.org/en. Next to this, various websites contain collections of decision aids, such as: Harding Centre for Risk Literacy; UK National Institute for Health and Care Excellence; UK Patient.info; University of Laval decision boxes; Option Grids (subscription through EBSCO Health)
To sum up, shared decision making in physiotherapy requires clinicians to have good communication skills and be knowledgeable in evidence-based practice. Importantly, it appears that the implementation of shared decision making in clinical practice did not lengthen the duration of a consultation, so why wouldn’t you try to improve your care path? We at Physiotutors aim to deliver high quality evidence based content in different formats to help you become an expert physiotherapist. Check out the rest of our website for a ton of relevant information you may use right away!
Reference
Hoffmann T, Bakhit M, Michaleff Z. Shared decision making and physical therapy: What, when, how, and why? Braz J Phys Ther. 2022 Jan 1;26(1):100382. doi: 10.1016/j.bjpt.2021.100382. Epub ahead of print. PMID: 35063699. https://pubmed.ncbi.nlm.nih.gov/35063699/

Ellen Vandyck
Research Manager
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







