Untangling Entrapment Neuropathies: A Comprehensive Overview
This blog post is largely derived from our podcast interview with Dr. Annina Schmid and complemented with scientific evidence. It is by no means a complete overview of the scientific literature on entrapment neuropathies but aims to provide important information to the reaeder. Enjoy reading!
Nerve pain can be as puzzling as it is debilitating, affecting patients’ daily lives and clinicians’ ability to provide clear answers. Among the many types of nerve disorders, entrapment neuropathies hold a prominent yet often misunderstood place. These conditions occur when nerves are compressed, irritated, or stressed as they pass through narrow anatomical spaces. Symptoms often include pain, tingling, numbness, and in some cases, weakness or reduced reflexes. Despite their prevalence, the complexity of these conditions can make them challenging to diagnose and treat effectively.
In a recent Physiotutors podcast, Dr. Annina Schmid, a musculoskeletal physiotherapist and expert in pain neurosciences, shared her vast knowledge about entrapment neuropathies. Her insights not only highlighted the nuances of these conditions but also shed light on current treatment approaches and the exciting research shaping their future. This blog revolves around her discussion during which we explored key aspects of entrapment neuropathies.
What are entrapment neuropathies?
At their core, entrapment neuropathies are conditions where nerves are squeezed or irritated as they travel through narrow spaces in the body. These spaces can be anatomical bottlenecks, like the carpal tunnel in the wrist, or areas affected by swelling or inflammation. While a well-known example is Carpal Tunnel Syndrome (CTS), which involves compression of the median nerve at the wrist, there are many other forms. These include cubital tunnel syndrome, affecting the ulnar nerve at the elbow, and less common conditions like Tarsal Tunnel Syndrome, Morton’s Neuroma, and Thoracic Outlet Syndrome.
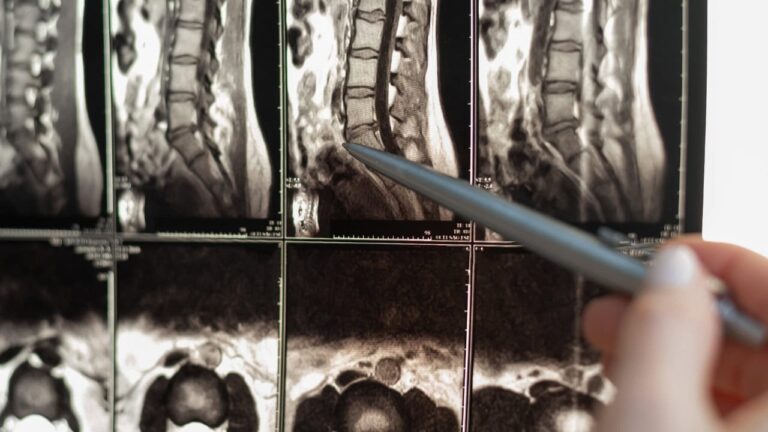
In some cases, entrapment neuropathies arise in the spine, such as in cervical or lumbar radiculopathies. These conditions occur when nerve roots become compressed, often due to herniated discs or degenerative changes in the spine. While these disorders may seem distinct, they share the underlying mechanism of nerve compression or irritation, leading to a variety of sensory and motor symptoms.
The clinical presentation of entrapment neuropathies is as diverse as their causes. Some patients experience mild tingling and numbness, while others may suffer from sharp, radiating pain or significant weakness. In severe cases, nerve entrapment can lead to permanent loss of function, which emphasizes the importance of timely and accurate diagnosis.
The clinical presentation of entrapment neuropathies is as diverse as their causes.
Spaces Where Nerves Get Trapped and/or irritated
The anatomical spaces where nerve entrapment occurs are as varied as the conditions themselves. The carpal tunnel is one of the most common culprits, where the median nerve is compressed as it passes through a narrow channel formed by the carpal bones and the transverse carpal ligament. This condition is particularly common in people who perform repetitive wrist movements, such as typing or manual labor.
Another frequent site of entrapment is the cubital tunnel, where the ulnar nerve runs along the cubital tunnel, a narrow space between the medial epicondyle of the humerus, the arcuate ligament (which joins the two heads of the flexor carpi ulnaris muscle), the olecranon and the ulnar collateral ligament. Like carpal tunnel syndrome, cubital tunnel syndrome often presents with numbness, tingling, and weakness, particularly affecting the little and ring fingers.
Less commonly, nerve entrapment can occur in the lower body. For example, tarsal tunnel syndrome involves compression of the tibial nerve as it passes through the ankle, while Morton’s neuroma affects the plantar digital nerve in the foot. Although they are not very common, these conditions can cause significant pain and functional limitations.There are also controversial conditions, such as piriformis syndrome, which some clinicians argue may not exist as a distinct entity. Piriformis syndrome is thought to involve irritation of the sciatic nerve as it passes near the piriformis muscle in the gluteal area. While some patients report symptoms consistent with this diagnosis, the lack of definitive diagnostic tools and criteria makes it a topic of ongoing debate.
Risk Factors for Entrapment Neuropathies
Biological factors, such as being female, are significant, particularly for carpal tunnel syndrome. Hormonal changes during pregnancy can increase the risk, as can pre-existing conditions like diabetes or hypothyroidism that can lead to systemic neuropathies.
Lifestyle and occupational factors also play a role. Repetitive hand movements, such as those performed by butchers or assembly line workers, increase the likelihood of developing carpal tunnel syndrome. Obesity is another relevant contributing risk factor. The mechanism of how obesity increases the risk of CTS is still unclear.
Genetic predisposition cannot be overlooked. The impact of connective tissue genes is not limited to the spaces surrounding the nerves. Connective tissue is also present inside the nerves themselves, and genetic changes affecting this internal tissue can further increase the nerve’s vulnerability to mechanical exposure and irritation.
Diagnosing and Differential Diagnosis of Entrapment Neuropathies
Distinguishing between a peripheral entrapment neuropathy and a radiculopathy requires careful attention to the patient’s symptoms, history, and clinical findings. Several key factors can help differentiate these conditions:
- Onset of Symptoms
Peripheral entrapment neuropathies often have a gradual onset, developing slowly over time. Patients may struggle to pinpoint when their symptoms began, describing a progressive increase in tingling, numbness, or pain.
In contrast, radiculopathies, such as those caused by nerve root compression in the cervical or lumbar spine, often present with a more acute onset. Patients may recall a specific event or moment, such as lifting a heavy object, that triggered their symptoms. - Laterality
Peripheral entrapments, such as carpal tunnel syndrome, frequently occur bilaterally, affecting both hands or wrists. While radiculopathies can present on both sides, it is much less common. - Aggravating and Alleviating Factors
Specific movements or positions can provide clues:- Shaking the hands often changes the symptoms of carpal tunnel syndrome but does not influence the symptoms of cervical radiculopathy.
- Raising the arm overhead may alleviate symptoms of cervical radiculopathy (e.g., C7 root), but this position typically has no effect on upper limb entrapment neuropathies.
- Provocation Tests
Different physical tests can provoke symptoms depending on the location of the nerve compression:- For cervical radiculopathy, positions of the neck, such as those in the Spurling test, can exacerbate symptoms.
- For peripheral entrapments, movements or positions involving the wrist, elbow, or other specific anatomical areas, such as Phalen’s test for CTS, are more likely to reproduce symptoms.
- Nerve Palpation
Palpation of the nerve can be particularly helpful for distal entrapment neuropathies. For example, palpating the ulnar nerve in the cubital tunnel may reproduce symptoms in cubital tunnel syndrome. In radiculopathies, nerve palpation is less likely to provoke pain or other symptoms. - Neurological Deficits
If weakness or sensory loss is present, the distribution of these deficits can be a critical differentiating factor:
Peripheral nerve entrapments cause deficits in the specific territory of the affected nerve. For instance, a median nerve entrapment would lead to sensory and motor changes in areas innervated by the median nerve. Radiculopathies, on the other hand, result in deficits following a dermatomal or myotomal pattern corresponding to the affected nerve root. An example of case-specific differentiation between peripheral nerve problems or C8 radiculopathy is outlined below:- Assess the Neurological Deficits
Begin by testing muscles that share the same nerve root (C8) but are innervated by different peripheral nerves. If you find weakness, always compare with the muscles of the contralateral limb for baseline testing. If the flexor pollicis (median nerve) or the abductor digiti minimi (ulnar nerve) are weak along with the extensor pollicis longus, it is likely a C8 nerve root issue, as all these muscles share C8 innervation. - Evaluate Peripheral Nerve-Specific Muscles
To determine if the problem is specific to the radial nerve for example, test muscles innervated by the ulnar nerve but not involving C8 and again, compare with the contralateral limb for baseline. For example, the brachioradialis muscle is innervated by the radial nerve but not by a C8 nerve root. If these muscle is weak, while muscles innervated by C8 nerve root and the ulnar (abductor digiti minimi) or median nerve (flexor pollicis) show normal functioning, this strongly suggests a radial nerve problem rather than a C8 root problem. - Assess Sensory Distribution
The sensory exam can also help clarify the diagnosis in the case of sensory loss. A C8 nerve root issue may cause sensory loss in the ulnar aspect of the forearm, extending into the ring and little fingers. In contrast, a radial nerve problem would produce sensory loss in the dorsal aspect of the forearm and into the dorsum of the hand.
- Assess the Neurological Deficits
- Diagnostic Tests
Advanced diagnostic tools, such as MRI and electrodiagnostics, are useful tools for confirming the diagnosis in complex cases. MRI is useful for identifying structural changes in tissues provoking neuropathies, while nerve conduction studies can assess the functional status of the affected nerves.ars and it commonly accompanies them throughout their productive years. This timing poses a significant challenge, as migraines are predominantly experienced when individuals are often focused on careers, work, and raising children. After reaching this peak, many people experience a gradual decline in the frequency of migraines as they age, especially women, who may notice a reduction in migraine occurrences around menopause.
Reliability of Dermatome Testing
Dermatomes, or the sensory areas innervated by specific nerve roots, are often used to guide diagnosis. However, their reliability depends on whether the neuropathy is leading to a loss of function or a gain of function.
In cases of loss of function, such as numbness, dermatomes are highly reliable in determining the sensory level affected. For example, a patient with an L5 nerve root problem may have weakness in extending the big toe and sensory deficits in a characteristic pattern, typically tested on the dorsum of the foot near the MTP2 joint.
Conversely, dermatomes are less reliable for gain of function symptoms, such as tingling or pain. Research shows that up to two-thirds of patients with radiculopathy have symptom distributions that do not align with textbook dermatome maps in the case of function gain.
Treatment Approaches
Treatment for entrapment neuropathies is as varied as the conditions themselves. Conservative management is often the first line of treatment, particularly for mild to moderate cases. However, close monitoring and paying particular attention to worsening symptoms is highly advised, as in these cases more drastic interventions (such as decompression surgery) might be justified to avoid severe nerve damage.
Neurodynamic exercises, such as nerve gliding techniques, are widely used to improve nerve mobility and reduce symptoms. Studies have shown that these exercises can reduce nerve edema and inflammation, particularly in conditions like carpal tunnel syndrome. Releasing the tissue potentially causing the entrapment is recommended prior to nerve mobilisations, although this is often not possible due to the location or the nature of the tissue causing the nerve compression.
Splinting is another effective strategy, especially for carpal tunnel syndrome. By keeping the wrist in a neutral position, splints can prevent adopting positions that add pressure to the median nerve and provide relief from symptoms.
In cases of neuropathic pain, pharmacological interventions may be necessary in more severe cases. Medications like gabapentin or pregabalin can help manage pain, particularly when conservative treatments fall short.
Surgery is reserved for severe cases, such as those involving significant neurological deficits or intractable pain. Procedures like carpal tunnel release or decompression surgery can relieve pressure on the affected nerve and prevent further damage.
Can Nerves Regenerate?
The question of nerve regeneration is central to understanding the long-term prognosis of entrapment neuropathies. While nerves can regenerate to some extent, the process is slow and often incomplete.
Research by Dr. Schmid and her team has shown that chronic nerve compression can limit the nerve’s ability to fully reinnervate affected areas. For example, in patients with long-standing carpal tunnel syndrome, surgery can relieve symptoms but may not restore full nerve function or only very slowly.
Interestingly, studies on chronic entrapment neuropathies, such as Morton’s neuroma, have revealed persistent low-grade inflammation in the affected nerves, with an inflammation different to that experienced in e.g. muscles. This finding suggests that traditional anti-inflammatory treatments may be insufficient and highlights the need for new approaches, such as pharmacological strategies that, instead of suppressing it, would turn the inflammation into a pro-resolving one.
Emerging Research and Future Directions
The future of entrapment neuropathy diagnosis and treatment is promising, thanks to advances in imaging and precision medicine. Ultra-high-field MRI and MR neurography are paving the way for more accurate diagnostics by allowing clinicians to visualize nerves in unprecedented detail. These techniques are particularly valuable for identifying subtle changes in nerve structure that may not be visible with traditional imaging.
Deep clinical phenotyping is another exciting area of research. By using advanced imaging, biopsies, and neurophysiological tests, psychosocial factors, etc., researchers are identifying subgroups of patients with different presentations (e.g. mechanosensitivity vs. sensory loss) of the same condition. This approach could lead to more targeted treatments and better outcomes for patients.
Take this Masrterclass for free now!
Watch this free Masterclass with wrist and hand specialist physiotherapist Thomas Mitchell exclusively on the Physiotutors App

References
Silver, S., Ledford, C. C., Vogel, K. J., & Arnold, J. J. (2021). Peripheral Nerve Entrapment and Injury in the Upper Extremity. American family physician, 103(5), 275–285.
Zvonickova, K., Rhee, A., Sandy-Hindmarch, O., Furniss, D., Wiberg, A., & Schmid, A. B. (2024). Systemic low-grade C-reactive protein is associated with proximal symptom spread in carpal tunnel syndrome. Pain reports, 9(3), e1156. https://doi.org/10.1097/PR9.0000000000001156

Anibal Vivanco
Physiotherapist, content creator
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







