Pain in the butt – Why It’s not Piriformis Syndrome

If you or your patients feel pain deep in the butt, there’s a good chance that they will end up with the diagnosis of piriformis syndrome. In this blog post, we will explain why it’s NOT piriformis syndrome 99% of the time, what the actual causes might be, and especially what to do about it!
Prefer watching a video rather than reading? Then check out our video on this topic:
Background
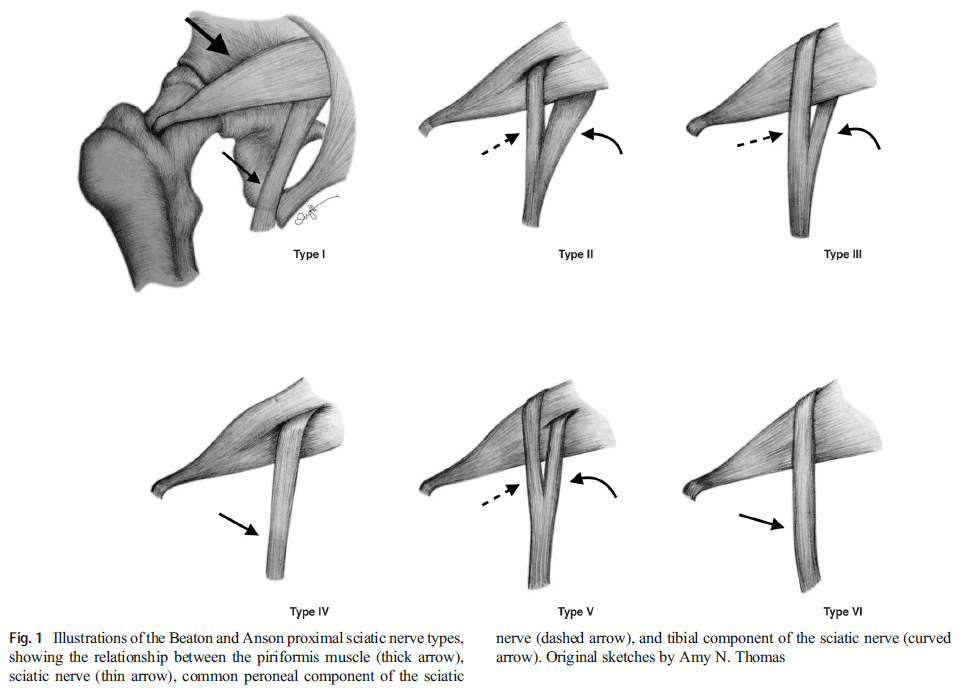
The piriformis muscle runs from the sacrum to the hip joint. Due to the fact that the sciatic nerve runs underneath it, it was suggested that a tight piriformis might compress the sciatic nerve and cause pain in the buttock and the back of the leg. Researchers have even found anatomic variations where the sciatic nerve runs directly through the muscle, leaving the sciatic nerve even more susceptible in theory.
There are more anatomic structures than the piriformis that could potentially compress the sciatic nerve. Therefore, the term “deep gluteal syndrome” is now preferred.
However, there are more anatomic structures that could potentially compress the sciatic nerve like the Gemelli-obturator internus complex, the hamstring muscles, fibrous bands containing blood vessels, vascular abnormalities, and space-occupying lesions. For this reason, experts now prefer the term “deep gluteal syndrome”.
Independent of how we want to call it, why do we say that it’s not piriformis syndrome then? Here are 3 strong arguments:
1. A study by Barret et al. (2018) examined 1039 adult hips on MRI of which around 20% had sciatic nerve variants that might make the sciatic nerve more susceptible to compression by the piriformis muscle.
They found no relationship between sciatic nerve variants and piriformis syndrome.
2. Piriformis syndrome by definition is the compression of the sciatic nerve by the piriformis muscle. When a nerve gets compressed and irritated, patients report symptoms like pins & needles or a loss of feeling and strength in the distribution of that nerve. Nerve pain usually has a burning, electric, or shooting quality – most people that we see in practice only have deep, aching buttock pain and no symptoms distal to the buttock and referred pain to the posterior thigh at most.
So if the pain stays in the buttock area and has a quality different from nerve pain, how can the sciatic nerve be affected?
3. In patients that do actually suffer from real sciatica, only 6-8% are thought to have piriformis syndrome. This means that in the vast majority of cases, there will be different underlying reasons for sciatica, mainly nerve root compression due to lumbar disk herniations or foraminal stenosis.
Only 6-8% of patients suffering from real sciatica are thought to have piriformis syndrome
In many regards, the diagnosis of piriformis syndrome in the lower limb is comparable to thoracic outlet syndrome in the upper limb. The diagnosis makes sense from an anatomical point of view, but both are a diagnosis of exclusion and are highly debated by experts in the field. In patients that do undergo medical imaging or surgery, most cases turn out to be caused by nerve root compression.
Diagnosis
So how can we perform a structured diagnosis for piriformis syndrome?
First, make sure that your patient also suffers from symptoms of nerve root compression, so he or she describes pins & needles, burning, possible loss of feeling and strength, or shooting pain in the distribution of the sciatic nerve which runs all the way down the backside of the leg into the foot.
If this is the case, you first need to rule out lumbosacral radicular syndrome. Check out our playlist with videos that can help you with that by a click on the info button in the top right corner.
After ruling out radicular syndrome, we would continue with provocation tests that stretch or contract the deep gluteal muscles in an attempt to elicit sciatic nerve pain.
Of course, we have an extensive list of provocation tests for piriformis syndrome on our channel as well.
In case your patient only reports buttock pain, there can be a huge variety of underlying pathologies making a diagnosis very challenging. Here’s an overview by Gomez-Hoyos et al. (2018) with possible underlying reasons for posterior hip/buttock pain:
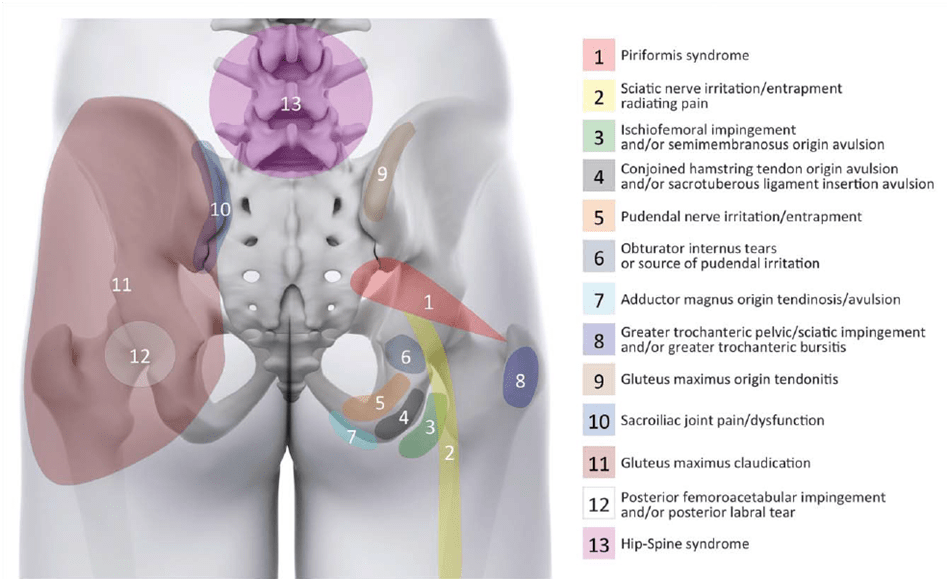
Our first priority would be to examine the lumbar spine which commonly refers pain into the buttock area. The sacroiliac joint can be a driver of nociception as well. The cluster of Laslett can be helpful in making this diagnosis more or less likely. For the other diagnoses, you can find videos on our channel.
Now let’s move on to what we most commonly see in practice, which is muscle pain in the deep gluteal area, also called myofascial pain.
A way to confirm this diagnosis is to have the patient stretch and contract the deep external rotators of the hip, which should elicit symptoms deep in the buttock.

Furthermore, manual palpation of the deep gluteal area should elicit recognizable pain by the patient. Make sure to compare both sides as basically everyone will report pain if you just poke hard enough.
So what is the reason that muscles become painful?
Like mentioned in earlier videos, in most cases muscles become tight, because they are weak and the demand placed on them is higher than their capacity. Be aware that psychosocial and environmental factors can also have an influence on the patient’s pain experience. So a patient’s pain threshold could be lowered by stress, lack of sleep or decreased sleep quality, anxiety, depression, etc.
Orthopedic Physiotherapy of the Upper & Lower Extremities
Boost Your Knowledge about the 23 Most Common Orthopedic Pathologies in Just 40 Hours Without Spending A Fortune on CPD Courses
Treatment
There is quite a variety of options targeted at short-term pain relief like manual pressure and massage in the painful area, dry needling, heat, and rolling with a foam roller or tennis ball.
Another short-term option is to stretch the deep gluteal muscles. Here are 2 stretches that you might want to try at home:
- Standard piriformis stretch in sitting or supine
- Yoga Pose

While those are all “optional”, our recommendation for short-term pain relief is to decrease activities that are aggravating your buttock pain.
Avoid prolonged sitting or standing and try to change positions as often as possible as our muscles don’t like static postures. Sitting on a well-cushioned pillow can make sitting a bit more bearable and having a pillow between your legs when you’re lying in bed can reduce prolonged stretch on the gluteal muscles.
If running or walking is painful, temporarily decrease your running or walking volume to tolerable levels.
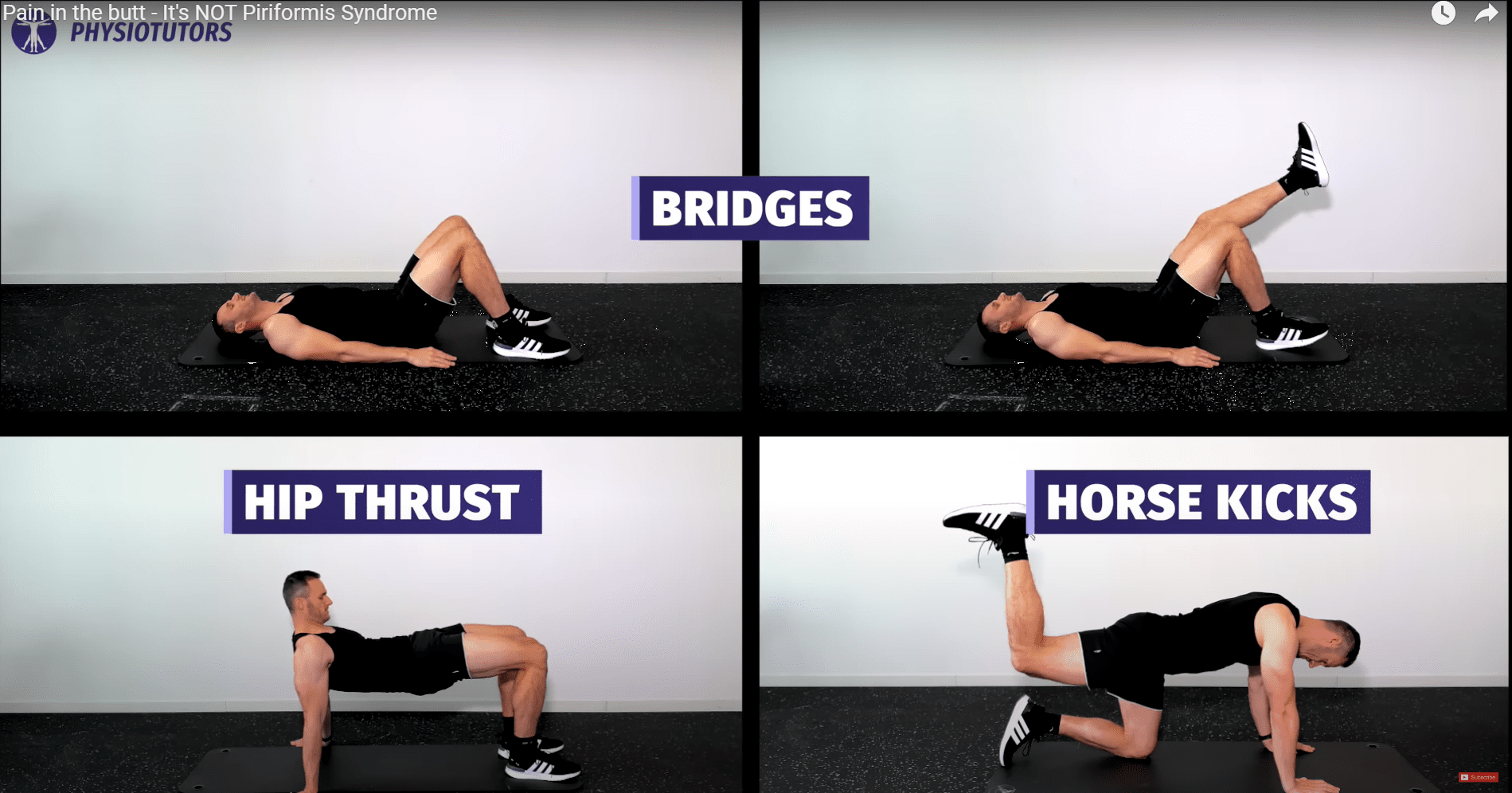
As mentioned in other videos, the only real long-term solution to muscle pain is a progressive exercise program that targets the painful area. With all exercises, make sure that pain levels are tolerable during the program. If pain increases afterward, make sure the pain settles within 24 hours. If this is not the case, try easier exercises or decrease the number of sets and reps.
Here’s an example of a progressive exercise program starting from easy to more advanced exercises:
- Clam Shells 🡪 Add resistance bands 🡪 side plank clamshell
- Fire hydrants in sitting 🡪 quadruped🡪 standing with resistance band
- Glute bridges 🡪 1 legged
- Horse kicks
If these exercises are tolerable, you can move on to heavier more global exercises such as
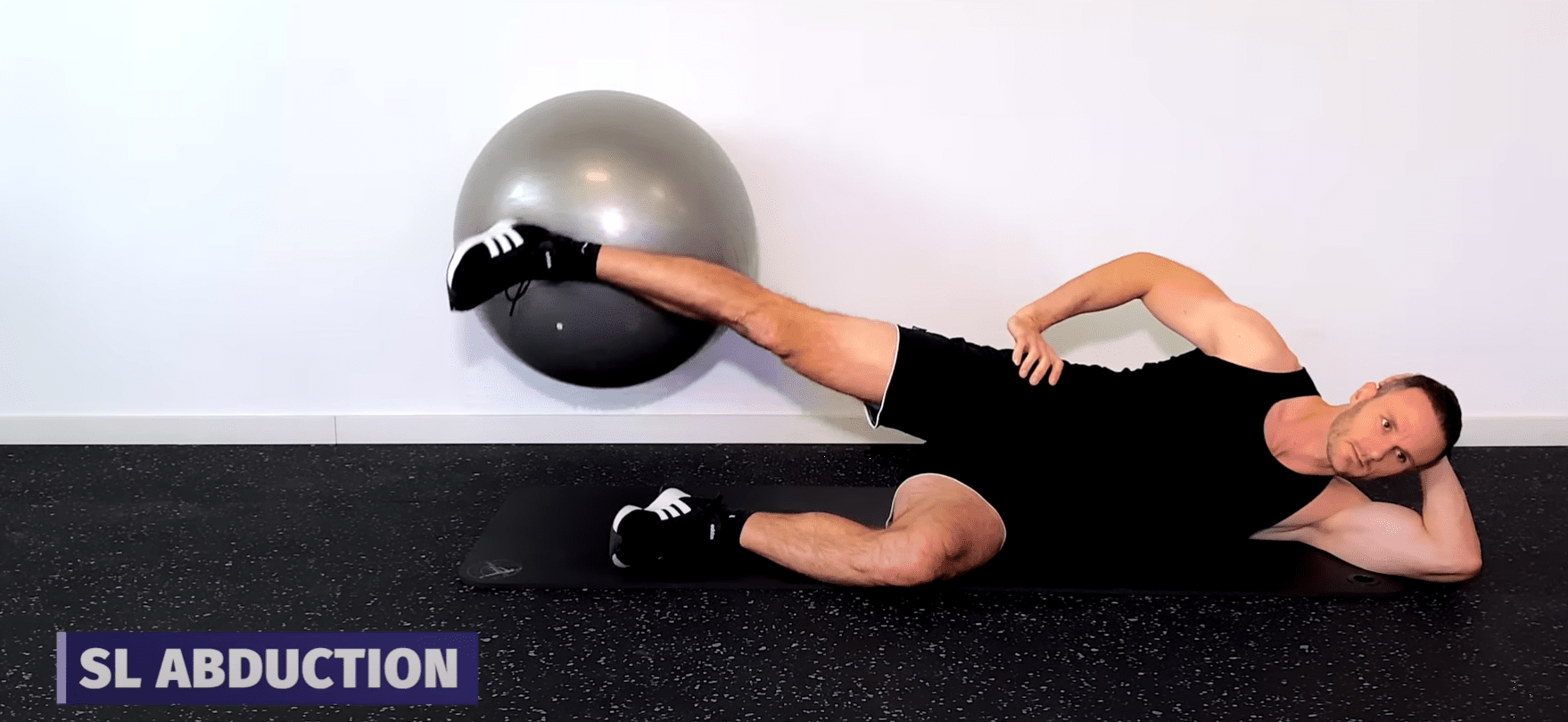
- Side lying abduction with the ball against the wall (see above)
- Leg Presses
- Squats
- Hip thrusts
Okay, this was our video on “pain in the butt” and why it’s not piriformis syndrome in 99% of the cases. Most cases can be treated effectively with a progressive strengthening program. Try it out with your patients and let us know if this works for you as well as it does for us!
As always, thanks a lot for reading!
Kai
References

Kai Sigel
CEO & Co-Founder of Physiotutors
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







