The Frozen Shoulder Guidelines: Frozen in Time?
The treatment of a frozen shoulder is based on a 2013 guideline. Is this guideline still up-to-date? Or did new evidence emerge?

Welcome to our in-depth blog post on recognizing and treating the frozen shoulder. Different treatments exist, and this blog post will examine the main advice and supporting data for this difficult situation.
Introduction
Frozen shoulders are recognized as one of the most challenging conditions. Contrary to the misconception that they will resolve independently without intervention, these conditions often require careful management and intervention. In this post, we will delve into the diagnosis and management strategies for frozen shoulders.
More of a listener than a reader?
You can watch the filmed version of this post here.
Diagnosis and Key Characteristics
Risk Factors
Frozen shoulders can affect individuals of various age groups and backgrounds, but several risk factors increase the likelihood of developing this condition.
Primary adhesive capsulitis affects 2-5% of the population, and secondary capsulitis due to thyroid disorders or diabetes has a prevalence of a whopping 4–38% percent, which is exceptionally high. Make sure you’re on full alert when a patient with shoulder pain steps into the clinic with comorbidities such as these.
There are a few other risk factors. Patients with a history of Dupuytren’s disease are also at increased risk. If you’d like to know more about Dupuytren’s disease, check out our guideline video here.
“The 50-year-old shoulder.“
In Japan, they call it the 50-year-old shoulder, which directly informs us of another risk factor: age. Rarely will you see a patient with a frozen shoulder younger than 40 years old or older than 65 years old. The peak incidence lies between 50 and 56 years of age.
The guidelines state that females are more often affected than men; however, some authors call this into question (e.g., Lewis 2015). A history of a previous frozen shoulder should be considered a risk factor too. There is a 5–34% chance that the pathology reoccurs contralaterally.
Other risk factors include prolonged immobilization after surgery, a myocardial infarction, trauma, and autoimmune diseases.
Clinical Presentation
Frozen shoulders often present with gradual stiffening and increasing pain over time. External rotation and abduction are primarily the affected movements. The restrictions are observed in both active and passive movements.
Frozen Shoulder Phases
The condition progresses through several proposed phases:
The early phase is characterized by sharp pain with movements, achy pain at rest, and sleep disturbances.
The second and third phases involve a loss of motion in all planes and can last up to several months. Histologically, there is a difference between the two, but not clinically.
The fourth phase is when pain decreases, but stiffness can persist for up to 24 months.
Nevertheless, after two years, not all patients will be symptom-free. The typical length of a frozen shoulder is 30 months, but 50% of individuals continue to experience mild to moderate disabilities years after the condition first manifests (Shaffer et al. 1992)
Misdiagnoses & Differential Diagnoses
As mentioned before, one of the pitfalls is misdiagnosis in the early stages. This phase is critical since a corticosteroid injection can alleviate a lot of pain and will, according to the most recent guidelines, not be administered with a (wrongful) diagnosis of subacromial shoulder pain (Lafrance et al. 2022). So getting the diagnosis right is crucial for the treatment choices for a frozen shoulder.
Let’s make sure you won’t miss the next one. There is a boatload of differential diagnoses to consider: acute calcific tendonitis/bursitis, arthrosis of the shoulder, cervicalgia, cervical disc disorders, contusion of the shoulder and upper arm, diseases of the digestive system, fractures, impingement syndrome of the shoulder, TOS, avascular necrosis, labral lesions, suprascapular nerve entrapment, neoplasm, AC OA, Cx OA, cervical radiculopathy, long head of bicep tendinopathy, rotator cuff tears,…
New Evidence Emerged
The patient’s history and your clinical exam will be crucial in your diagnostic process. The most common shoulder complaint is subacromial shoulder pain or rotator cuff-related shoulder pain. These umbrella terms encompass some of the diagnoses in the previous list. The frozen shoulder guideline is a bit dated, and new evidence has emerged. The more recent rotator cuff-related shoulder pain guidelines consider tendinitis, bursitis, impingement, partial tears, and long head of bicep tendinopathy all the same diagnosis. This makes the list at least a tad shorter. We have covered these guidelines as well, so if you’re interested, click below.
Presentation of the Frozen Shoulder
The general presentation is an increase in pain and stiffness over time. The inflammatory process will cause a lot of pain at night, with sleep disturbances as a consequence. As stated before, the loss of ROM is both active and passive.
Diagnose the Frozen Shoulder
To put it in numbers, you need a 25% decrease in two planes of motion and a 50% decrease in passive external rotation compared to the uninvolved side. Having less than 30° of external rotation will count toward the diagnosis as well. Special tests are not helpful for the diagnosis.
Treatment
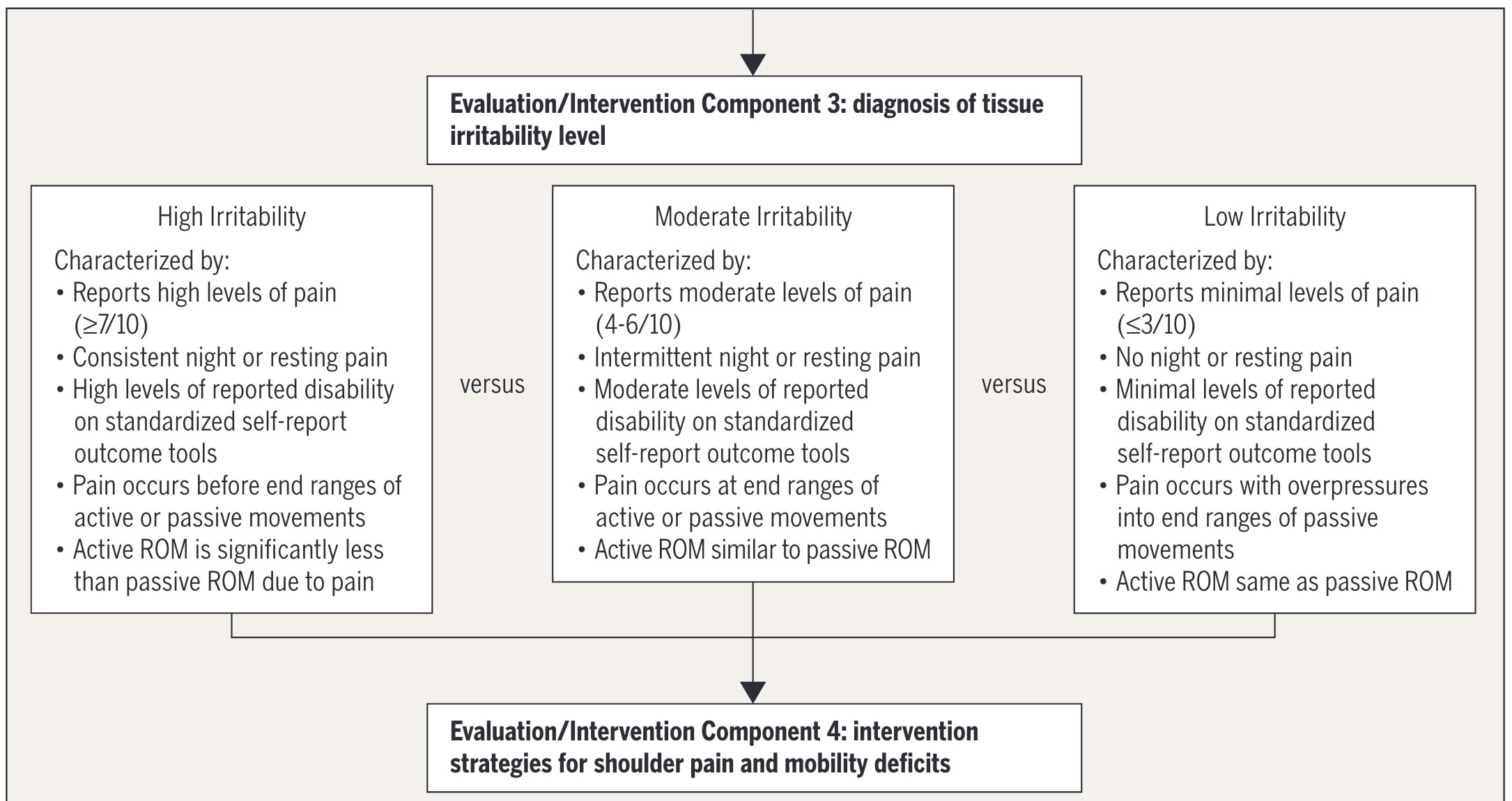
The level of tissue irritability helps categorize patients into high, moderate, or low irritability groups. This classification informs the choice of treatment options.
Treatment Approaches for Frozen Shoulders
Multiple treatment options for the frozen shoulder exist. But what is effective?
Patients should be educated about the natural history of frozen shoulders and the importance of modifying their activities to encourage a pain-free range of motion.
Intra-articular steroid injections, combined with shoulder mobility and stretching exercises, have the strongest recommendation for short-term pain relief.
Stretching exercises should be tailored to the level of irritability (Kelley et al. 2013).
Other forms of exercise, such as mobility or resistance training, can be considered but are often more effective when combined with a steroid injection (Challoumas et al. 2020).
Additional Modalities
Some additional modalities to consider include short-wave diathermy, ultrasound, or electrical stimulation combined with mobility and stretching exercises. However, it’s worth noting that the evidence supporting these modalities is not particularly strong, and more recent trials—since the guidelines—have raised questions about their effectiveness (Ebadi et al. 2017, Tugce Onal et al. 2018, de Sire et al. 2022, Hanchard et al. 2012).
Glenohumeral joint mobilizations can help decrease pain and increase the range of motion. However, they may be less effective in the first few weeks or months, likely due to the highly active inflammatory process during this phase (Page et al. 2014).
Assess Progress
It’s crucial to regularly assess your patient’s progress using questionnaires to evaluate pain and function before and during treatment. Questionnaires you can use are: SPADI, DASH, and the ASES.
Conclusion
In conclusion, frozen shoulders are a complex condition that requires careful diagnosis and management. While there is no definitive treatment for the frozen shoulder, a combination of education, intra-articular steroid injections, and tailored exercises can provide substantial relief. Remember that every patient’s experience with a frozen shoulder is unique, and treatment should be adjusted accordingly. More high-quality trials are definitely needed in this dated field.
Thanks a lot for reading!
Max
References

Max van der Velden
Research Manager
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







