Rhomboid Pain / Pain between the Shoulder Blades – What is it and how do we “fix” it?

If you’re working as a musculoskeletal physio, there’s a good chance that you’ll see at least 1 patient a day coming in with pain between the shoulder blades. But what is causing this pain? Is it the neck? Is it the upper back? Is it posture? Or Is it trigger points and muscle tightness? In this blog, we will explain how to get to the bottom of medial scapular or rhomboid pain and show you how to treat it.
Prefer watching instead of reading? Check out our video below:
Don’t fall for the “quick fix”
If you’re a practitioner or patient looking for solutions for pain between the shoulder blades, you’ll find plenty of different suggestions on social media. There is one camp that claims that medial scapular pain is coming from the lower cervical area, another one claiming that it’s the thoracic joints and limited thoracic mobility, and a third camp that focuses on the rhomboid muscles directly.
But how do you know who is right and could it be one or the other in different patients?
There is no singular cause of rhomboid pain. Make sure to conduct a thorough examination!
Referred pain from the neck/cervical area
There is indeed a great amount of literature (Slipman et al. 2005, Dwyer et al. 1990, Cloward et al. 1959) showing that the cervical intervertebral disks at C4/C5 and lower, as well as the facet joints, can all refer pain to the area medial to the scapula.
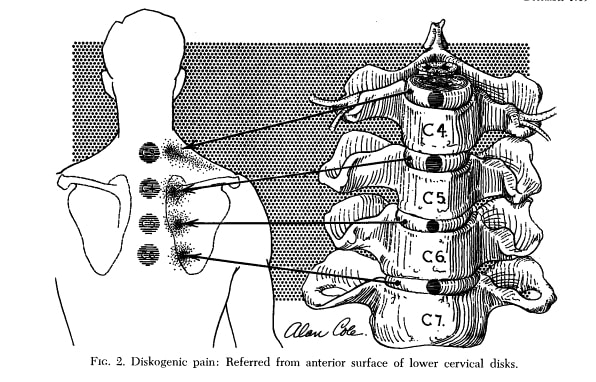
But can we as therapists make it more or less likely that the origin of interscapular pain is coming from the neck? If you have watched our video on referred pain, you know that the referred pain often starts as local pain in the spine and if pain persists, spreads to an area distally. So in case interscapular pain is referred from the neck, you would expect a history of neck pain, concomitant neck pain, and an association between the degree of neck pain and medial scapular pain. Furthermore, referred pain is often aching and diffuse in nature in contrast to local pain which is often sharp or stabbing and well localized.
Third, a nociceptive stimulus at the cervical area should refer pain to the rhomboids. A way to examine this is by performing PA pressure on the cervical levels C4 and lower. If you’re a manual therapist, you would want to perform PIVMS in 3D extension with the goal of eliciting an increase in pain in the interscapular area.
To summarize, rhomboid pain coming from the cervical area is likely if:
- The patient also has neck pain or a history of neck pain
- Interscapular pain increases with increasing neck pain or decreases when neck pain decreases
- Provocative maneuvers like PA pressure or PIVMs in the lower cervical area elicit or increase pain in the rhomboid area
If your suspicion of referred pain from the neck was confirmed, you can directly move on to treatment. Cervical manipulation and mobilization can often provide instant, but often only short-term pain relief.
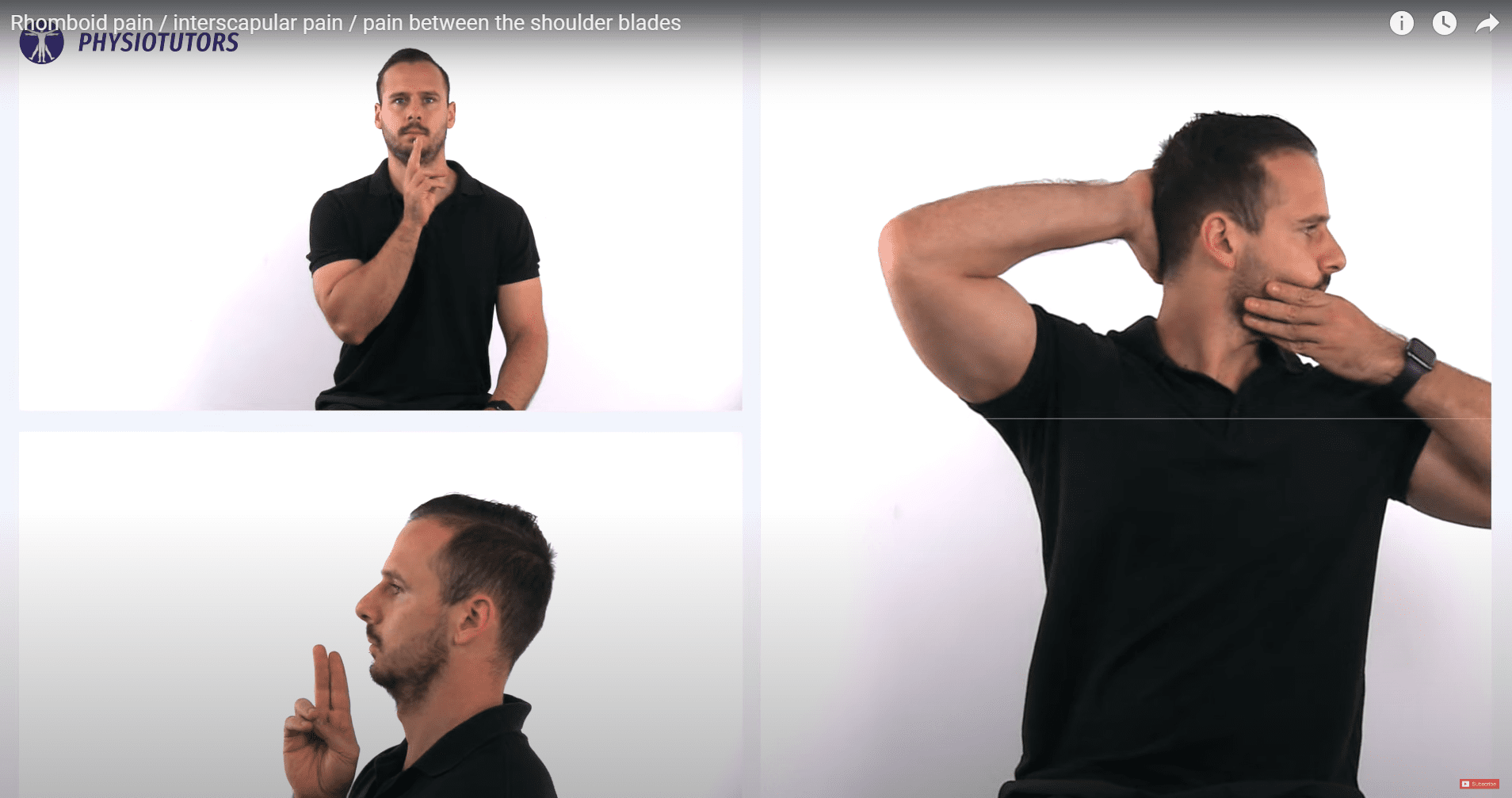
For this reason, it’s important that the patient performs self-mobilizations of the cervical area up to several times per day at home or at work, such as:
- Retraction of the cervicothoracic spine
- Rotation of the cervical spine
- In case the patient remains in provocative postures for a prolonged period, the following exercises might provide relief and can be done as active workplace breaks:
Advise the patient that there is no clear link between posture and pain in the scientific literature, but that remaining in static prolonged posture can be a contributor to muscle pain. Therefore, patients should try to change their posture frequently and use the aforementioned exercises as movement breaks.
Thoracic referred pain
Now let’s examine if the pain might be coming from the thoracic spine. The story here is very similar to what we just mentioned about referred pain from the cervical spine. Studies by Dreyfuss et al. (1994) and Young et al. (2008) show that referred pain from the thoracic facet joints and costotransverse joints refer pain laterally. So basically the whole upper and midthoracic area can potentially refer pain medial to the scapula.
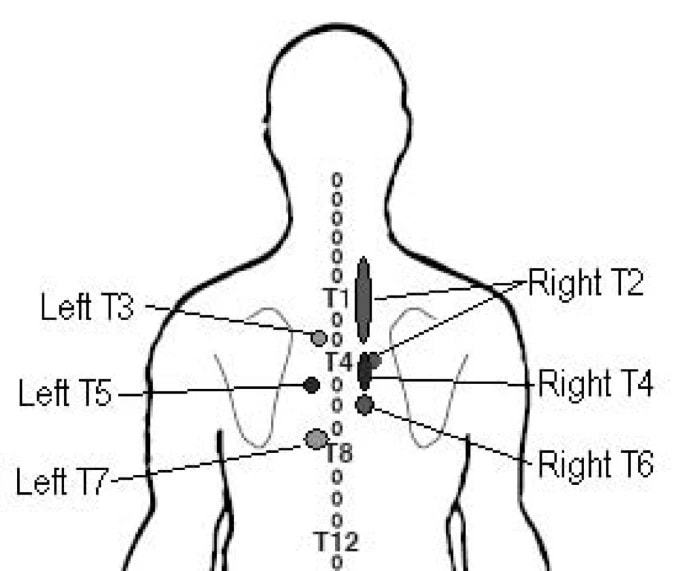
If this hypothesis is likely, we would expect a history of thoracic pain, current thoracic pain, an association between thoracic pain and medial scapular pain and we can try to provoke rhomboid pain by manual examination.

Again, you can either perform PA pressure centrally or unilaterally to the facet joints and/or costotransverse joints. Another option are PIVMS in the direction of 3D extension with the goal of eliciting or increasing interscapular pain.
If your suspicion of referred pain from the thoracic spine was confirmed, you can consider the following treatment options. As mentioned in the cervical spine, cervicothoracic and/or thoracic manipulation and mobilization can often provide instant, but often only short-term pain relief.
There are plenty of mobilization exercises for the thoracic spine that patients can perform themselves several times a day.
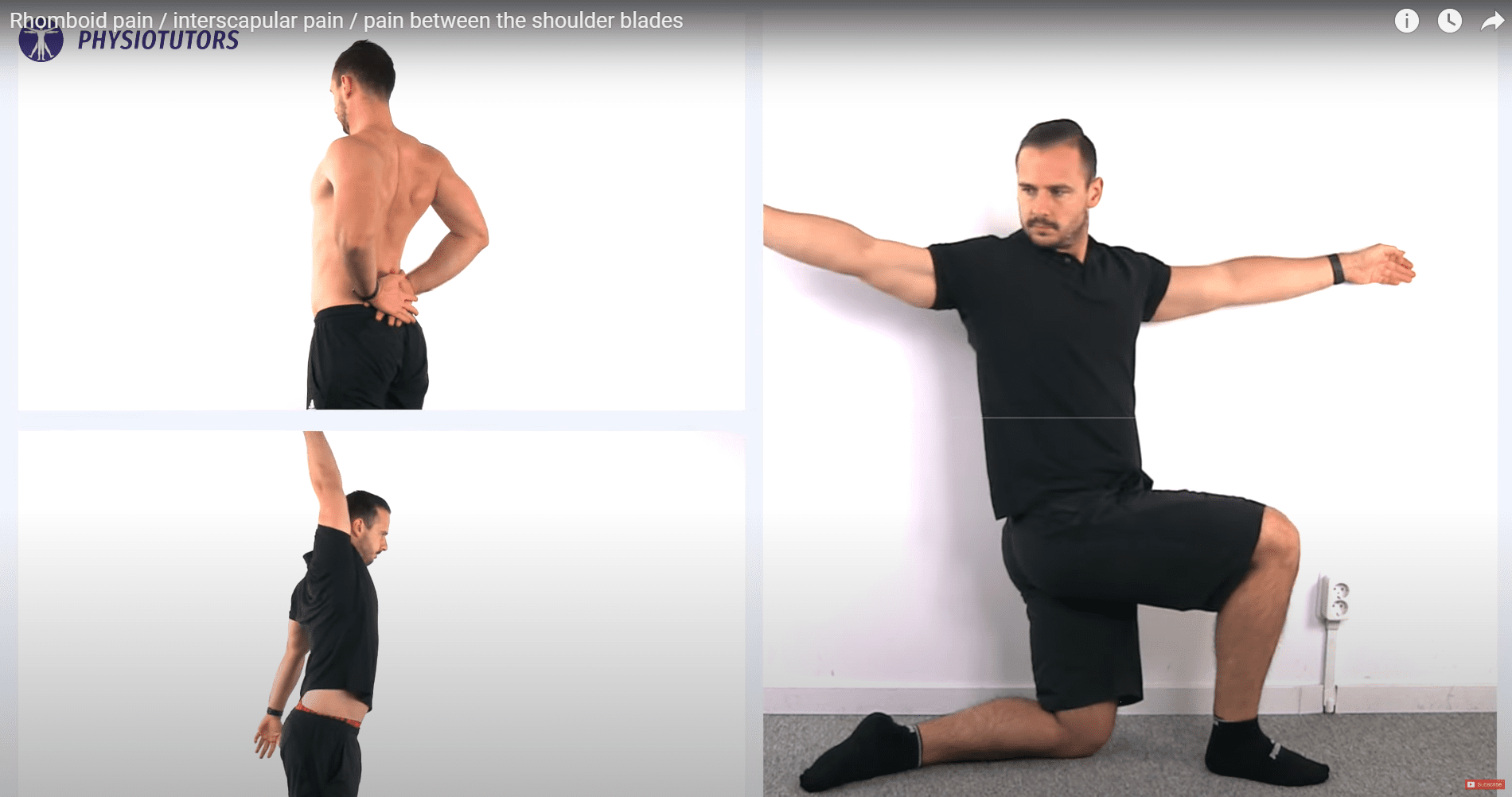
Here are 3 examples:
- Windmills for the cervicothoracic spine
- Rotation in side-lying or against the wall for thoracic rotation
- Scapula adduction
Again, advise the patient to regularly change posture and use the exercises as movement breaks at work.
Orthopedic Physiotherapy of the Spine
Master Treating the Most Common Spinal Conditions in Just 40 Hours
Local muscle pain and trigger points
So you’ve examined the cervical spine and the thoracic spine, but you haven’t found these areas to be the culprit of rhomboid pain? Then there’s a good chance that your patient is having local muscle pain. In contrast to referred pain, local muscle pain is often described as sharp and well-localized. Unfortunately, the phenomenon of trigger points can also be responsible for referred, diffuse and aching pain, which can make a differential diagnosis more difficult.
To make the hypothesis of local muscle pain or trigger points more likely, you can palpate the rhomboids and adjacent muscles in the interscapular area for sore spots. Make sure that you are reproducing the patient’s recognizable pain because you can find tender spots in basically all asymptomatic patients as well.
So what can you and your patient do in case the pain is likely of muscular origin?
There is a broad range of options for short-term pain relief that are worth a try:
- Trigger Point Treatment with your thumb or dry needling
- Tennisball: Yes, this does help quite a few patients in the acute phase. Put a tennis ball or lacrosse ball between your rhomboids and a wall and find the painful spot. Stay on this spot for 1-2 minutes. Ideally, your pain levels should decrease within that time frame despite constant pressure
- Heat: Putting a hot water bottle on painful muscles can often provide relief. A heat plaster can be an alternative.

To stretch the rhomboids, Sit in a flat, level chair. Move to the edge of the seat so your feet are flat on the floor and your knees are at right angles. Spread your legs a little more than hip-width apart. Reach over and grab your left ankle with your right hand. With your left hand, press into your right elbow crease until you feel a stretch between your spine and shoulder blade on the right side.
Hold the stretch for around 30 seconds, breathing deeply. Then return to start and repeat. Do 2 – 3 repetitions, then switch and do the same stretch on the other side.
The long-term solution to help and prevent rhomboid pain is – you guessed it – exercises. The following exercises are all targeted at the rhomboids amongst other muscles:
- Scapula Arm lifts
- 1-arm Rows
- Rear Delt cable pulls
- T-lifts on a gym ball or bench
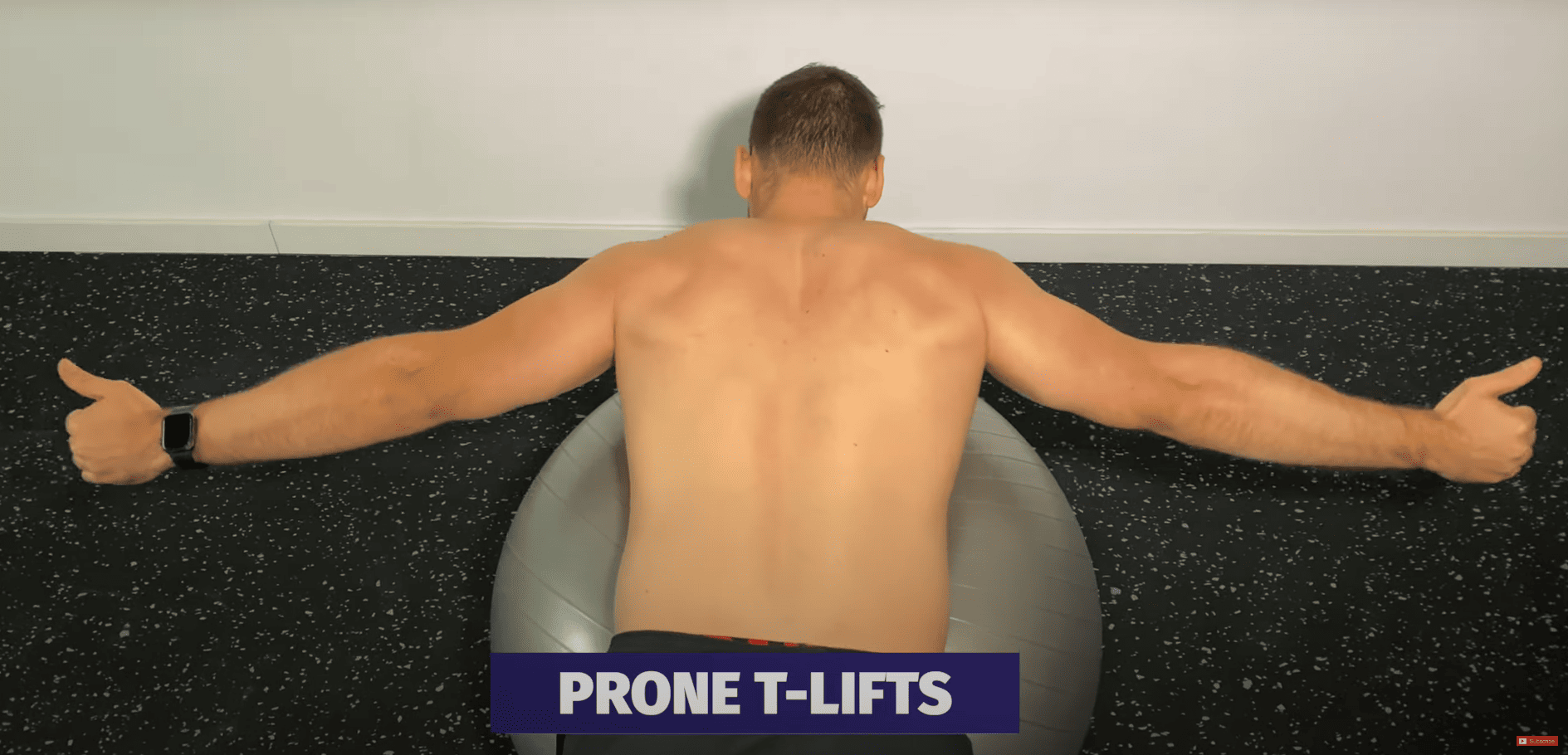
All exercises should be done with tolerable pain at max. In case a patient experiences an increase in pain, pain levels should settle to starting levels within 24 hours after the exercise. If the pain reaction lasts longer, you should decrease the training intensity or volume.
Alright, this was our blog on the cause of interscapular pain and possible treatment options for it. We hope this helped with some confusion that you might have about this topic.
As always, thanks for reading!
Kai
References

Kai Sigel
CEO & Co-Founder of Physiotutors
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







