Cervical Radiculopathy | Diagnosis & Treatment for Physiotherapists

Cervical Radiculopathy | Diagnosis & Treatment for Physios
Introduction & Epidemiology

Cervical radicular syndrome is the umbrella term encompassing cervical radicular pain and/or cervical radiculopathy. Even though “radicular pain” and “radiculopathy” are synonymously used in the literature, they are not the same. Radicular pain is defined as “pain evoked by ectopic discharges originating from a dorsal root or its ganglion”. Disc herniation (hernia nucleus pulposus, HNP), the most common cause, and inflammation of the affected nerve seem to be the critical pathophysiological process. Radiculopathy is yet another, distinct entity. It is a neurological state in which conduction is blocked along a spinal nerve or its roots (Bogduk et al. 2009).
This leads to objective signs of loss of neurologic function such as sensory loss (hypoesthesia or anesthesia), motor loss (paresis or atrophy), or impaired reflexes (hyporeflexia).
In the cervical spine, true disc prolapse and herniation of the nucleus pulposus are uncommon. The neural foramen is bordered ventrally by the uncovertebral joint and dorsally by the superior articular process of the caudal vertebrae. Compressive radiculopathies occur as a result of the mechanical distortion of the nerve root either by hypertrophied facet joints or uncovertebral joints, disc protrusion, spondylotic spurring of the vertebral body, or a combination of these factors (Abbed et al. 2007). HNP accounts for about 20%-25% of cervical radiculopathies and degenerative disc disease (DDD) accounts for about 70%-75% (Roth et al. 2009).
A review from Van Zundert et al. (2010) reports an annual incidence of 82,3 new cases of cervical radicular syndrome in 100.000 people, with an adjusted incidence of 107 for males and 64 for females. The study also reports that the most commonly affected nerve root is C7 in 45-60% of all cases, followed by C6 (20-25%) and C5 and C8 with both 10%.
Use the manual therapy app
- Over 150 mobilization and manipulation techniques for the musculoskeletal system
- Fundamental theory and screening tests included
- The perfect app for anyone becoming a MT
Clinical Presentation & Examination
Signs & Symptoms
The following signs & symptoms can be indicative of neck pain grade III (Bono et al. 2011, Kuijper et al. 2008):
- Pain in the neck is minor compared to arm pain, additionally possible scapular and periscapular pain
- Neck movements and maneuvers increasing intraspinal pressure like coughing
and sneezing worsens pain or tingling in the arm - Varying degrees of paresthesia, sensory loss (hypoesthesia) in the dermatomal region of the affected nerve root
- Identification of a restricted cervical range of motion, defined as rotation less than 60 degrees or limited and painful rotation
- Varying degrees of motor weakness (paresis) in the myotome of the affected nerve root
- Varying degrees of decreased deep tendon reflexes (hyporeflexia) of the corresponding nerve root
- Atypical signs & symptoms include deltoid weakness, scapular winging, weakness of the intrinsic muscles of the hand, chest or deep breast pain, and headaches
Examination
After patient history-taking, you might have formed the ICD (International Classification of Disease) hypothesis that your patient suffers from cervical radicular syndrome. You can then further decrease your clinical uncertainty by performing physical tests to either exclude or confirm the hypotheses. The first test battery is focused on the reproduction or easing of radicular pain and/or paresthesia:
A positive Spurling test is a very specific test that can confirm the diagnosis of cervical radicular syndrome. The test is positive upon reproduction of symptoms like pain and paresthesia in the arm and hand.
Other orthopedic tests to diagnose cervical radicular syndrome are:
- Cluster of Wainner
- Cervical Distraction Test
- Shoulder Abduction Sign
- Valsalva Maneuver
- Arm Squeeze Test
- Neck Tornado Test
During the second part of your examination, you should perform a neurological examination focusing on the presence and degree of radiculopathy evaluating hyporeflexia, hypoesthesia, and paresis:
The following video on dermatome testing was derived from the American Spinal Injury Association (ASIA) form:
Lee et al. (2008) evaluated the literature and created a composite dermatome map based on published data from 5 papers they considered to be the most experimentally reliable. Their maps look like this:
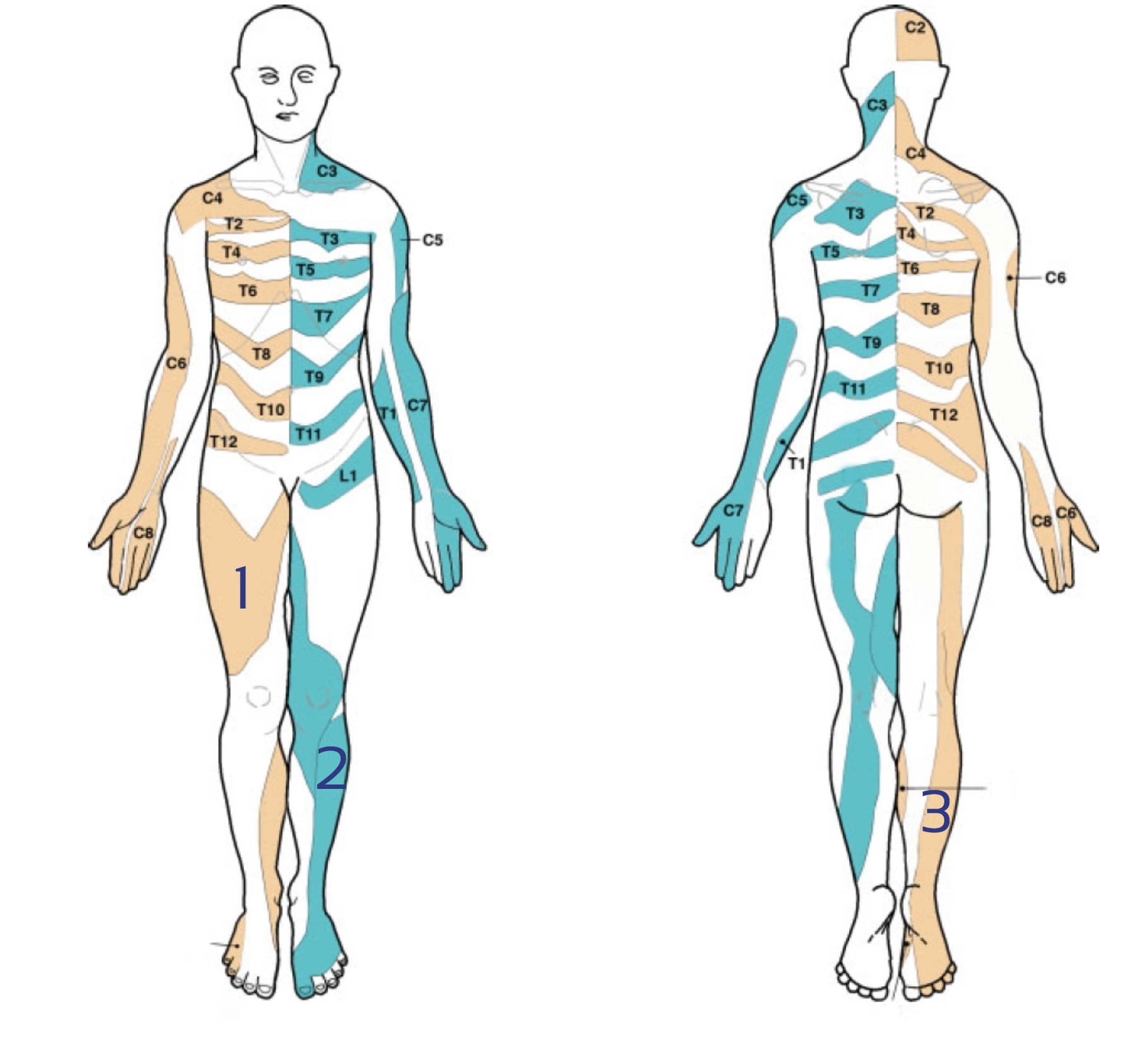
There is a lot of discussion going on about the reliability of dermatome maps. Check out our blog articles and research reviews if you want to learn more about it:
- Determining the Level of Cervical Radiculopathy
- Why Dermatome Maps may still useful
- 3 Truths University Didn’t Tell You about Radicular Syndrome
You can test the upper limb myotomes as explained in the following video:
Be aware, that cervical radiculopathy can be mimicked by a peripheral nerve entrapment. For more information check out the following videos:
- C5 radiculopathy or suprascapular nerve entrapment?
- C6, C7 radiculopathy or Carpal Tunnel Syndrome?
- C8 Radiculopathy or Ulnar Nerve Entrapment?
5 ESSENTIAL MOBILIZATION / MANIPULATION TECHNIQUES EVERY PHYSIO SHOULD MASTER
Use the manual therapy app
- Over 150 mobilization and manipulation techniques for the musculoskeletal system
- Fundamental theory and screening tests included
- The perfect app for anyone becoming a MT
Treatment
As in aspecific neck pain, treatment should be based on your findings from patient history-taking and examination. The goal is to focus on modifiable negative prognostic factors that can be influenced by therapy. Factors that we can directly influence positively are a high level of pain, disability, range of motion, and decreased joint mobility. Factors that might be influenced directly through advice and education, but also indirectly through treatment, are movement-related fear, catastrophic thinking, and passive coping.
If you go through the list of prognostic factors you can see that there are quite a couple of factors that we will hardly or not be able to influence. If a patient presents with dominant psychosocial factors or work-related factors, Bier et al. (2017) recommend considering contacting other medical professionals like psychologists or a physiotherapist specialized in work rehabilitation.
In the case of cervical radicular syndrome, the guideline of the Dutch Royal Society of Physiotherapists recommends advising the patient about the benign course of cervical radicular syndrome and that arm pain usually resolves on its own. Furthermore, advise the patient to stay active, but also to avoid movements and activities that aggravate the radiating pain or other arm complaints.
What does the evidence say about effective treatments?
Thoomes et al. (2016) have conducted a review and mention that the evidence for manual therapy and physiotherapy is sparse and most interventions are evaluated in only a single randomized controlled trial (RCT). Kuijper et al. (2009) have compared (1) physiotherapy focussing on neck and upper limb strengthening exercises with (2) a semi-rigid neck collar to (3) a wait-and-see approach in patients with acute neck pain. Their results showed a decrease in pain and disability measured on the Neck Disability Index (NDI) in all 3 groups at 6 weeks follow-up. The physiotherapy group and neck collar group experienced a significantly greater decrease in pain compared to the control group with only the collar group showing a significantly superior decrease on the NDI compared to the control. While this high-quality study was conducted in an outpatient setting of a hospital, Keating et al. (2019) will compare a multimodal physiotherapy approach to a wait-and-see group for patients with acute cervical radicular syndrome in primary practice.
Surprisingly, there is no single trial comparing the effectiveness of neck exercises for cervical radicular syndrome with a control group. For this reason, it is not possible to estimate the treatment effect of craniocervical flexion exercises although commonly prescribed. The following video gives you an idea, of which exercise could be used in your treatment:
While there is no evidence available for thoracic mobilization, Young et al. (2019) have found that “one session of thoracic manipulation resulted in improvements in pain, disability, cervical ROM, and deep neck flexor endurance in patients with cervical radiculopathy. Patients treated with manipulation were more likely to report at least moderate change in their neck and upper extremity symptoms up to 48 to 72 hours following treatment.”
A study of lower quality by Ragonese et al. (2009, no direct link available) compared manual therapy versus strengthening exercises versus the combination of both interventions. The results of this study suggest that a multimodal treatment approach using a combination of manual therapy and strengthening exercises is superior to treatment by either intervention alone.
Nee et al. (2012) compared “neural tissue management”, which included manual therapy techniques and nerve gliding exercises that have been advocated for reducing nerve mechanosensitivity, for 4 treatments within 2 weeks with a wait-and-see approach. They found participant-reported improvement regarding neck & arm pain and disability in the experimental group compared to the control group.
Kim et al. (2017) compared neural mobilization with manual traction to manual traction alone. Both interventions were done 3 times a week for 8 weeks. They found improved pain, disability, range of motion, and muscle endurance of the deep cervical flexors in the combined group vs. the traction group after 4 and 8 weeks.
In the following video you can see an example of nerve gliders and tensioners that can be performed as home exercises by patients:
There is some debate about cervical traction as a treatment option for cervical radicular syndrome. Romeo et al. (2018) conducted a systematic review and meta-analysis and found that mechanical traction – when added to physiotherapy – had a significant effect on pain in the short and intermediate-term and disability in the intermediate term. Manual traction had a significant effect on pain in the short term. They conclude that the current literature lends some support to the use of mechanical and manual traction for CR in addition to other physical therapy procedures for pain reduction, but yielding lesser effects on function/disability.
Surgical treatment
Engquist et al. (2013) compared the results of surgery and physiotherapy with physiotherapy alone. They showed that surgery with physiotherapy resulted in a more rapid improvement during the first postoperative year, with significantly greater improvement in neck pain and the patient’s global assessment than physiotherapy alone, but the differences between the groups decreased after 2 years. Therefore, they conclude that structured physiotherapy should be tried before surgery is chosen.
Another study by Peolsson et al. (2013) also compared surgery with physiotherapy to physiotherapy alone. At a 2-year follow-up, the groups did not show any significant difference in neck muscle endurance, manual dexterity, and right hand-grip strength. Therefore, the authors also conclude that physiotherapy should precede a decision for surgery.
At last, an older study by Persson et al. (1997) compared surgery for cervical radicular syndrome to physiotherapy or a cervical collar. After 4 months, the surgery group reported less pain, less sensory loss, and better muscle strength compared to the 2 conservative groups. However, at a 1-year follow-up, there was no significant difference between any of the 3 groups.
So while surgery might be able to improve symptoms in the mid-term, results seem to be equal for physiotherapy and surgery in the long term.
Do you want to learn more about cervical radiculopathy? Then check out our blog articles and research reviews:
- Determining the Level of Cervical Radiculopathy
- Why Dermatome Maps may still useful
- 3 Truths University Didn’t Tell You about Radicular Syndrome
- Physiotherapy for Painful Radiculopathies
References
Use the manual therapy app
- Over 150 mobilization and manipulation techniques for the musculoskeletal system
- Fundamental theory and screening tests included
- The perfect app for anyone becoming a MT
Finally! How to Master Treating Spinal Conditions in Just 40 Hours Without Spending Years of Your Life and Thousands of Euros - Guaranteed!

What customers have to say about this course
- Shachaf Alexander19/07/24Orthopedic Physiotherapy of the Spine Orthopedic Physiotherapy of the spine
Interesting course packed with useful data and practical tools.
I highly recommend.Verena Fric25/11/22Orthopedic Physiotherapy of the Spine GREAT COURSE ABOUT THE SPINE
great course, best overview about the different syndromes of the spine, very helpful and relevant for the work with patients - Peter Walsh01/09/22Orthopedic Physiotherapy of the Spine 5 starsChristoph21/12/21Orthopedic Physiotherapy of the Spine Really a well done course, using the modern ways of teaching. Compliments! Sometimes for me you entered too much into details instead of touching more important chapters of Spine treatment like techniques for the treatment of muscles and fascias
- John09/10/21Orthopedic Physiotherapy of the Spine EXCELLENT COURSE HIGHLY RECOMMEND
As a newly graduated physiotherapist i highly recommend this course just to know you are on the right track with your patients. the information presented is very clear and easy to follow as well as the great physiotherapy style videos. It makes learning actually fun , thanks guys for all your hard work. Well deserved.Alexander Bender06/09/21Orthopedic Physiotherapy of the Spine During the corona crisis, I booked many online courses and webinars, but none were as entertaining and well thought out as PhysioTutors’ courses.
All units are well summarized, meaningfully broken down and easy to understand.
I am looking forward to the other courses.
Many greetings from Germany. - GHADEER05/01/21Orthopedic Physiotherapy of the Spine VERY INFORMATIVE AND UPDATED
for anyone who is lost in handling spine cases, this course is very helpful.MICHAEL PROESMANS20/12/20Orthopedic Physiotherapy of the Spine HIGHLY METHODICAL, WITH PLENTY OF SCIENTIFIC REFERENCE
Clear, structured and well researched course concerning most common pathologies of the spinal complex.
Plenty of informative modules, with detailed video-analysis.
If you’re looking for a course to study in your own time, with enough depth and scientific background, then you’ve found a very good one here.
Bang for buck, a great course. - BENOIT08/05/20Orthopedic Physiotherapy of the Spine After finishing the Orthopedic course for Lower & Upper limbs, I was looking forward to begin this Spine specific course.
Really good overview about all spine pathologies from epidemiology to diagnosis & treatment which made me more confident to care for my future patients.
ANOTHER GREAT COURSE !
The courses are well detailed with lot of informations and videos.
For me these 2 courses are must to see to learn and update knowledge for most common pathologies in Physiotherapy.Nicolas Cardon27/04/20Orthopedic Physiotherapy of the Spine This is a very interesting course !
We can find many informations about the main pathologies and their differential diagnosis and about objective and subjective exam. Videos are clear and well designed.
It’s a very well course for these who wish complete their Orthopedic Manual Therapy curriculum.
A French Physio’







