3 Truths University didn’t tell you about Radicular Syndrome

I’m sure a lot of students and therapists out there have learned that radicular pain and radiculopathy follow a dermatomal distribution. But is that really true and exactly like we have learned it from textbooks?
First of all, let’s distinguish between radicular pain and radiculopathy. Even though “radicular pain” and “radiculopathy” are synonymously used in the literature, they are not the same. Radicular pain is defined as “pain evoked by ectopic discharges originating from a dorsal root or its ganglion”. It’s the neuropathic, electric pain that patients feel shooting down the leg.
Radicular syndrome is the umbrella term for radicular pain (pain originating from the radix) and radiculopathy (conduction block along a spinal nerve or root)
Radiculopathy is yet another, distinct entity. It is a neurological state in which conduction is blocked along a spinal nerve or its roots (Bogduk et al. 2009). This leads to objective signs of loss of neurologic function such as sensory loss called hypoesthesia or anesthesia in the severe form, motor loss called paresis or atrophy in the severe form, or impaired reflexes called hyporeflexia or areflexia if they are completely absent. If radicular pain or radiculopathy or both are present, we are talking about radicular syndrome, which is an umbrella term.
Does radicular pain follow a dermatomal pattern?
Okay, so now let’s see if radicular pain follows a dermatomal pattern. A study by Murphy et al. (2009) observed pain patterns in patients with radicular pain and found the following:
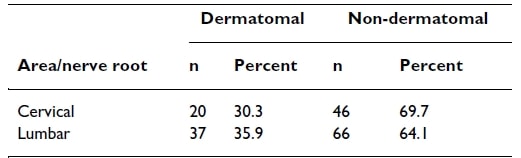
Radicular pain in the cervical spine followed a dermatomal distribution in only 30% of cases, while in the lumbar spine, it was slightly better with 36%. Now let’s look at specific dermatomes separately.
For the cervical levels, only C4 seems to be more or less reliable with 60% – although we have to be careful with the interpretation here as there were only 2 patients with an affected nerve root at C4. All other levels do not seem to be reliable.
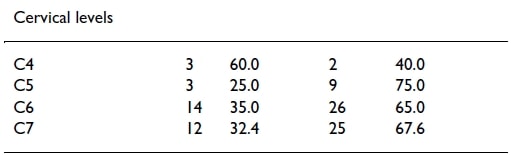
It doesn’t get much better for the lumbar spine:
It seems that only level S1 might be more or less reliable with 65% of patients with an S1 nerve root compression reporting pain in the dermatomal distribution of S1. All other levels did not follow a dermatomal distribution regularly. It has to be said though that Murphy and colleagues included patients with multi-level disease, which probably decreased the reliability a bit. Another, more recent study by McAnany et al. (2019) observed pain patterns in cervical radiculopathy. They found that only 54% fit the regular dermatome pattern described in the Netter anatomy book. In the non-standard distribution, dermatomal levels differed by 1.68 levels either cranially or caudally from the standard.
Radicular pain only seems to reliably follow a dermatomal distribution in nerve roots C4 (60%) and S1 (65%)
How reliable are dermatomes, myotomes, and reflexes?
Okay, so if radicular pain is not reliable and mostly reported as a shooting, electric pain along the whole distribution of the arm or the leg – how reliable are our dermatomes, myotomes, and reflexes?
A study by Rainville et al. (2017) compared sensory changes and weakness in patients with C6 and C7 radiculopathy. They concluded that these symptoms have limited value to differentiate between the two levels. Al Nezari et al. (2013) performed a meta-analysis to see if a peripheral neurological examination is able to diagnose the level of lumbar disc herniation. They state that sensory, motor, and reflex testing all had a low sensitivity, moderate specificity, and limited diagnostic accuracy to determine the level of disc herniation. So while a neurological examination may help to confirm the presence of radicular syndrome and to assess hypofunction to establish a baseline and to monitor treatment progress, it cannot determine the affected level of nerve root compression.
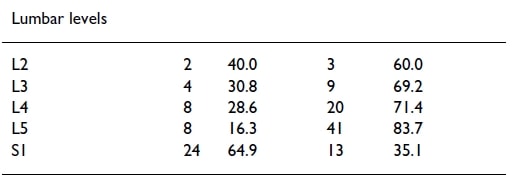
Now, what is the reason that our dermatome maps are so unreliable? The literature mentions several possibilities. First, there is huge variability in the brachial and lumbosacral plexus. If we look at cadaver studies for the brachial plexus, a typical textbook anatomy of the brachial plexus was only found in 37-77% of cases. Two major variations are described in the brachial plexus:
We are talking of “prefixation” when nerve root C4 contributes considerably to the plexus and T1 does not or only minimally. This variation has a prevalence of between 26-48%. The second variation is called “postfixation”. This is the case if there is only little or no contribution from C5 and considerable innervation from T2. This variation is present in 4% of the population. A prefixation or postfixation can shift the observed pattern of cervical radiculopathy cranial or caudal depending on the anatomic variant present.
A second reason is that intradural connections of rootlets in more than 50% of cadavers are found by C5 and C6 and C6 and C7. Such a connection between rootlets of different nerve roots is called anastomosis.
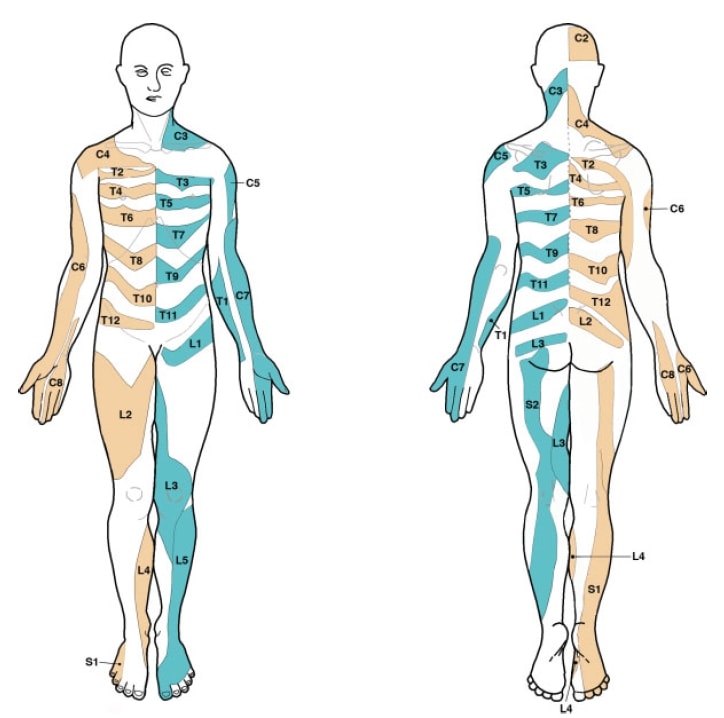
Third, textbooks commonly used in medical health programs contain multiple, conflicting dermatome maps. On top of that, the seminal basis that formed dermatomal maps is flawed in various ways. For example, the map created by Garrett and Keegan in 1948 has never been confirmed by follow-up studies up to this day, yet this map is mostly used in textbooks. Lee et al.(2008) evaluated the literature and created a composite dermatome map based on published data from 5 papers they considered to be the most experimentally reliable. Their map looks like this, which might be a bit different from what you and we have learned at school:
Okay, let’s summarize: So neither radicular pain nor radiculopathy seem to follow a strict dermatomal pattern of maps we have learned in school. So with our clinical examination, we’re probably not able to determine which nerve root is affected. At the same time, this information is probably way more important for surgeons than for us as physiotherapists. If someone is suffering from radicular symptoms coming from L5 or S1 won’t probably change our management strategy in any important way. You may want to continue doing your neurological assessment to confirm radiculopathy and to evaluate the degree of hypofunction. At the same time keep in mind the high degree of anatomical variation and that predicting the affected level is impossible.
Orthopedic Physiotherapy of the Spine
Master Treating Spinal Conditions in Just 40 Hours Without Spending Years of Your Life and Thousands of Euros
Alright, we hope this answered the question thoroughly. Comment down below if you were surprised about the actual evidence and if you have any further questions. A lot of this information and much more can be found in our online course on the spine.
Thanks a lot for reading!
Kai

Kai Sigel
CEO & Co-Founder of Physiotutors
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







