Meniscus Tear | Diagnosis & Treatment for Physios

Meniscus Tear | Diagnosis & Treatment for Physios
The meniscus is essential for stability, shock absorption, distribution of forces, lubrication in the knee as well as proprioception. (Englund et al. 2009)
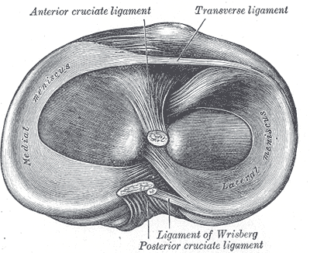
The lateral meniscus has the form of a half-circle and has a greater tibial surface area than the medial meniscus. It is approximately 3cm wide and 3-4 cm long and is attached to the tibia anteriorly and posteriorly. The ligamentous attachment of the lateral meniscus is less developed, which gives it more freedom of movement than the medial meniscus.
Meniscus injuries are mostly caused by rotation of a flexed knee into extension (Bansal et al. 2002).
All movements which can lead to ligament injuries in the knee can also cause meniscus injuries (Solomon et al. 2002). For this reason, meniscal tears are often seen together with anterior cruciate ligament (ACL) tears. In acute injuries, the lateral meniscus is torn more often than its medial counterpart (Smith et al. 2001). On the other hand, the medial meniscus tears more often in patients with chronic ACL- insufficient knees who suffer a new trauma (Murrel et al. 2001, Keene et al. 1993, Irvine et al. 1992).
These different scenarios also lead to a different localization and type of rupture: In the case of a medial meniscus tear (with a chronic ACL tear) peripheral ruptures in the dorsal horn are seen more often and with a lateral meniscus tear (in the case of an acute ACL tear) more ruptures are seen in the dorsal horn or the mid-lateral third. (Shelbourne et al. 1991, Thompson et al. 1993, Smith et al. 2001).
The menisci can be damaged through acute trauma or long-lasting overuse. Partial or full tears in the medial or lateral meniscus are further categorized into:
– Vertical/longitudinal tears may progress to Bucket Handle Tears
– Radial/Transverse tears may progress to Parrot Beak Tears
– Horizontal tears may progress to Flap tears
Epidemiology
The incidence of a meniscus injury presenting to the general practitioner is estimated at 2 out of 1.000 patients per year with a male: female ratio of 2,5:1 (Belo et al. 2010). In a prospective cohort study in a primary care setting in the Netherlands, 35% of patients between 18 and 65 with an acute knee injury were diagnosed with a meniscus tear. In the same study, 11% had a combined ACL and meniscus tear, while 9% had a combined medial collateral ligament tear and meniscus tear (Kastelein et al. 2008).
While traumatic tears often occur in the menisci periphery and are seen in patients younger than 30, more complex and degenerative patterns tend to occur in older adults (Poehling et al. 1990).
It should be mentioned that meniscus abnormalities seen on MRI seem to be extremely common in the asymptomatic population as well.
In a study by Beattie et al. (2005) 43 out of 44 asymptomatic individuals with mean age of 41.1 (age range 20-68) showed at least one meniscal abnormality.
27 individuals (61.4%) had abnormalities in at least three of the four regions of the knee.
It is important to add that meniscal tears can lead to knee osteoarthritis (OA), but knee OA can also lead to a spontaneous meniscal tear through the breakdown and weakening of meniscal structure (Englund et al. 2009). While the prevalence of meniscus tears is very high in asymptomatic individuals, Bhattacharyya et al. (2003) found a significantly higher frequency of meniscal tears in individuals with symptomatic OA. On top of that, a study by Hunter et al. (2006) found a strong association between meniscal damage and cartilage loss.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
A meniscal injury can cause pain and edema and a locking knee during flexion and extension.
The chance of a meniscus lesion is increased in case the patient is older than 40 years of age and has suffered from a rotation trauma during weight-bearing of the knee, which makes continuing activity impossible. Furthermore, a popping sensation during trauma makes a meniscal tear more probable (Wagemakers et al. 2008).
Further clinical signs & symptoms include (Décary et al. 2018, Wagemakers et al. 2008), :
– Isolated medial or diffuse knee pain location
– Knee complaint with progressive onset in degenerative meniscus tears
– Mild to severe pain while pivoting on the knee during activities of daily living or sports
– Joint swelling 12-24 hours after trauma
– Joint line tenderness
– Reduced AROM
– Pain in the end ranges of motion
Physical Examination
Shrier et al. (2010) argue that the physical examination for meniscal tears is different than diagnostic tests as meniscal tears are heterogeneous in nature, for example, posterior vs. anterior tears. Therefore, the authors reason that sensitivity and specificity values should not be relied on for meniscus injuries, but the choice of physical tests should rather be based on the logic underlying how different tests stress different parts of the meniscus.
Another very common test to diagnose meniscus tears is the Appley Test:
Other orthopedic tests to assess patellofemoral pain are:
- Joint Line Tenderness
- Jump Sign /Finochietto Test
- Thessaly Test
- Ege’s Test
- Duck Walk Test
- Bounce Home Test
THE ROLE OF THE VMO & QUADS IN PFP

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Meniscectomy or partial surgical meniscus repair is one of the most common orthopedic surgeries worldwide. However, in recent decades, this procedure has come under fire as several randomized controlled trials have shown equally satisfactory results with conservative management. Furthermore, Sihvonen et al conducted a randomized trial that compared arthroscopic partial meniscectomy to sham surgery which showed no difference and an even slightly higher risk of developing knee OA 5 years after surgery. Let that sink in for a moment.
So, the described conservative management of meniscus tears in the literature typically involved a combination of a warm-up, range of motion, strength, and joint control/proprioceptive exercises done for 2-3 sessions per week over the course of 12 weeks. These sessions were either supervised or done independently by the patient. Patients were assessed with validated outcome measures such as the KOOS, Lysholm knee score, Tegner activity scale, and isokinetic strength measurements.
We will present a couple of exercise progressions for each domain:
Make sure you identify the specific needs of your patient. For example, for some people, a lunge may be necessary for their ADL or work so you would incorporate those in your training as well. This is also a long list of exercises and we shouldn’t overwhelm our patients with a ton of exercises. Keep it to a minimum of 3-5 exercises.
What about patients with mechanical symptoms like knee locking or catching?
Sihvonen et al. (2016) compared the outcomes of 900 consecutive patients with symptomatic degenerative knee disease and meniscus tear undergoing arthroscopic partial meniscectomy. They then compared the outcomes of patients with mechanical knee catching or locking and patients without mechanical symptoms. Surprisingly and in obvious contrast to the prevailing consensus and most guideline recommendations, the study indicates that a preoperative self-report of mechanical symptoms is actually associated with a less favorable outcome of surgery than the absence of these symptoms. Of all patients with mechanical symptoms, locking or catching was alleviated in only 53%. At the same time, 11% of patients without prior mechanical symptoms experienced locking or catching after surgery.
One of the key findings of the study was that mechanical symptoms were more prevalent in patients with knee OA. This data suggests that mechanical symptoms are actually attributable to general knee degeneration, rather than a distinct lesion such as a degenerative meniscus tear.
Progressive Exercise therapy consisting of neuromuscular and strength exercises for the lower limbs, mainly the quadriceps, and performed 2-3 times a week for a duration of 12 weeks has been shown to be effective in middle-aged patients with degenerative meniscus tears (Kise et al. 2016). While the effectiveness of an exercise program for younger patients under 40 with traumatic meniscus tears yet has to prove its effectiveness, the general focus of exercise is no different compared to that of degenerative tears.
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Increase Your Treatment Success in Patients with Knee Pain
What customers have to say about this online course
- Esra06/02/25Leuk en nuttig! Leuke cursus. Leuke afwisseling tussen tekst, video en toetsjes. Prettig dat de tekst in het Nederlands was.Linda Valk01/01/25Pfp syndroom cursus Hele fijne cursus, met duidelijke uitleg, zowel theoretisch als praktisch duidelijk.
- Erik Plandsoen31/12/24PFP & Hoffa fat pad syndrome Hele fijne cursus, met duidelijke uitleg, zowel theoretisch als praktisch duidelijke oefeningen.Anneleen Peeters22/12/24Great! Super interesting and insightful. Definitely a great tool to freshen up and expand on previous knowledge.
- Ronald Dols13/12/24Top cursus Mooie holistische benadering van een veelvoorkomend probleem.Olivier21/11/24Goede cursus! Hele goede cursus!
- Berfin Karagecili03/09/24Patellafemoraal pijn en fat pad syndroom Patellafemoraal pijn en fat pad syndroom
Hele duidelijke uitleg met instructie video’s. de tussentijdse toetsen waren ook handig om zo 100% uit je stof te kunnen halen.Martijn de Bruijn24/05/24PATELLOFEMORAL PAIN & FAT PAD SYNDROME It was a great course by Claire!! Nice explanation of the examination and treatment modalities.
Also the sport specific parts were very helpful. - Jean-Christophe Di Ruggerio04/03/24PATELLOFEMORAL PAIN & FAT PAD SYNDROME Great course with a knee expert!Seppe van den Audenaerde09/12/23PATELLOFEMORAL PAIN & FAT PAD SYNDROME GREAT COURSE THAT OPENED MY VIEW ON KNEE PAIN
Because of the way Claire looks at the knee joint and its surrounding joints, I learned a lot and it opened my eyes. Will look into her other courses for sure! - Alvin Chi24/07/23PATELLOFEMORAL PAIN & FAT PAD SYNDROME BEST PFPS RESOURCE I HAVE FOUND
I cannot recommend this course enough. I stumbled upon this course through the physiotutors podcast, and Claire’s episode on there intrigued me enough to purchase the course. As someone who treats PFPS every day, I have yet to find a resource that tries to personalize treatment for the patient rather than broadly treating all patients the same. Claire goes into detail on how physical exam findings lead to different treatment options. I wish this course was available 10 years ago. I highly recommend this course and hope Claire continues to contribute more courses on physiotutors!Cesare Cambi15/06/23PATELLOFEMORAL PAIN & FAT PAD SYNDROME COURSE ABSOLUTE AMAZING
The course has given me a very deep and practical insight over the PFPS’ patients. it was full of nice and important clinical and practical tips for everyday usage, thing that I really enjoyed and appreciated
I personally liked the most the sections regarding the assessment strategies and the brace and taping’s techniques, but overall a must-do course on for anyone interested in improving his/her skills in the treatment of Knee pain. - Lorna Thornton-McCullagh14/06/23PATELLOFEMORAL PAIN & FAT PAD SYNDROME THANK GOODNESS FOR CLAIRE PATELLA
What a brilliant course. A colleague had attended her course and recommended it to me- I never fancied attending London so when it came on line I grabbed the opportunity. Claire P always presents complicated material clearly and thoroughly without the normal physiotherapist pomp and circumstance. This course has been well researched with up to date evidence and well conveyed- THANK GOODNESS FOR CLAIRE PATELLAGeorge Hill12/05/23PATELLOFEMORAL PAIN & FAT PAD SYNDROME Excellent course by Claire Robertson, I thoroughly enjoyed it. Learned so much!. Well done physiotutors, keep up the great work you guys are doing. - Hannah Toppets06/12/22PATELLOFEMORAL PAIN & FAT PAD SYNDROME PFP & FAT PAD SYNDROME
Great course with nice video’s and clear info on the objects. Also nice to have a little quiz after each chapter. Nice to know how to tape and sport-specific rehab.




