Learn
Referred Pain Thoracic Spine | Thoracic Screening | Visceral Referred Pain
One of the major challenges for a clinician seeing patients with neck and shoulder pain is determining the source of the symptoms. Similar to low back pain, in thoracic pain, we often cannot accurately determine a source of nociception, but we will have to rule out serious pathology.
One such source, that is often overlooked, but that has to be ruled out during your screening process is true and referred visceral pain. True visceral pain arises as a poorly defined sensation usually perceived in the midline of the body, at the lower sternum or upper abdomen. This diffuse nature and difficulty in locating visceral pain are due to a low density of visceral sensory innervation and extensive divergence of visceral input within the central nervous system. Visceral pain is therefore perceived more diffusely than noxious cutaneous stimulation with respect to location and timing. Subsequent symptoms may entail referred pain to somatic structures that share the same segmental innervation and that are more densely innervated. This way, visceral referred pain can mask as pain from musculoskeletal structures. If you want to dig deeper into the neurophysiological mechanism behind this phenomenon, check out this post.
Sikandar et al. in the year 2012 point out that somatic pain can be distinguished from visceral pain as it is often associated with marked autonomic phenomena, including pallor, profuse sweating, nausea, GI disturbances, and changes in body temperature, blood pressure, and heart rate. At the same time, it often produces strong affective responses, and therefore can be reinforced by anxiety and depression.
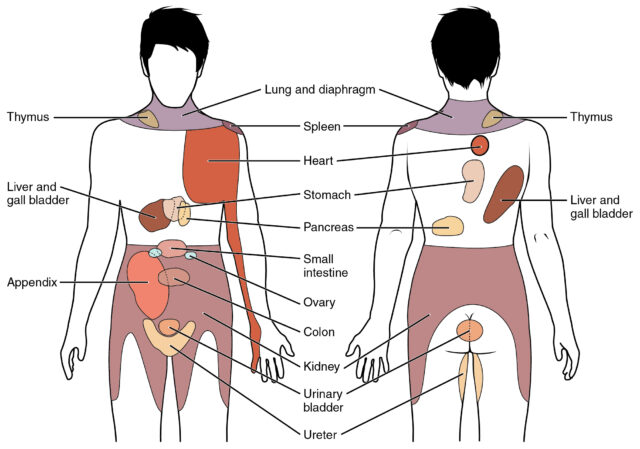
So which organs have their segmental innervations in the thoracic spine and can potentially refer pain to the mid and upper back? These are the following:

In case a patient complains about radiating symptoms along the ulnar side of the arm mimicking C8 radiculopathy or ulnar nerve entrapment is a pancast tumor.
For the cardiovascular system you could ask for:
- Heart trouble
- Pain or pressure on the chest
- Palpitations, so an abnormality of the heartbeat
- History of smoking
- High blood pressure
- Shortness of breath- including nocturnal
- Swelling of extremities
- Family history of cardiovascular disorder
- Elevated cholesterol level
Items you could ask for the pulmonary system are:
- History of smoking
- Shortness of breath
- Wheezing
- Prolonged coughing
- Sputum-amount/color
- History of asthma, emphysema, pneumonia, tuberculosis
The organs of the digestive system generally refer pain to the thoracic spine with the exception of the large intestine, sigmoid colon, and esophagus:

In your interview you should ask for:
- Difficulty with swallowing
- Nausea/heartburn
- Vomiting
- Specific food intolerances
- Constipation
- Diarrhea
- Changes in the color of stools
- Rectal bleeding
- Jaundice
- History of liver or gallbladder problems
You can imagine that some of these questions are very straightforward and private and probably not what a new patient expects during the intake. For this reason, it’s important to explain why you are asking these questions. In our experience, it makes sense to start with more general questions (for example: Do you have abdominal pain?) and dig deeper with the more specific questions if the initial questions were positive.
A more general tract that is often overlooked as it is not specific to a certain area is the locomotor tract. If the patient describes insidious onset of symptoms in multiple joints, the therapist should be wary of the presence of inflammatory disorders (i.e., rheumatoid arthritis, systemic lupus, etc.) as opposed to multiple areas exhibiting pure mechanical musculoskeletal dysfunction. Questions you could ask for the locomotor tract are: if there is pain, swelling, or movement restriction in other joints in the body next to the joint the patient is primarily complaining about.
At last, there are a couple of general evaluation principles that will help you to distinguish visceral pain or visceral referred pain from musculoskeletal pain. These are:
- Pain from musculoskeletal structures can be related to a change in body or limb position or to specific movements. So if the symptoms do not vary, regardless of body position and movement and are present at rest –especially if the pain is most severe waking them up at night – a pathological disorder should be suspected
- We have already mentioned that visceral pain is described to be poorly localized, diffuse, dull, and vague in character. It can be constant, but may rhythmically build up to a peak and then recede. Sensations of cramping pain have been attributed to spasms of the muscle wall of the hollow viscus and have been described in gastroenteritis, constipation, menstruation, gallbladder disease, and ureteral obstruction.
- The behavior of symptoms from visceral organs will vary depending on the function of the organ. They might thus be related to eating habits or ingestion of certain foods, may occur with bowel or bladder fullness or constipation, or be associated with the actual acts of urination or defecation
- Contrary to musculoskeletal pain in which patients often report an incident, accident, or trauma marking the onset of complaints, a serious pathology might be suspected in case of insidious onset with unexplained symptom development.
- Questions about general health may also reveal critical information. Signs& symptoms like fever, chills, nausea, unexplained weight loss, malaise, vomiting, changes in bowel habits, or rectal and vaginal bleeding for more than 1 or 2 weeks might be an indicator of serious pathology. Make sure that you are aware of conditions that the patient is currently treated for or has been treated for in the past as many can have a history of recurrence and ask for family history as well.
- Last, patient information including age, gender, occupation, and ethnicity may place people at higher risk for the development of specific diseases.
Be aware, that no single question allows you to reach a conclusion. What we are looking for is a pattern that might indicate serious pathology. It has to be said that you are not trying to make a specific diagnosis for certain organ pathology here. This is out of the scope of a physio and the expertise of an MD. The message that we want to bring across here is that it should become routine to include screening for visceral pathology during your screening process as well, so you can refer out if serious pathology is suspected.
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
Similar to the thoracic spine, visceral referred pain can also refer to the cervical spine and the lower back. Check out our posts on those two areas as well:
References:
References
Like what you’re learning?
BUY THE FULL PHYSIOTUTORS ASSESSMENT BOOK
- 600+ Pages e-Book
- Interactive Content (Direct Video Demonstration, PubMed articles)
- Statistical Values for all Special Tests from the latest research
- Available in 🇬🇧 🇩🇪 🇫🇷 🇪🇸 🇮🇹 🇵🇹 🇹🇷
- And much more!