Management of Whiplash Associated Disorders
Whiplash associated disorders are one of the toughest conditions to manage as a physiotherapist. Do you know what to do?

Introduction
Whiplash associated disorders are a common complaint in today’s society. The main symptom of whiplash is neck pain although symptoms such as stiffness, dizziness, paresthesia/anesthesia in the upper quadrant, headaches, and arm pain are frequently reported as well.
International data suggests that approximately half of people sustaining a whiplash still report symptoms one year after the accident. Psychiatric disorders such as post-traumatic stress disorder, depression and anxiety are often associated and these individuals usually report higher levels of disability, pain and reduced physical function.
More of a listener/watcher than a reader? Make sure to watch this synopsis video on the topic.
Recovery
Three general pathways of recovery are identified. You can see that if recovery occurs, it will take place in the first 2-3 months after the injury, as seen in this image below.
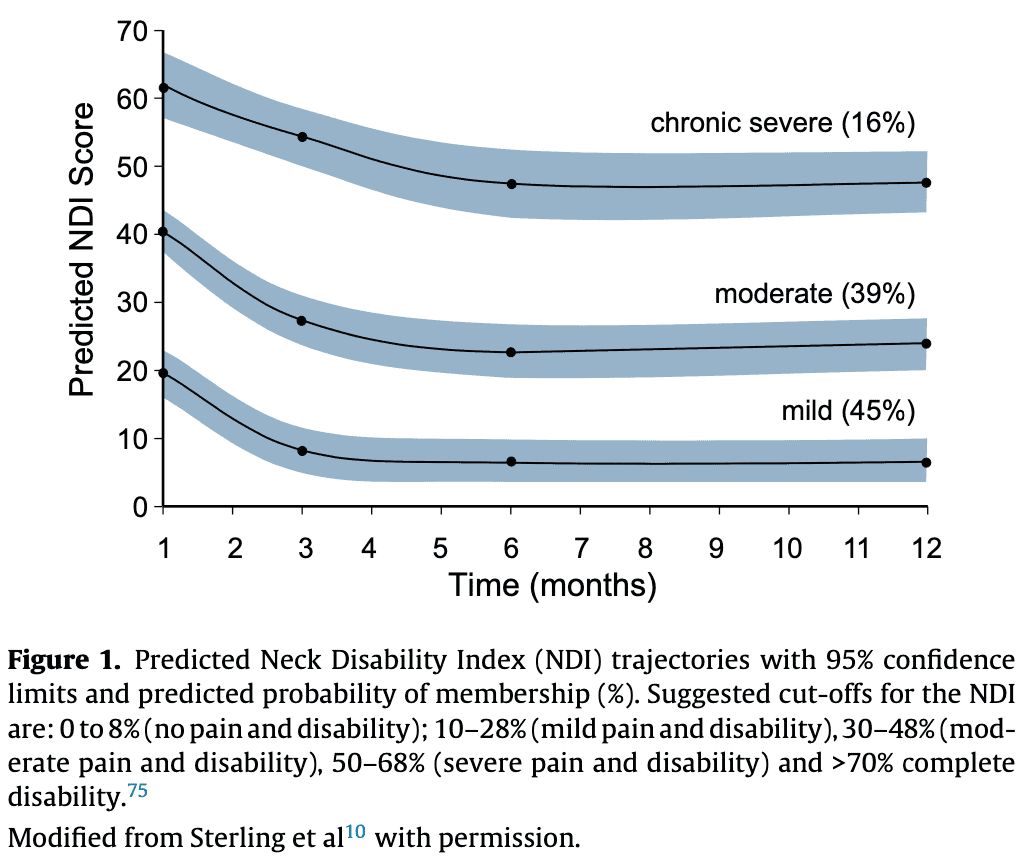
A clinical prediction rule was found for full recovery, being: neck disability scores under 32% with an age under 36 years.
A common question will then be: can we identify the patients that will develop chronic symptoms, as well as those that recover fully?
A clinical prediction rule was found for full recovery, being: neck disability scores under 32% with an age under 36 years.
Predicting moderate to severe disability at 12 months was fairly possible with a neck disability score of more than 40%, an age above 34 years, and a score of more than 5 on the hyperarousal subscale of the posttraumatic stress diagnostic scale.
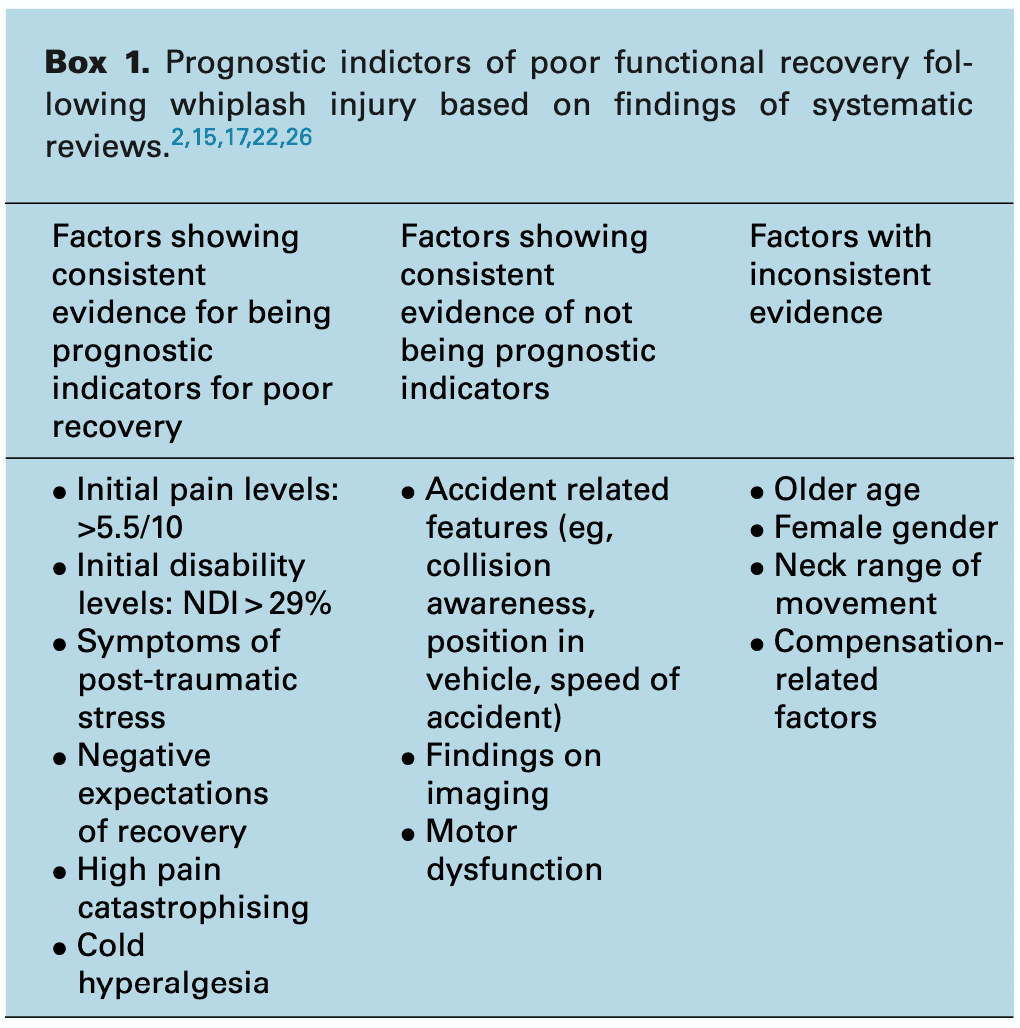
Below you can see other prognostic indicators of poor functional recovery.
Clinical examination
At your first consultation the pain and disability should be reported because of its consistent prognostic capacity. The visual analogue scale and neck disability index can be of use here. Keeping an eye out for psychological issues is recommended. Examples are an inability to sleep due to thoughts about the accident or avoiding driving due to fear. For more information about measuring psychological issues, check out this table.
Much of the clinical examination is in line with the neck pain guidelines, found here.
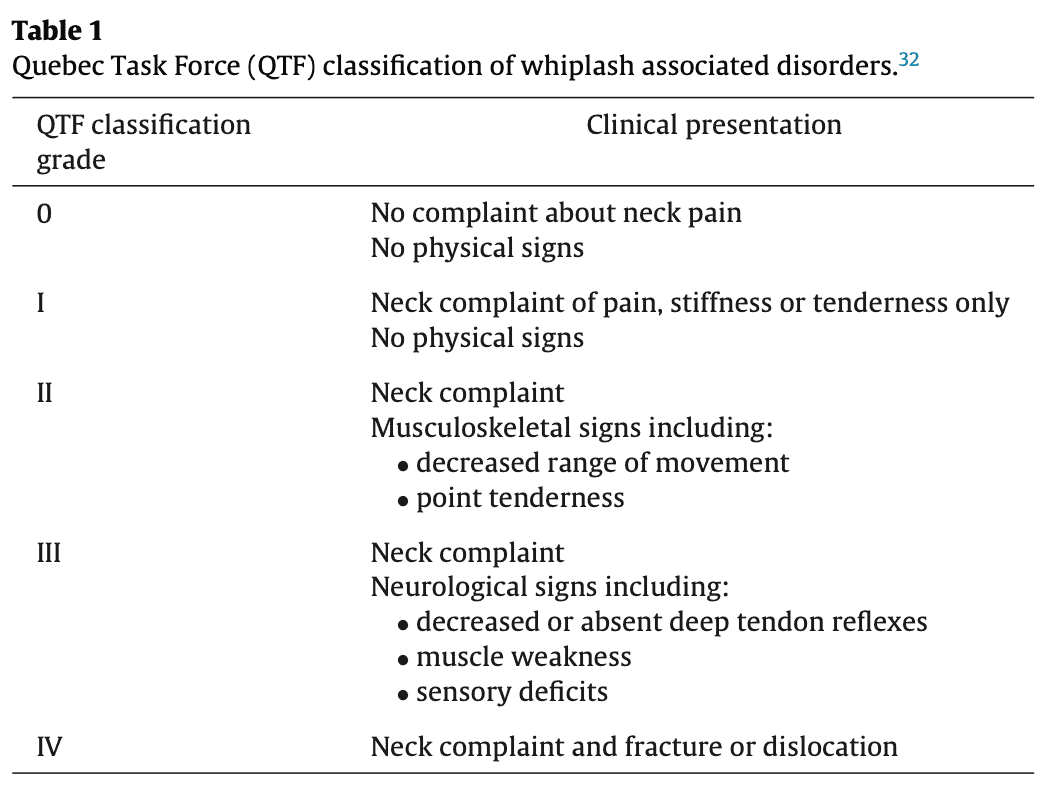
Classifying whiplash associated disorders is possible with the Quebec Task Force classification. Most patients will fall in category number two. Identifying specific structures at cause is impossible in most cases. Imaging is therefore only required when grade 4 disorders are suspected. The Canadian C-spine rule or Nexus rule are valid tools for elevating this suspicion.
Patients with whiplash associated disorders often report diffuse symptoms of sensory loss or gain and generalized muscle weakness. This is frequently due to altered nociceptive processing, and not necessarily a neurological compromise.
Previous research has found inferior performance on tests of motor control involving the cervical flexor, extensor and scapular muscle groups when compared to asymptomatic control participants; changes in muscle morphology of the cervical flexor and extensor muscles; loss of strength and endurance of cervical and scapular muscle groups; and sensorimotor changes manifested by increased joint re-positioning errors, poor kinaesthetic awareness, altered eye movement control, and loss of balance. That is a mouthful, you can read up about the assessment of these issues in Jull et al 2008.
Orthopedic Physiotherapy of the Spine
This course will enable you to become confident in screening, assessing and treating the most common pathologies in the cervical, thoracic and lumbar spine based on the very latest evidence.
Management
Now, how do we manage these patients? Advice to stay active and picking up where they left off in their activities should be one of the first things to do. And exercise should work, right? Kinda, but not much, and effects do not seem to hold up long. Exercise therapy generally has small effect sizes for whiplash associated disorders. At least it’s better than a soft collar or rest.
The type of exercise does not seem to matter so we could just scale up whatever the patient likes between range of motion exercises, McKenzie exercises, postural exercises, and strengthening and motor control exercises.
Manual therapy can be added as long as the patient benefits from it, measured with validated outcome measures. However, the quality of evidence is low.
As you’ve probably heard, there are few effective treatments for whiplash associated disorders. More research is needed.
Reference

Max van der Velden
Research Manager
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







