The Myth of Core Stability – Stop blaming a weak core for low back pain

The myth of core stability: In this blog article you will learn why we need to stop blaming a weak or “unstable” core for low back pain and why the whole idea of a weak or “unstable” core is based on outdated research ideas.
“Yeah, you have a weak core, you gotta do core stability exercises man”. If we had received one cent per time that a weak or unstable core had been blamed for a patient’s low back pain in the health or fitness industry, we would surely be millionaires by now. In this blog, we will have a look back in time to see where the idea of an unstable core came from and discuss why the concept is BS.
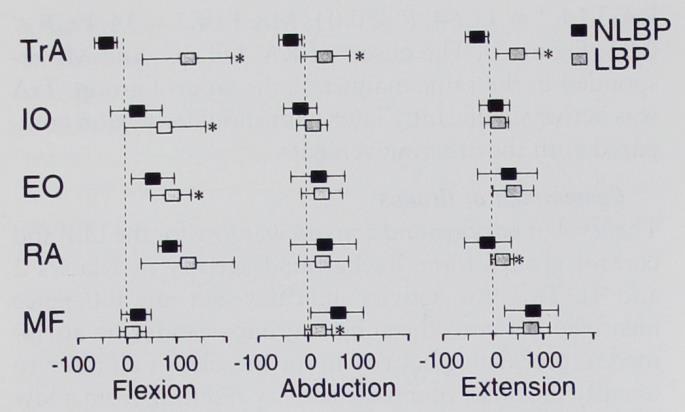
Almost 25 years ago, Hodges et al. conducted a study in which they found a delayed onset of contraction of the transverse abdominis of 50 milliseconds when patients with chronic low back pain raised their contralateral arm compared to a healthy group.
This paper has triggered the core stabilization craze that we are still seeing in the health industry today. In short, the concept was born that the deep stabilizers, namely the transverse abdominis and the multifidi would act as a corset to stabilize the lumbar segments around mid-range, which was termed „neutral zone“. In 2008, however, a study by Alisson et al. measured the transverse abdominis bilaterally and found that both sides act independently. So the left side contracts when you raise your right arm and the other way round. They concluded that the TrA does not act as a corset and that the idea of the muscle as a bilateral stabilizer needs to be revised.
Both sides of the TrA act independently, thereby questioning the concept of a “corset function”
Assessment

Anyways, let’s assume that the function of the TrA is still that of a stabilizer of the lumbar spine. While this delayed muscle onset was measured in a laboratory setting, we will have to ask ourselves if we can detect this „dysfunction“ in the clinic. In practice, the pressure biofeedback unit was invented to determine the function of the TrA and multifidi. But how accurate is this measure really? Lima et al. In the year 2012 compared the validity of the pressure biofeedback unit to electromyography and found a very poor diagnostic accuracy with both sensitivity and specificity of 60% – and then we are not talking about the delayed onset of contraction, but just A contraction of the muscles.
The pressure biofeedback unit is not a valid tool to assess TrA and multifidi function
What about movement control tests? Luomajoki et al. (2007) showed that a test battery of 6 different tests had substantial intra- and inter-rater reliability. If you’re curious about the battery, check out the video in the top right corner. While these tests are reliable, we don’t know if they are also valid: In other words, how do patients with low back pain perform these tests compared to subjects without pain? And even if there was a marked difference between groups, how do we know if those movement “flaws” are relevant to the persistence of back pain?
We know that people move differently in pain and it could very well be that this altered movement strategy is an effect rather than the cause of pain.
Treatment

But let’s continue and assume that the TrA has an important stabilizing function and that we can accurately detect patients with a delayed onset of contraction in the TrA and multifidi. What then happened in practice is that we started to perform training for those muscles in either supine or four-point kneeling position. But how is strength training gonna fix the timing issue? Lederman in 2008 compares that to trying to play to piano faster by exercising with finger weights and performing push-ups. On top of that, how is being able to perform a draw-in maneuver in a supine position going to carry over to activities of daily living? The idea to train those muscles in a supine or kneeling position with slow speed contradicts the principle of specificity and similarity or transfer. The only thing that would make sense is to train the speed of movement and hope that the system will somehow reset itself.
To overcome this issue, proponents of core stability came up with the solution to teach everyone to continuously brace their cores in order not to have to worry about onset timing. This proposal is completely abnormal and not how our nervous system works. Show me one patient who is consciously co-contracting voluntarily all the time – it’s not possible because our nervous system wants to perform a task and then organizes muscle activity to achieve that task and not the other way round. This is like driving in reverse all the time. That’s the same reason why most patients have such difficulty performing a proper draw-in maneuver. Not sure if you are like me, but I always hated to give this exercise to patients because I knew it would be super weird and over-complicated to explain this exercise to patients and they would often not be able to do it even if I tried with different cues or the pressure biofeedback unit.
At last, we’d like to add that increased co-contraction of the trunk muscles happens involuntarily in a lot of patients with low back pain. The low back pain researcher Kjartan Vibe Fersum said the following (and we stole this from Jarod Hall’s lecture on the topic by the way) „If people in pain walk like a plank, maybe don’t put them in a plank“.
If people in pain walk like a plank, maybe don’t put them in a plank – Kjartan Vibe Fersum, Back pain researcher
To make the story short, research has then also shown that training does not improve feed-forward activation of deep abdominal muscles (Vasseljen et al. 2012, Allison et al. 2012)
Okay, so now let’s say that unless all that we’ve stated earlier, we would be able to change the onset timing of the TrA and multifidi – does it even matter?
Credits to Jarod Hall again for assembling the following list of studies who have shown that:
- No association between change in onset an LBP (Vasseljen et al. 2012)
- Spine stabilization exercises in the treatment of chronic low back pain: a good clinical outcome is not associated with improved abdominal muscle function (Mannion et al. 2012)
- Wong et al. (2014) – systematic review: changes in morphometry or activation of transversus abdominis following conservative treatments tend not to be associated with the corresponding changes in clinical outcome
If we look a bit broader than just the TrA or multifidi Steiger et al. (2012) performed a systematic review looking at different target aspects of performance and their influence on treatment outcomes for low back pain. They found that the treatment effects could NOT be attributed to any change in the musculoskeletal system such as mobility, strength, or endurance.
This was to expect because there are no simple solutions to complex problems. Back pain is multi-factorial and research has shown that psychosocial factors like depression, anxiety, movement-related fear, coping, workplace satisfaction, etc. All influence the prognosis.
So to sum it up: 1) The TrA does probably not have a corset function to stabilize the spine. 2) We are not able to accurately assess TrA or multifidi function in practice. 3) Slow strength training for the TrA or multifidi does not transfer to onset timing of contraction of those muscles and research also shows that it’s not possible to alter onset timing. 4) Neither onset timing, nor strength or endurance of the TrA and multifidi are relevant for a positive outcome. If you are a regular follower this sounds a hell lot like the myth-busting we did for scapular dyskinesis, right? For all of those reasons, the very same researchers who have come up with the concept like Hodges or who have build research on this concept like Peter O’Sullivan or Chad Cook have all moved on. If they have abandoned the concept of core stability – and remember for some it was a huge part of their professional career – so can you!
Orthopedic Physiotherapy of the Spine
Master Treating Spinal Conditions in Just 40 Hours Without Spending Years of Your Life and Thousands of Euros – Guaranteed!
But we’re not completely done yet and we ask you to keep reading a little bit longer. Despite all of the reasons we have mentioned, low-load motor control exercises do seem to be effective to improve low back pain. There is tons of research that compared core stabilization exercises with general strengthening exercises for the low back. Some of these studies by Smith et al. (2014), Saragiotto et al. (2016), Luomajoki et al. (2018), Wang (2012), Coulombe (2017) amongst others show that low-load stabilization exercises might be a tiny bit better at reducing pain at short-term but all of them show that general strengthening is equally effective at long-term.
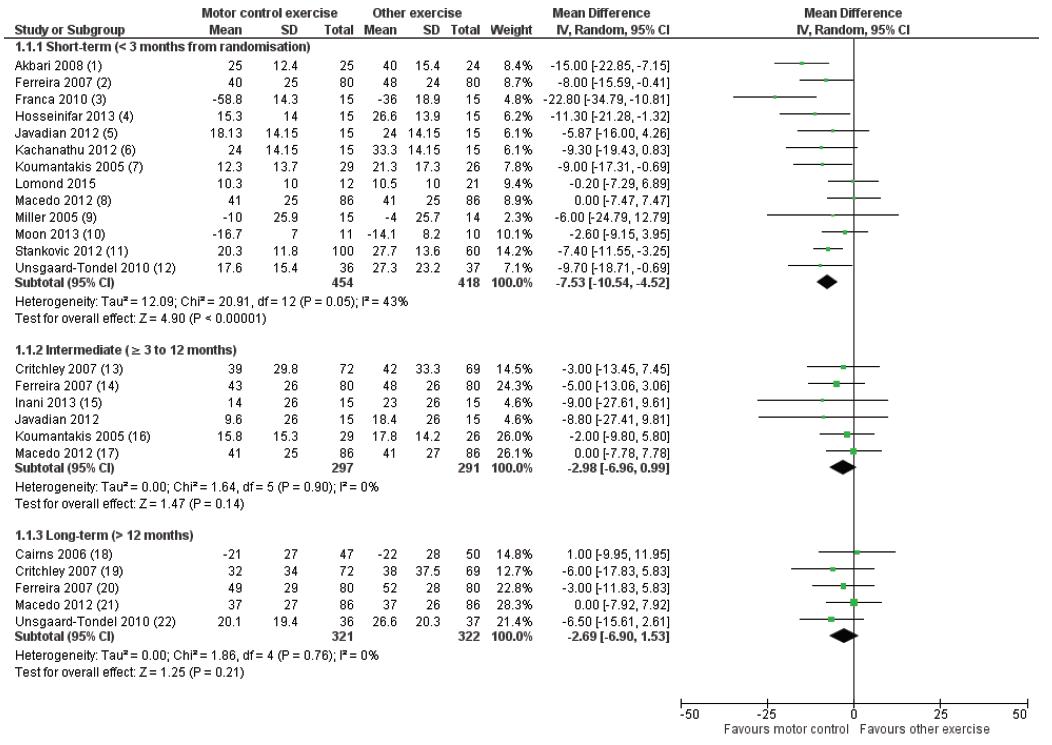
So while core stability is not the holy grail, it still is an option for rehab. However, this is not because the deep lumbar muscles are trained to fix an unstable spine. We think they work because they are useful especially at the beginning of a progressive loading program of the spine. Similar to other exercise programs, the positive outcome is likely to be explained by aspecific effects such as diffuse noxious inhibitory control, the release of pain-reducing chemicals in your brain, maybe just more movement in itself, or psychosocial factors such as decreased movement-related fear, increased confidence, etc., but in fact: We just don’t know really!
So leaving out the awkward draw in maneuvers, it’s okay to train your pelvic tilts, dead bugs, bird dogs, Waiter’s bow, and so on. But do them with the idea of a gradual loading program and not with the idea to selectively activate deep muscles to stabilize the spine. If the concept of an unstable spine is explained to a patient it can do a lot of harm and create unnecessary worry and fear-related movement.
Okay, this was a bit of a longer blog on the myth of core stability. More content like this on the spine can be found on our online course “Physiotherapy of the Spine“. Thanks a lot for reading!
Kai
References
Jarod Hall’s Video on Back Pain and Core Stability: https://www.youtube.com/watch?v=LdukopYcBtk

Kai Sigel
CEO & Co-founder of Physiotutors
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







