The Absolute NO.1 Exercise for Chronic Low Back Pain

We have probably click-baited you into reading this blog post because you might be looking for THE magic exercise or FIX to make low back pain magically disappear. The truth is: There is none and can never be one single exercise that is the best for low back pain or any other hurtful body part or muscle whatsoever. In fact, this way of thinking is very simplistic and focuses on a body part or pathology rather than the person. If there was 1 best exercise our profession would basically become redundant and patients could follow cookie-cutter approaches.
There can never be one best exercise for every person. If this exercise existed, our profession would become redundant.
But let’s first look at the effectiveness of different forms of exercise for patients with low back pain:
First of all, a meta-analysis by Searle et al. (2015) has shown that strength and resistance exercises, as well as coordination/stabilization exercises, are effective in reducing pain in patients with chronic low back pain although effect sizes are usually rather small. So that’s pretty good news, now let’s look a bit closer at different exercise programs and their effectiveness:

A study by Marshall et al. (2013) compared Pilates exercises with stationary biking and while Pilates was superior at 8 weeks, the results were equal in the long term at 6 months.

Then there is this pretty well-known study by Shnaydermann et al. (2013) who have found that walking is as effective as specific exercises for the low back at 6 weeks. It has to be mentioned though that the people in the study were all sedentary, so we cannot assume that the outcome would be the same in a more active population.
Furthermore, there is tons of research that compared core stabilization exercises with general strengthening exercises for the low back. Some of these studies by Smith et al. (2014), Saragiotto et al. (2016), Luomajoki et al. (2018), Wang (2012), Coulombe (2017) amongst others show that low-load stabilization exercises might be a tiny bit better at reducing pain at short-term but all of them show that general strengthening is equally effective at long-term.

At last, a study by Aasa et al. (2015) compared low-load motor control exercises with deadlifts. In the study, the low-load motor control group outperformed the high-load group on short-term, but again- long-term results were equally effective. So the good news from all of these studies is that doing something is better than nothing. So one might argue that the best exercise is the one that gets done.
But why choose one form of exercise only?
Ben Cormack from Cor-Kinetic compares different exercise modes to different vitamins that our body needs just like in a balanced diet. So you might want to incorporate strength, high-load and low-load, coordination, power, endurance, and graded exposure exercises as well as movement games, etc. into a well-balanced exercise program.
Glasgow et al. (2015) thus also mention that an optimal loading program consists of different key variables and mechanisms.

One thing we know from research is that patients with low back pain often display decreased movement variety. So using different exercise modalities might be one way to increase movement variability. What is very interesting is that we are always thinking that getting stronger, more flexible, better at activating certain muscles, or improving movement “faults” etcetera is what explains the effects of our exercise program. However, a systematic review by Steiger et al. (2012) has shown that treatment effects are NOT attributable to changes in the musculoskeletal system.
Treatment effects are NOT attributable to changes in the musculoskeletal system (Steiger et al. 2012)
There might be other changes that are responsible for the effects such as diffuse noxious inhibitory control, the release of pain-reducing chemicals in your brain, maybe just more movement in itself, or psychosocial factors such as decreased movement-related fear, increased confidence, etc., but in fact: We just don’t know really!

So how specific should we be? Aspecific problems such as aspecific low back pain probably do not have to be body-part or structure-specific, but also benefit from a more general approach. On the other hand, a specific problem such as Achilles tendinopathy, in which we know the nociceptive structure, will benefit more from a structure-specific approach such as load on the Achilles tendon by calf raises for example.
But even if we have a structure-specific problem, we should not only be specific to a certain joint, tendon, or muscle, but specific to the person in front of us!
Aspecific problems do not need a structure-specific approach, while body-specific problems will probably need a more structure-specific approach
Research always looks at the average effect of a group with two or more very standardized interventions. However, the person in front of you could deviate from this standardized mean. For example, isometric exercises generally work well to decrease pain. At the same time, research has shown that exercise-induced analgesia might not occur in patients with central sensitization but actually increase pain levels. This means that we will always have to be flexible and adapt our treatment if it does not seem to be effective in our patients after 2 or 3 sessions, even if research might suggest otherwise.
Another big reason that there can never be THE single best exercise for every person is that different people need different amounts of vitamins. So what you’ll have to ask yourself with every exercise you’re giving to patients is what do you want them to get from this exercise?
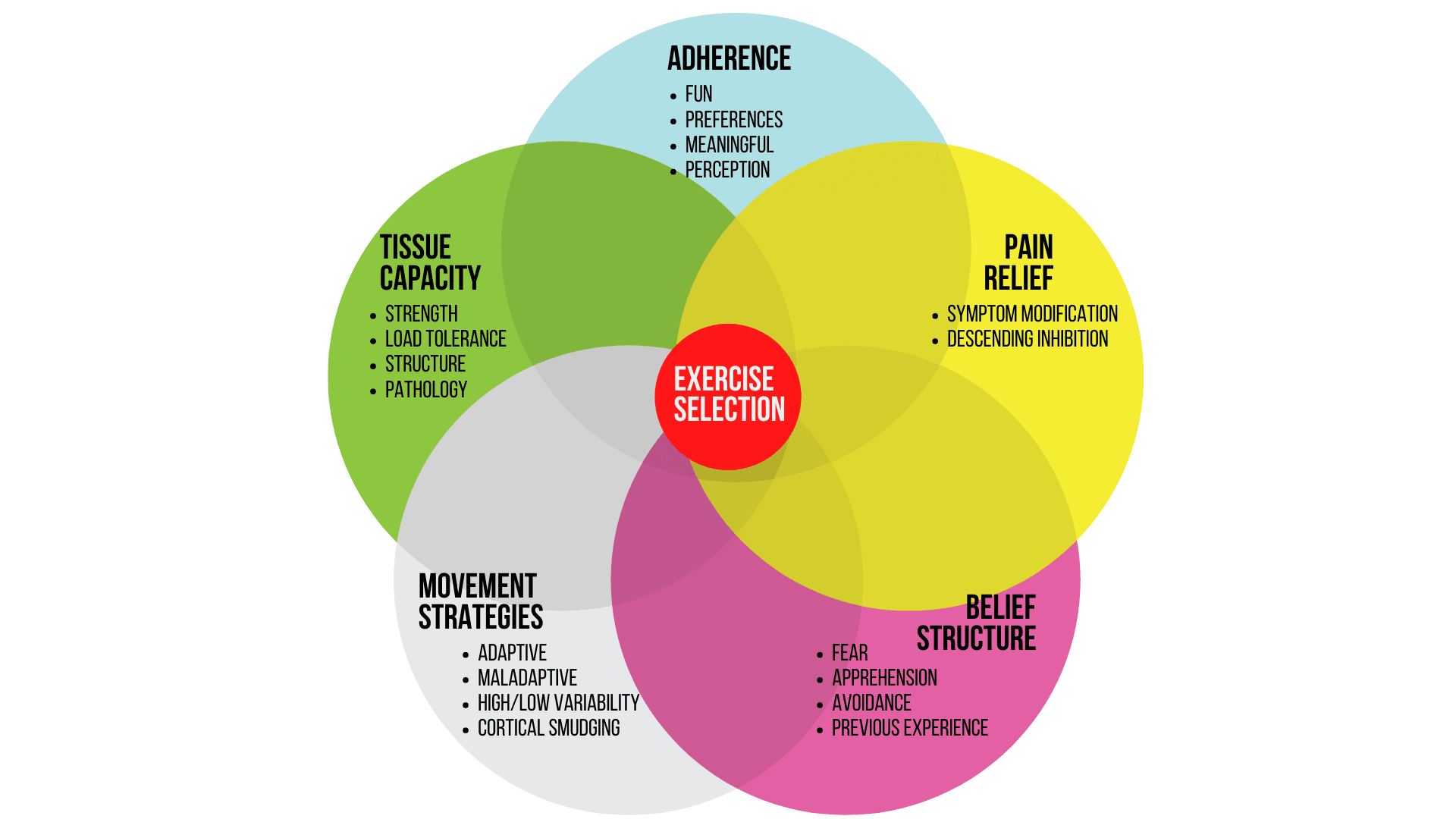
It could be that you are trying to increase tissue capacity or exercise adherence. Another target could be to challenge their belief structure or to alter their movement strategies or it could be pain relief. On top of that, the ideal exercise is tailored to a patient’s level of skill and irritability.
All of these different areas should influence exercise selection to make it person-specific!
For example, a young weightlifter who has to return to high-level performance after the first episode of low back pain might need maximum strength, power, and work on his technique. On the other hand, a 70-year-old sedentary pensioner with chronic low back pain and apprehension to bend forward due to maladaptive illness beliefs will probably need a graded exposure program with lots of reassurance and education.
Orthopedic Physiotherapy of the Spine
Master Treating Spinal Conditions in Just 40 Hours Without Spending Years of Your Life and Thousands of Euros
For the very same reasons, we cannot expect that generic exercises will lead to optimal outcomes. The challenge for us as therapists is to listen to our patient’s story and to ask ourselves which vitamins he or she needs and then select the appropriate exercises to give them these different vitamins.
Alright, this was our blog on “the best exercise for low back pain”. Shout-out at this point to Ben Cormack from Cor-Kinetic who inspired us to discuss various concepts in this blog. If you want to know how we apply these concepts in different exercise programs check out our online course “Orthopedic Physiotherapy of the Spine“
Thanks a lot for reading, bye!

Kai Sigel
CEO & Co-Founder of Physiotutors
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







