Feasibility of Heavy Slow Resistance Training in Gluteal Tendinopathy

Introduction
Gluteal tendinopathy (GT) is a common source of lateral hip pain (LHP), particularly in middle-aged women, affecting up to 24% of this population. It is associated with reduced hip abductor strength, gluteal muscle atrophy, and significant impairment in daily function and quality of life.
Exercise therapy is currently the primary treatment for tendinopathy management. Exercise targets muscle strength deficits and associated atrophy, promotes tendon remodeling, and can provide an analgesic effect. Among different forms of exercise, heavy slow resistance training appears to be recommended. Patient education is combined with exercise, aiming to reduce tendon compression and high, provocative tensile load through postural and movement modification.
While this approach of education and progressive strengthening is effective in a lot of tendinopathy-related pathologies (such as Achilles tendinopathy and lateral elbow tendinopathy) not much is known about the effectiveness in gluteal tendinopathy, as the use of heavy slow resistance training is unexamined. Moreover, a lot of people and clinicians are worried about provoking the tendon-related pain by applying high-load strengthening exercises. Therefore, this study was conducted as a feasibility study to evaluate the potential effectiveness of heavy slow resistance training in gluteal tendinopathy and to evaluate the potential related side effects.
Methods
A single-group, 12-week feasibility trial was conducted, recruiting participants with clinically diagnosed gluteal tendinopathy. All sessions were supervised by trained sports science students under the guidance of the principal investigator.
Adult participants with lateral hip pain of at least 6 weeks were included when they reported tenderness over the greater trochanter, and pain provocation by the 30-second single-leg stance and resisted abduction tests. They had to have a full and normal passive hip range of motion (ROM). Candidates were excluded if they had hip osteoarthritis, a suspected tendon rupture following acute traumatic lateral hip pain, a persistent Trendelenburg sign during the 30-second single-leg stance, a recent (<6 weeks) corticosteroid injection, prior heavy slow resistance training within the past six months, systemic diseases affecting the muscular or nervous system, a hip replacement or planned surgery on the affected side, pregnancy, or a body mass index (BMI) greater than 40.
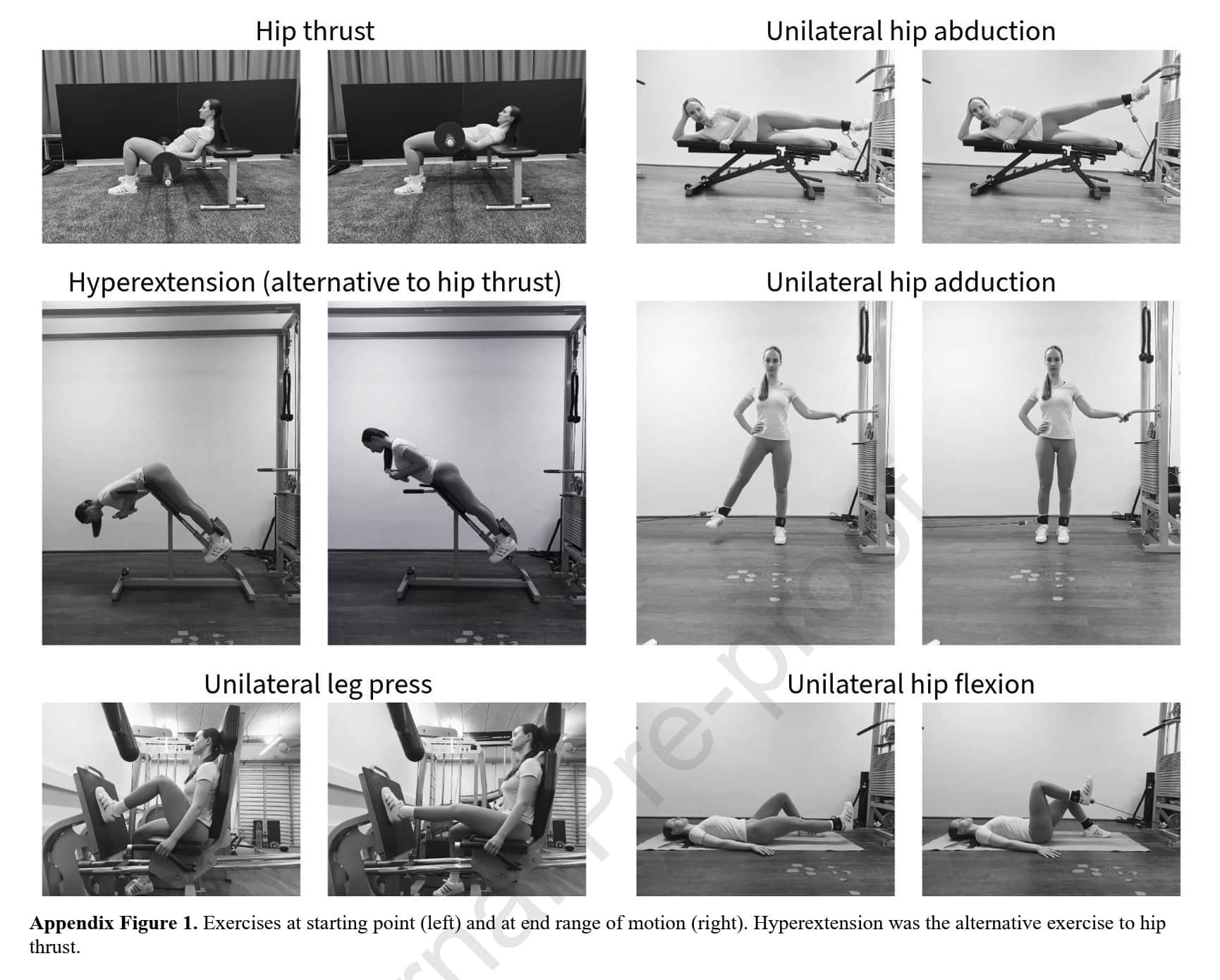
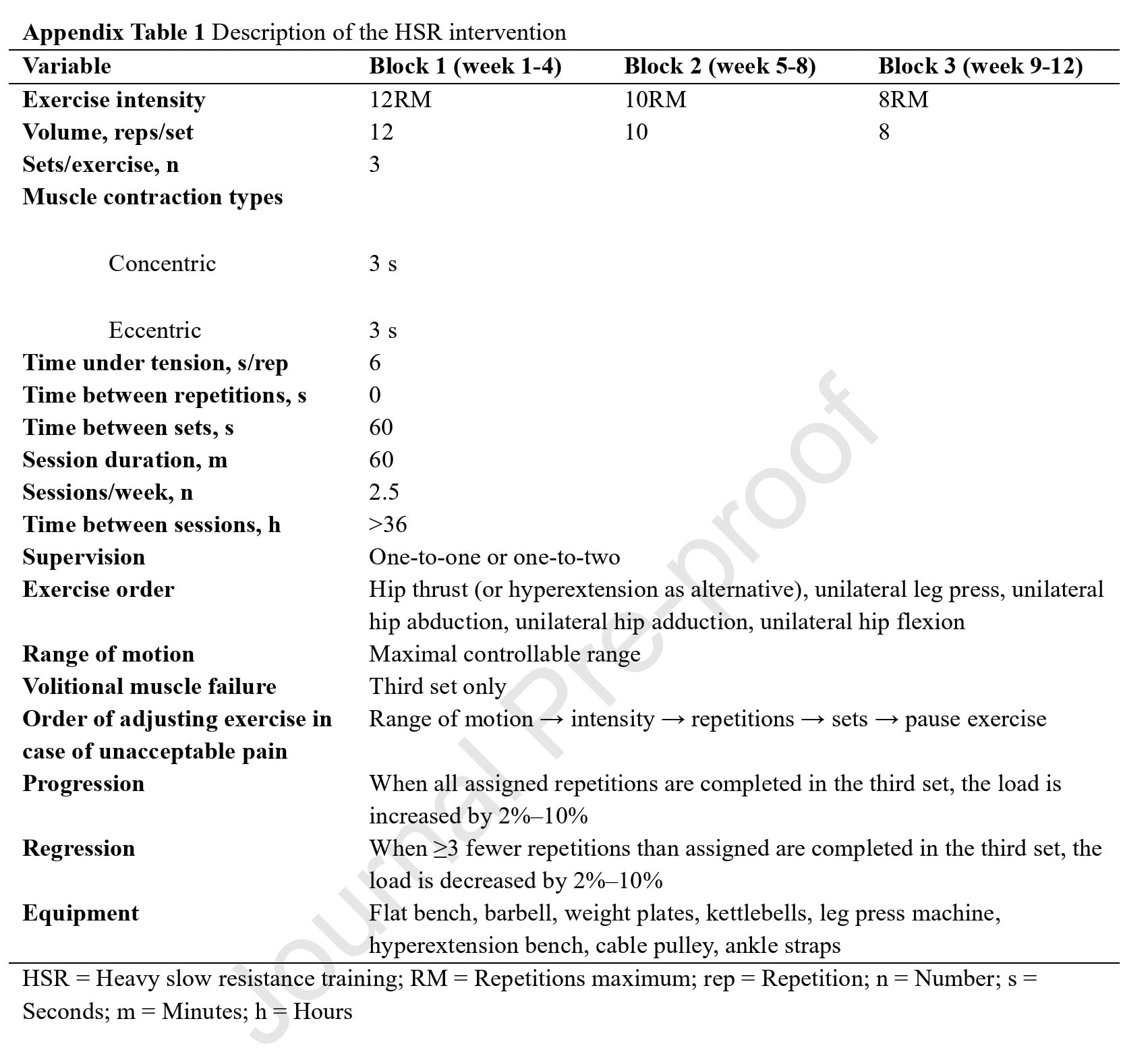
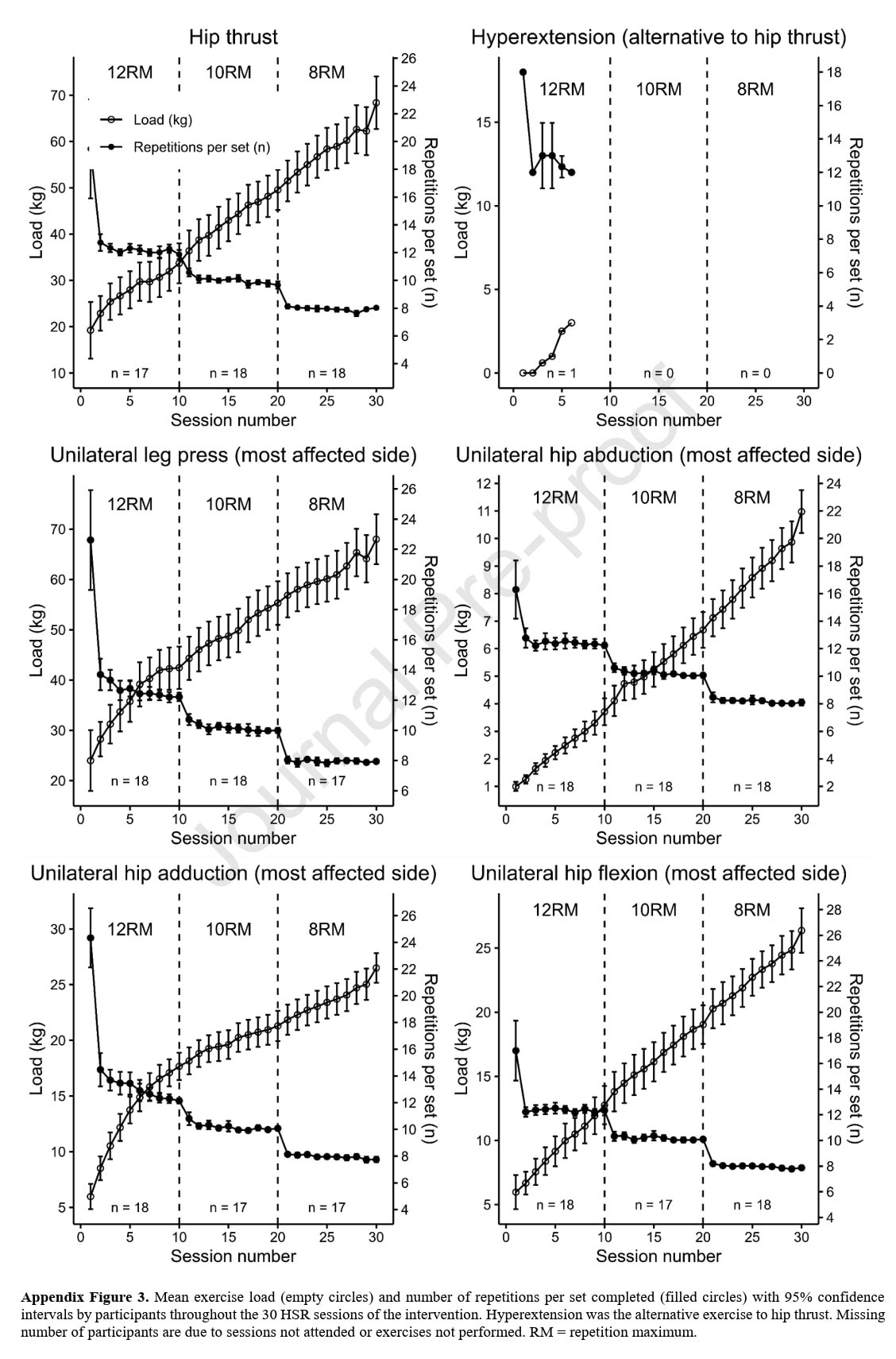
The intervention group participated in heavy slow resistance training for 30 sessions over 12 weeks. Each session started with a 10-minute submaximal warm-up on a cycle ergometer with an intensity of 11–12 on Borg’s rating of perceived exertion scale (RPE). After finishing the warm-up, the following 5 exercises were completed.
- Hip thrust (or hyperextension as an alternative)
- Unilateral leg press
- Unilateral hip abduction
- Unilateral hip adduction
- Unilateral hip flexion
These exercises were chosen as they address all major muscles of the hip, with a focus on agonistically or synergistically activating the hip abductors, according to the authors. Unilateral exercises were performed on both sides, starting with the most affected hip.
The intervention group followed the following training structure.
- Weeks 1–4: 3 × 12 RM. The first session served as a baseline where the starting loads were determined. In the following session, the load was increased to reach the desired 12RM.
- Weeks 5–8: 3 × 10 RM
- Weeks 9–12: 3 × 8 RM
Participants were instructed to perform the exercise with a 3-second concentric and 3-second eccentric contraction, ensuring 6 seconds of tension. Every third set was performed to volitional muscle failure. Loads were progressed linearly; if all requested repetitions (or more) were completed, the loads were increased by 2–10%. Likewise, loads were decreased by 2-10% if not all repetitions were possible. For the unilateral exercises, the loads were determined based on the most affected hip.
Adjustments followed a regression protocol if pain became intolerable: first, the range of motion was adjusted, but if that did not relieve the pain, the intensity, repetitions, or sets were altered (in that order). If none of these adjustments could decrease the pain, the exercise was paused. The same adjustments were made in case the participant reported unacceptable pain before or 24 hours following the session.
This feasibility trial of heavy slow resistance training in gluteal tendinopathy was supplemented with an educational part. The participants were educated on the nature of gluteal tendinopathy and what the management consisted of. They received written and oral information emphasizing:
- Avoiding hip adduction postures that increase tendon compression (cross-legged sitting, side-lying on affected side, standing with a hinged (adducted) hip)
- Sleep modification (pillow between knees, lie on unaffected side)
- Activity pacing (avoid prolonged walking, stair climbing, or leg crossing, avoiding stretches that involve pulling the leg across the mid-line of the body)
These strategies were reinforced throughout the HSR program.
Outcomes
The primary outcome measures consisted of feasibility outcomes:
- Session adherence (≥80% = “high”)
- Content adherence (≥80% of prescribed sets performed)
- Drop-outs, adverse events (AEs), and serious AEs (SAEs)
- Lateral hip pain tolerability before, during, and 24 h after sessions. This was assessed using the Pain Tolerability Questionnaire.
Secondary outcomes consisted of clinical outcomes for tendinopathy research:
- Lateral hip pain intensity at night over the past week, worst pain at night, and worst pain over the past week were measured using the NRS 0–10. The proportion of time with lateral hip pain over the past week was captured using the 0-100 NRS.
- VISA-G was used to measure function and the severity of disability in people with gluteal tendinopathy
- Pain Self-Efficacy Questionnaire (PSEQ): assessed self-efficacy in performing activities despite being in pain
- EQ-5D-5L measured health-related quality of life across five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression
- 9-step Stair Climb Test (9-SCT): The time in seconds to safely ascend and descend a flight of 9 steps (step height 17 cm) without a handrail was measured.
- 30-second Chair Stand Test (CST)
- Isometric hip muscle strength: Maximal isometric torque was assessed bilaterally for hip abductors, flexors, and extensors using an isokinetic dynamometer. Two submaximal trials were allowed (at approximately 50% of the MVIC) after which 3 consecutive maximal voluntary isometric contractions (MVICs) were performed. Participants were instructed to push as hard and fast as possible against the dynamometer arm for 5s. Standardized verbal encouragement was provided. Trials were interspersed by a 30s rest period. The trial with the highest peak torque was used for analysis. Dynamometer arm length and rotation axis height were standardized intra-individually across legs and testing sessions
- Hip abduction was tested side-lying with the active leg in 10° abduction, the greater trochanter aligned with the dynamometer rotation axis, and the passive hip in 45° flexion. The edge of the dynamometer arm pad was aligned with the superior border of the patella at full knee extension.
- Hip flexion and extension were tested supine with the active hip in 45° flexion, the greater trochanter aligned with the dynamometer rotation axis, and the back inclined 15°.
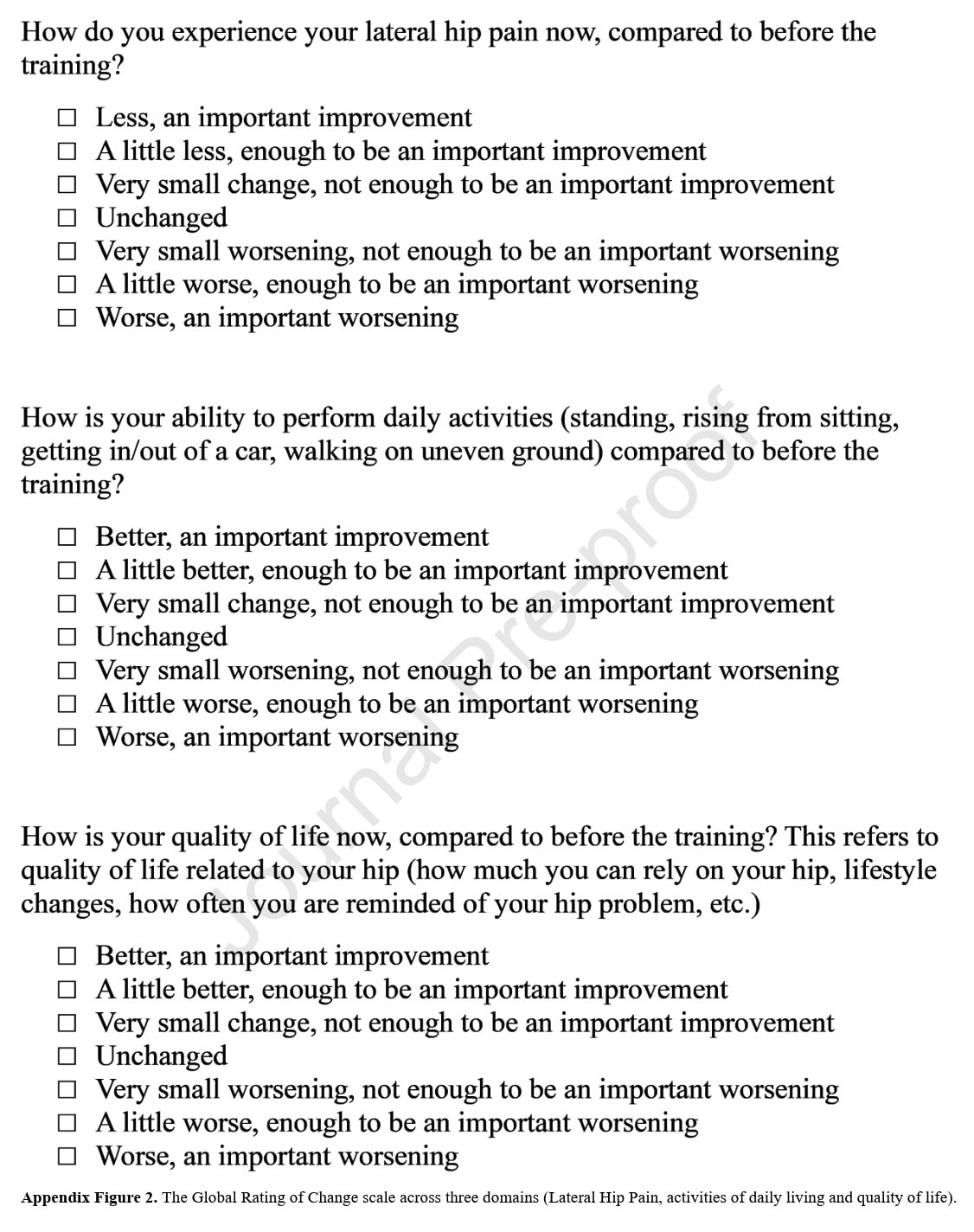
- Global Rating of Change (GRoC): see the figure displayed under.
Results
This feasibility trial studying heavy slow resistance training in gluteal tendinopathy was able to include 19 participants (79% women, mean age 52 ± 7 years). Their BMI was 26.6 kg/m2. Their usual hip pain was 5.1 out of 10 on the NRS, 58% reporting unilateral lateral hip pain and 42% reporting bilateral lateral hip pain. The symptom duration varied between participants, but was present for longer than 1 year for the majority of the participants. Their data is detailed in the table below.
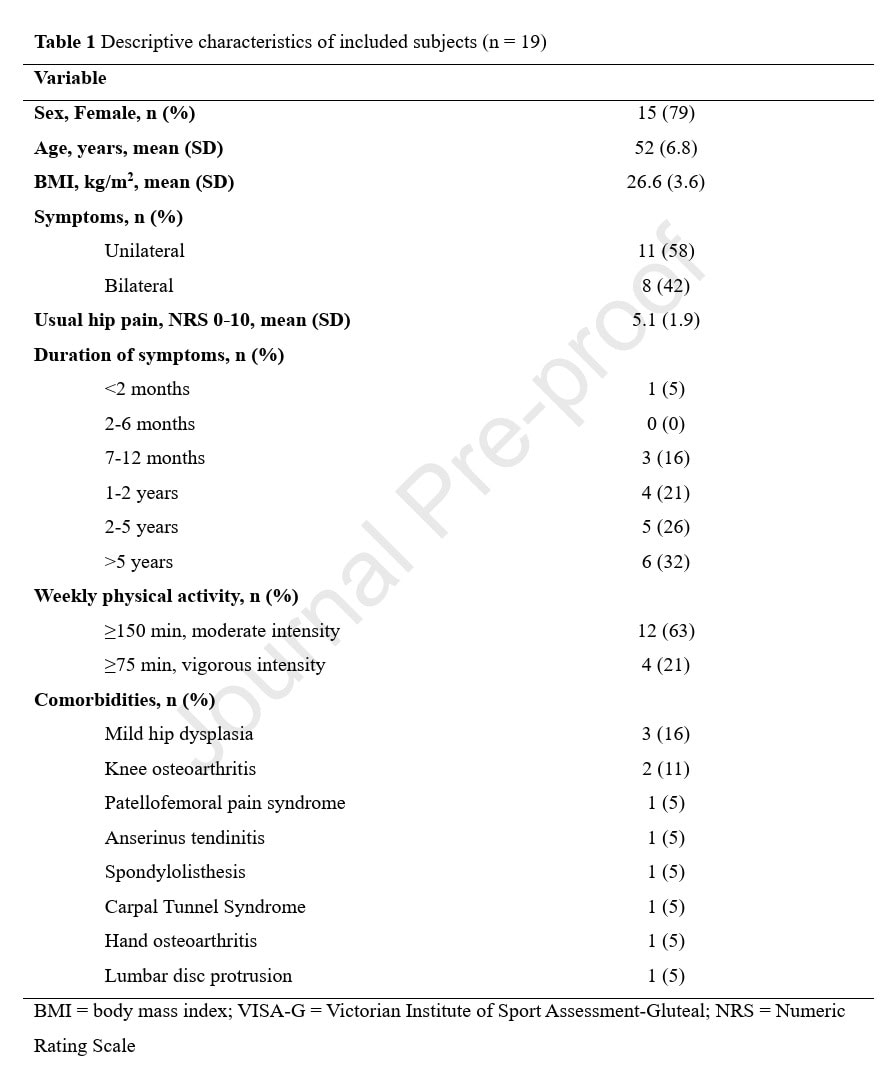
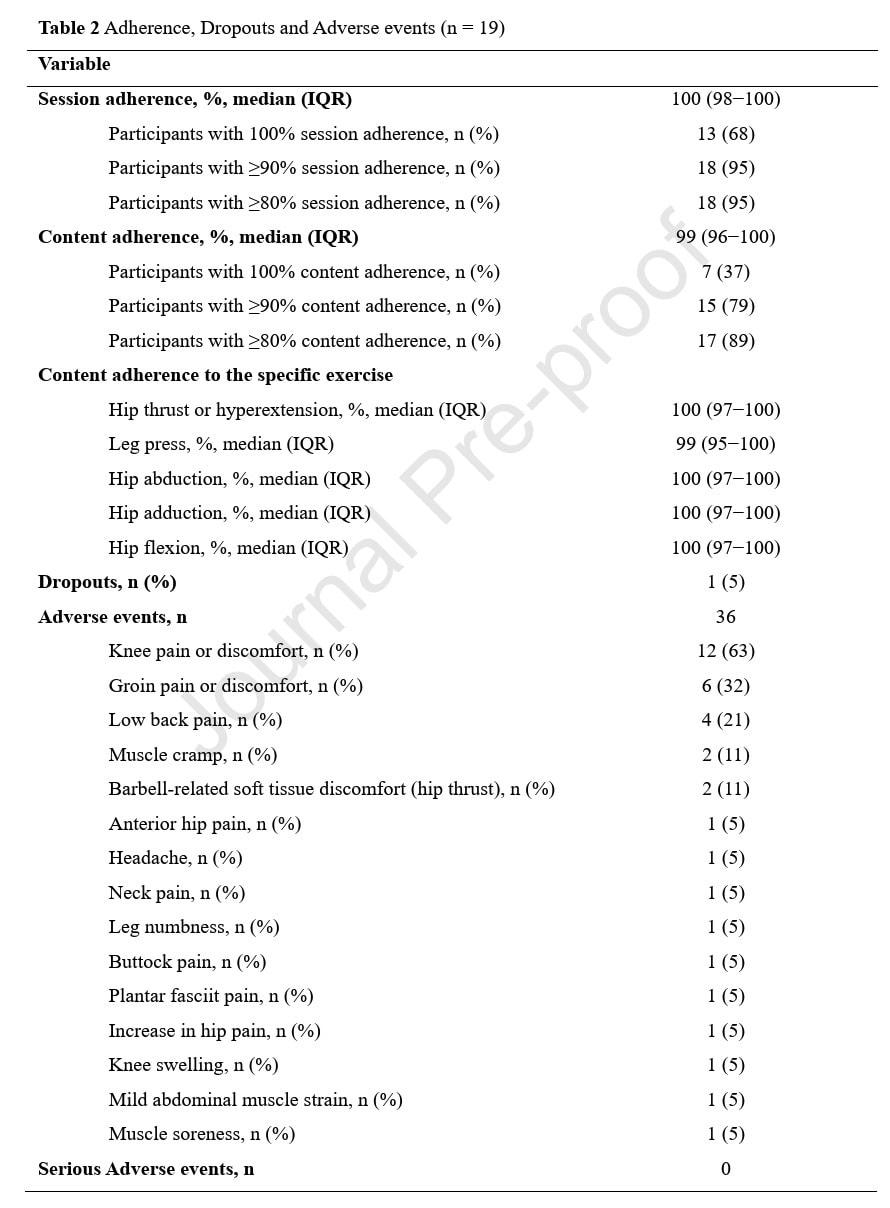
In terms of feasibility, high session and content adherence were noted: 95% of participants demonstrated 90% or better session adherence, and 89% of participants reached 80% or more content adherence.
The number of participants dropping out was low, only 1 participant (accounting for 5%), but this was unrelated to the intervention. No serious adverse events were reported. Some minor adverse events were mostly linked to knee or groin pain or discomfort, or low back pain. The authors reported that the knee and groin pain or discomfort were primarily associated with the hip adduction and leg press exercises, but that it was transient and decreased after correction of the exercise technique or within a few sessions after applying the regression protocol.
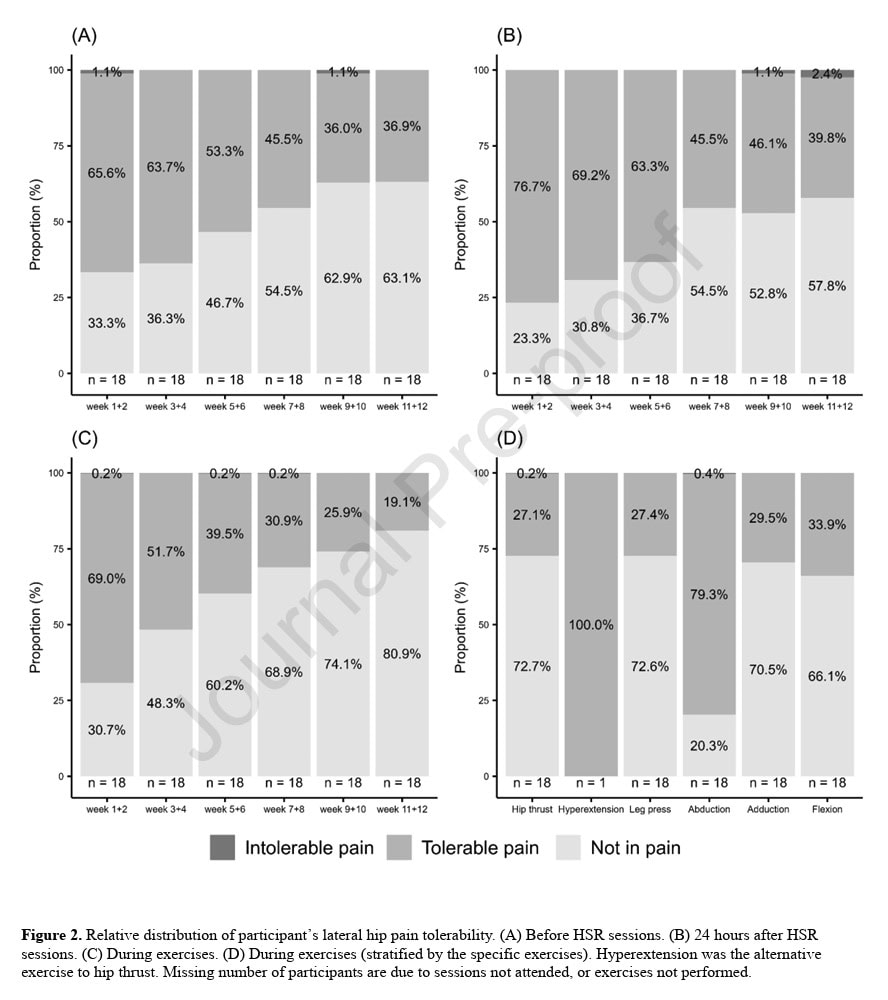
The pain tolerability was assessed by asking whether or not the participant had no pain or tolerable pain. At all timepoints (before, during, and 24 hours after heavy slow resistance training sessions), the participants reported 100% pain tolerability. Over the weeks, there was an increase in the proportion of participants reporting a shift from “tolerable pain” to “not in pain”, as can be seen in the figure below.
Among the different exercises, the hip abduction exercise was most frequently associated with tolerable pain, whereas the hip thrust, leg press, adduction, and flexion exercises were mostly causing no pain during the exercise execution. Only 1 participant performed the hyperextension exercise as an alternative to the hip thrust exercise.
Secondary outcomes concluded that 95% of the participants reported an important improvement in lateral hip pain, as measured by the GROC after the intervention. Eighty-four percent reported an important improvement in activities of daily living, and 95% reported an important improvement in quality of life.
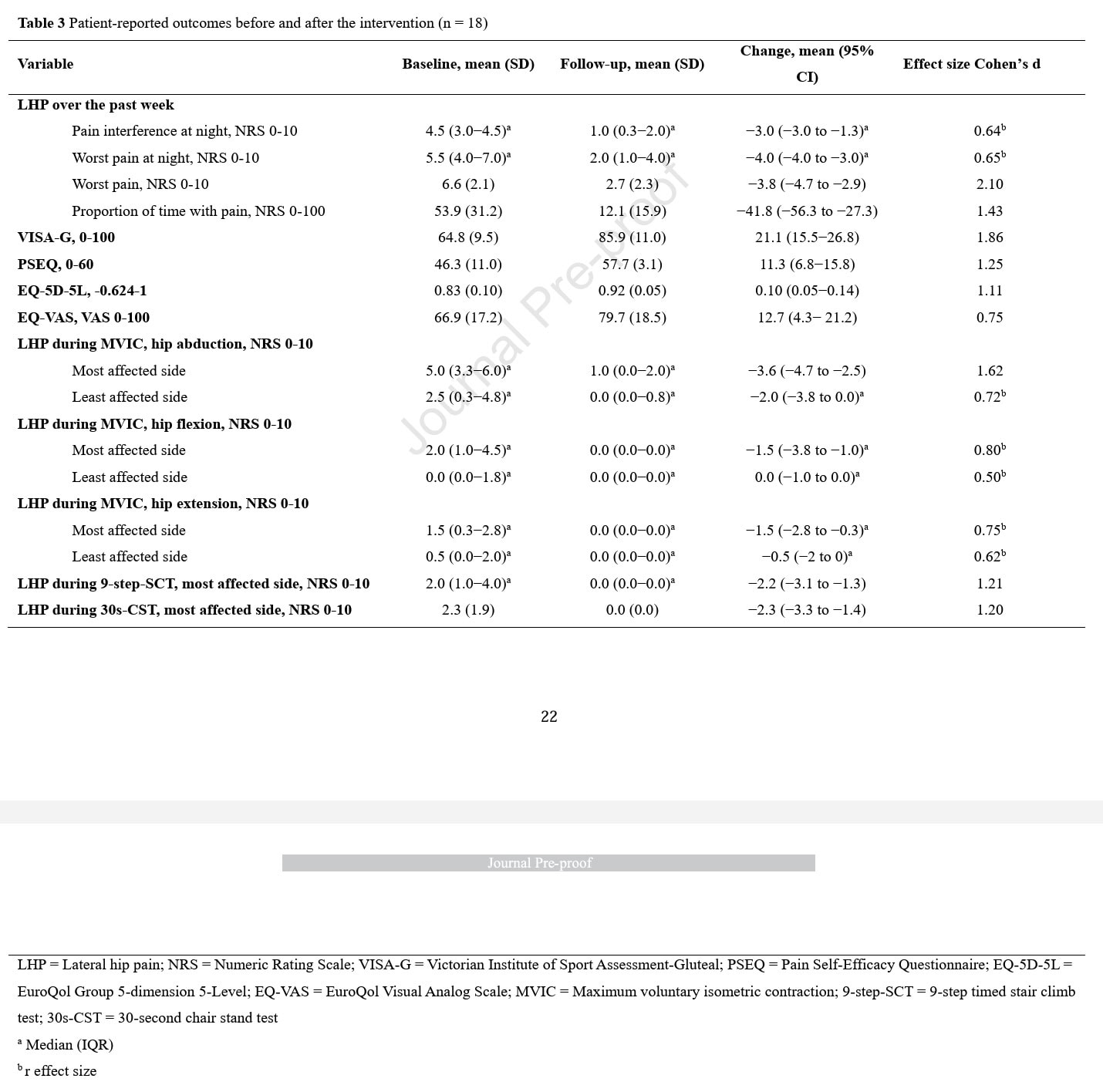
The pain scores before and after the training program were compared. Large effect sizes were observed for:
- A decrease of 3.8 points in “worst pain”.
- A decrease of 41.8 points in the “proportion of time with pain” reported from 0-100.
- An improvement of 21.1 points on the VISA-G questionnaire
- An increase of 11.3 points in pain self-efficacy (PSEQ)
- An improvement of 0.10 in quality of life (EQ-5D-5L)
The authors further specified that sixty-eight percent of the participants reported a decrease in nighttime lateral hip pain interference of 2 points, which is considered the minimally clinically important difference. Seventy-nine percent had a decrease of 2 points for “worst pain at night”, eighty-nine percent for “worst pain”, and seventy-nine percent for “proportion of time with pain”. The VISA-G changed from 64.8 points at baseline to 85.9 at follow-up, consistent with a mean 21.1 point improvement.
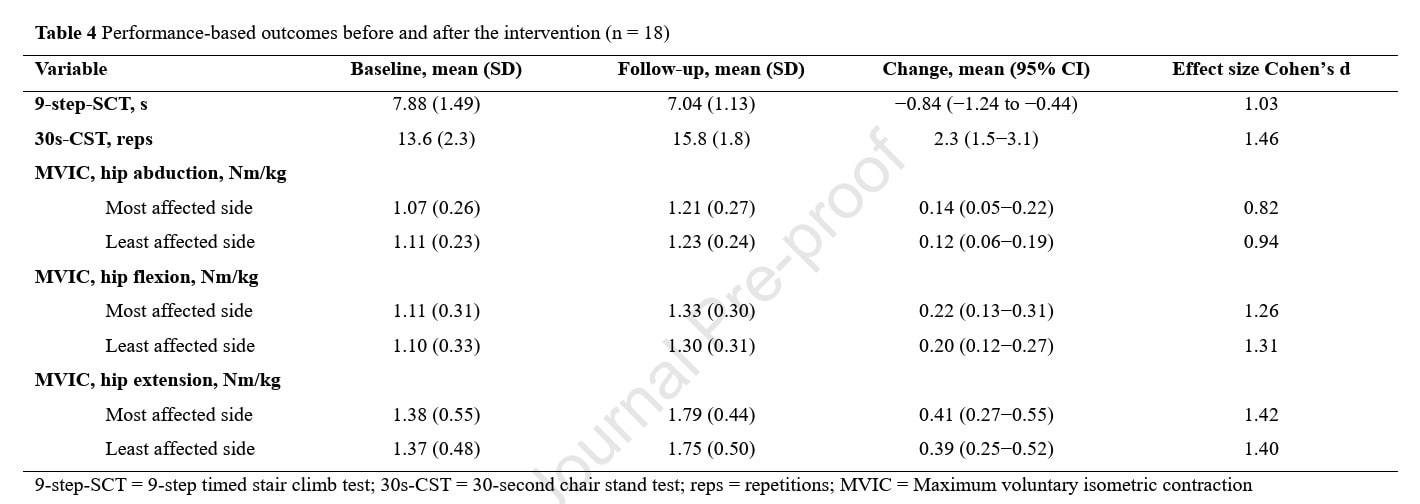
Regarding the functional tests, the following observations were made and supported by large effect sizes:
- A decrease of 0.84 seconds in the time needed to complete the 9-step-SCT
- An increase of more than 2 repetitions in the 30-second chair stand test
- Significant gains in maximal voluntary isometric contraction strength across all directions
Questions and thoughts
We must remain cautious about the current observations, as this was a single-group uncontrolled feasibility trial. Therefore, only the feasibility outcomes can be interpreted with confidence. Feasibility was demonstrated by the low number of adverse events, the absence of serious adverse events, and the high content and session adherence. Participant recruitment, however, may be a challenge since only 12% of screened participants were eligible for inclusion. It must be acknowledged that, since the recruitment of participants was done through social media, selection bias of highly motivated participants took place. The low drop-out rate, on the other hand, seems promising.
All effectiveness outcomes should be tested in future RCTs, where comparisons can be made between placebo groups and groups performing heavy slow resistance training in gluteal tendinopathy. Some of the secondary pain-related and functional outcomes showed promising results, in terms of effect size and improvement exceeding thresholds for clinically relevant differences. It remains uncertain, however, whether similar levels of adherence and compliance can be replicated in actual physiotherapy settings. This is due to the often-lower supervision in real-world practice compared to this trial, which benefited from the guidance of three sports science students during the interventions.
The educational component of the trial, which focused on gluteal tendinopathy, particularly caught my attention. A significant portion of the information discussed avoiding specific postures and activities. While preventive measures are ideal, this approach struck me as potentially nocebo-inducing. This could exacerbate participants’ fears and anxieties, reinforce avoidance behaviors, and ultimately lead to negative outcomes. I may be mistaken, but there was no mention of these posture and activity modifications being temporary.
A remark can be made for the unilateral exercises, where the loads were determined based on the most affected hip. This could have potentially underloaded the non-affected hip in those participants affected bilaterally.
Talk nerdy to me
The study’s design demonstrates strong adherence to TIDieR and CERT reporting, ensuring high replicability. A linear load progression, mirroring classical strength training periodization with 8–12 RM over 12 weeks, was employed to optimize tendon adaptation. The exercise loads were progressively increasing over the weeks, ensuring treatment fidelity.
Furthermore, the study reported moderate to large effect sizes (Cohen’s d > 0.8). However, these effect sizes may be inflated due to the small sample size. The Pain Tolerability Questionnaire, which asks “Is your pain tolerable?”, was used for pain assessment. While this pragmatic measure is well-suited for tendinopathy rehabilitation, it may be subject to social desirability bias, as participants might feel pressured to provide a positive response when confronted with such a direct question.
A significant limitation of the study is the absence of a control group or blinding. Consequently, the observed improvements cannot be definitively attributed solely to the High Slow Resistance (HSR) and educational intervention (EDU) combination.
Take-home messages
Heavy slow resistance training in gluteal tendinopathy combined with education appears to be a safe, feasible, and well-tolerated intervention for patients with gluteal tendinopathy. Participants showed excellent adherence. Secondary outcomes, although not the scope of this feasibility trial, demonstrated significant clinical improvements in pain, function, and strength, with no serious adverse events reported, even under high-load isotonic conditions. However, the study’s small, non-controlled design limits the ability to draw causal inferences, and the high level of supervision and motivated participant sample may lead to an overestimation of real-world outcomes.
Reference
