Greater Trochanteric Pain Syndrome | Diagnosis & Treatment

Greater Trochanteric Pain Syndrome | Diagnosis & Treatment
Introduction
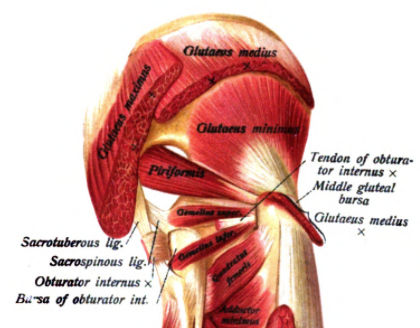
Gluteal tendinopathy or greater trochanteric pain syndrome (GTPS) describes lateral hip pain originating from irritation of the tendons of the gluteus medius and minimus. It used to be called trochanteric bursitis though the nomenclature has changed as more evidence from radiological, histological, and surgical studies emerged that showed non-inflammatory changes to the tendons rather than inflammation of the bursa (Grimaldi et al. 2016).
Generally speaking, tendons that experience normal and regular load are in a state of homeostasis; slightly greater than normal load will lead to a net anabolic biological response which results in increased tensile strength and favors the tendon’s load-bearing capacity.
A sedentary person may not induce these net anabolic responses through regular tendon loading and being overweight requires more load-bearing capacity, which may induce catabolic biological responses and reduce the tensile strength of the tendons.
On the other hand, a very active person who repeatedly puts the tendon under loads much greater than normal without adequate recovery time hinders the tendon to adapt appropriately and can lead to the development of tendinopathy (Magnusson et al. 2010).
Epidemiology
Gluteal tendinopathy is considered to be the most common tendinopathy of the lower extremity and is most prevalent in women over the age of 40 (Albers et al. 2014, Segal et al. 2007). Typical patients tend to be rather sedentary and overweight, though the condition can also be encountered in athletic populations, specifically runners (Del Buono et al. 2012).
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN – FOR FREE!

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
According to Grimaldi et al. (2015), the hallmark symptom of the condition is moderate to severe pain and tenderness over the greater trochanter with possible radiation into the lateral thigh. Sleeping on the affected leg is difficult, which impairs sleep quality. Prolonged sitting and subsequent rising up from the seated position are painful, especially from low sitting positions, where the hip is flexed beyond 90°. This is due to the fact that tensile and compressive forces of the tendons around the greater trochanter are higher in these positions.
Physical Examination
Grimaldi et al. (2016) conducted a diagnostic accuracy study on different diagnostic tests that were contrasted to MRI findings indicative of gluteal tendinopathy.
Grimaldi’s study setup mimics clinical situations better as we don’t see the unsymptomatic patient and judging from their findings, a positive test can practically establish that Gluteal tendinopathy is present though excluding the condition with a negative test is not possible, which is why we give it a strong clinical value in including the condition.
You should clear the lower back or SI Joint as a possible source for somatic referred pain to the lateral hip region.
Essentially forming the diagnosis requires (Grimaldi et al. 2017):
1) Pain on palpation
Pain on palpation was the most specific test in the study with a sensitivity of 80% and a specificity of 46,7%. This was the most sensitive test in the study and due to its negative likelihood ratio of point four three we give it a rather weak clinical value in excluding gluteal tendinopathy
2) 1 positive active test of the following:(e.g. FADER-R, ADD-R, SLS)
The Single leg stance test was the most specific test in the study.
To conduct the test the patient lies supine. Then flex the hip to 90°, adduct the hip, and add external rotation to end of range. Now, ask the patient to perform isometric internal rotation against your resistance, which will increase both tensile and compressive forces on the tendon of the gluteus medius and minimus. A positive test is the reproduction of the patient’s lateral hip pain in the region of the greater trochanter of at least 2/10 on the NPRS.
To conduct the test the patient lies on the bench in a diagonal side-lying position on their unaffected side with the hip and knee flexed to 80-90 degrees.
Support the affected leg with the knee extended, in neutral position so that leg is in line with the trunk. The anterior superior iliac spines are perpendicular to the treatment table. Whilst stabilizing the pelvis, the leg is moved into end-range hip adduction with overpressure. Subsequently, the patient is asked to perform isometric hip abduction against resistance. This position adds both passive and active tensile and compressive loads on the tendons of the Gluteus medius and minimus. A positive test is the reproduction of the patient’s lateral hip pain in the region of the greater trochanter of at least 2/10 on the NPRS.
3) Imaging evidence correlating with clinical signs and symptoms
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Grimaldi et al. (2015) wrote a clinical commentary on the proposed management of the condition as high-quality studies are still lacking. These recommendations are based on pathobiology, general information on tendon pain management, and principles and concepts of optimization of hip abductor muscle function, hip movement, and lower limb alignment.
As with many if not all tendinopathies load management is one of the key principles of rehab. In the case of GTPS, we want to avoid compression and stretch. Here are some things to consider to avoid:
Aspects to consider in reducing compression
Avoid hip adduction („hanging on one hip“ while standing, standing with legs crossed, sitting with knees crossed or knees together, as well as sleeping in a side-lying position. As sleep is often disturbed in GTPS, here are some Tips: sleeping on the back with legs slightly abducted reduces compression on the tendons, and you can also use a pillow between legs when sleeping in side lying. If symptoms are bilateral, the other hip can be cushioned with an eggshell mattress
Aspects to consider in reducing tensile loads
Any activity that involves a rapid stretch-shortening cycle (contraction) should be reduced. For athletes, this may mean temporarily avoiding long distance, high tempo, hill running, and plyometrics. Water-based exercise can serve as a temporary alternative.
Isometric Exercises
Isometric exercises have been shown to be a good starting point in tendinopathy rehab though the optimal loading dose for the gluteals has yet to be determined. A good starting point for isometrics in GTPS is to perform isometric abduction in a side-lying position. Here the patient should use pillows in between the legs to keep the hip from adducting.
For bilateral issues the patient can lie supine with the hips slightly abducted and a theraloop can be used for light resistance. Even performing it in standing is an option. Patients are asked to ramp up the contraction slowly and minimize pain. They can hold the contraction for around 45 seconds and repeat it 4 times several times per day.
Low-velocity high load home exercises
As a next step, we will look at low-velocity high load exercises that are easily done at home. Here a fine balance has to be found as there is a chance of potentially overloading and thus aggravating the tendon. A good indicator to assess progress is the change in night pain that is common in GTPS.
While we can target the hip abductors in a side-lying position with exercises such as (banded) clamshells or abduction, weight-bearing exercises have higher recruitment of the gluteals than non-weight-bearing exercises.
Example exercises can be:
- Banded sliders: The patient stands behind a chair for support. With the theraloop around the ankles and the foot of the affected hip on a sliding mat or towel, the patient slowly slides the leg into abduction and returns to the starting position.
- Side stepping: Sometimes, depending on the condition of the patient, sidestepping with a focus on the pushing leg can be enough to start engaging the hip abductors
The exercises should be done at least 3 times a week at first with moderate intensity and low repetitions. Closely monitor the tendon reactivity in the 24 hours following the exercises to establish an appropriate load. See this chart for a rule of thumb. Also, as previously mentioned, a good indicator of success is a change in night pain.
Exercise Protocol for GTPS
In recent developments, Mellor et al. (2018) conducted a prospective single-blinded randomized clinical trial comparing education plus exercise versus corticosteroid use versus a wait-and-see approach. This trial design allows us to analyze whether exercises on top of education are better than the conditions natural course.
After eight weeks, the exercise group was significantly better than the two other groups in terms of pain and global perceived change with an 80% success rate. At the 12 months follow-up, the exercise group was again better in terms of global perceived change than the wait-and-see group and the corticosteroid injection group and can thus be regarded an effective way of managing gluteal tendinopathy.
The exercise group received education about the condition, advice about load management and the following exercises to gradually build up the capacity of the tendons:
The exercises were done in 14 individualized sessions with a physiotherapist over the course of eight weeks as well as daily at home. For all exercises, the Borg scale is used to monitor difficulty. Warm-ups were done at a light level of 11-12, functional retraining at a 13-15 so somewhat hard to hard level, and targeted strengthening moving towards a hard to very hard level of 14-17 on the Borg scale. No change in trochanteric pain was acceptable during functional retraining. A maximum of NPRS 5/10 was tolerated as long as this eased after the exercise and did not increase pain at night or the next morning.
Here are the exercises from the protocol in writing:
Warm-up/low-load activation Exercises
- Static abduction in supine
- Static abduction in standing
Functional retraining exercises:
- Bridging (Double leg)
- Offset bridging
- Single Foot Hover
- Single leg extension
- Squat (Double leg)
Single-leg-focused exercise
- Offset squat
- Single leg squat
- Step-ups
- Scooter (slide lunge on a mat)
Strengthening exercises
- Side-stepping
- Band side slides (doorway slides)
- Mini squat bilateral abduction
Would you like to learn more about GTPS? Then check out the following resources:
- Gluteal vs. Sham Exersies in Gluteal Tendinopathy (Research Review)
- The Role of Shockwave in the Management of Chronic Tendinopathy – Common FAQs (Blog Post)
- Podcast Episode 007 – Hip Pathologies with Glen Robbins and Benoy Mathew
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Running Rehab: From Pain to Performance

What customers have to say about this online course
- gustaf hübinette05/02/25A fantastic course A fantastic and comprehensive course that I feel has both broadened and deepened my knowledge of running-related injuries and their rehabilitation. The content maintains a clear and cohesive structure, firmly grounded in research. A big plus is that even after completing the course, you can revisit the material whenever you need to review certain areas.Simon20/01/25Good, but too much! It's of course a luxury problem. It delivers, absolutely. I know a lot more about running injuries now. But you need to review how much time it takes to finish this monster.
- Salih Kuzal30/12/24Running Rehab Salih Kuzal Een hele leuke uitgebreide cursus wat goed toepasbaar is in de dagelijkse praktijk. Heb er veel van geleerd!Sander Wierstra27/12/24Leerzame cursus Deze cursus heeft me inzicht gegeven om topatleten en sporters beter te begeleiden richting een duurzame herstel, ik raad deze cursus zeker aan!
- Jaime van der Lugt27/12/24Running Rehab 2.0 Well organised and clear set-up course to dive deeper into Running Rehab. Very extensive. Would definitely recommend it!Jasper Campfens24/12/24Top cursus Erg sterke cursus. Zeer uitgebreid wordt er ingegaan op alle meest voorkomende hardloopblessures. Van diagnose tot RTR.
- Carmen21/12/24Running Rehab Very good en clear course!Thorin21/12/24Sterke aanrader! Zeer uitgebreide cursus over een grote populatie binnen de bevolking. Elke kinesitherapeut zal hier veel uit bijleren, of hij nu zelf aan lopen doet of niet! Gestructureerde cursus bestaande uit Evidence-Based teksten en video's. Duidelijke toepassing van de theorie terug te vinden in de video's.
- Ivo Rigter03/12/24Running Rehab: From Pain to Performance Bedankt voor de zeer uitgebreide en informatieve cursusEllen Oosting27/11/24Veel geleerd! Veel geleerd over blessures, behandeling, training en terugkeer naar sport. Afwisselende inhoud. Veel praktische tools. Punten ook snel bijgeschreven na afronding.
- Olivier19/11/24Goede cursus! Ik kan deze cursus alle fysiotherapeuten aanraden!Joas de Bijl07/11/24Fijne cursus Goede cursus waar wetenschap en klinische ervaring in terug komt. Leuke video’s die wat mij betreft goed aansluiten op de praktijk!
- Koen24/10/24Leerzame Cursus Een cursus die een absolute bijdrage levert voor therapeuten die veel patiënten zien met hardloopblessures.
Vooral de praktische tips en de opbouw na een blessure zijn erg bruikbaar en toepasbaar in een eerste lijn praktijk.
Tevens zijn de evidence based artikelen een mooie toevoeging op de kennis die al wordt gegeven.Tim14/10/24Great course Learned a lot about running injuries. So much more structure in assessing and treating all lower limb injuries. - Maria Kramer14/10/24Running Rehab: From Pain to Performance Goede cursus voor therapeuten die veel hardloopblessures behandelen en hier meer over willen weten. Veel evidence based informatie en praktische tips voor de opbouw na een blessure.Emin Yildiz26/08/24Running Rehab: From Pain to Performance Leerzaam, uitleg en inhoud van top kwaliteit!
- Daniel Deyhle02/02/24Running Rehab: From Pain to Performance A VERY DETAILED COURSE
Really nice! Lot´s of high quality content! I learned so much. Thank you!Jarne Standaert18/04/23Running Rehab: From Pain to Performance Dit is een uitstekende cursus voor therapeuten die patiënten met loopblessures gerichter en efficiënter willen behandelen. Je krijgt enerzijds een uitgebreid overzicht van welke loopgerelateerde blessures zich vaak voordoen. Anderzijds krijg je een goed onderzoekskader om de tekorten bij je patiënten op te sporen en dus ook gerichter te behandelen. De cursus is heel duidelijk. Je krijgt ook een goed beeld van welke oefentherapie je best toepast in een bepaald stadium van een bepaalde pathologie - Hannah Yelin09/04/23Running Rehab: From Pain to Performance A great course that gives you a comprehensive and detailed knowledge of various running complaints. The content is evidence based and the literature is attached. It is very well taught how to transfer the evidence into everyday practice. I highly recommend this course to all physios who work with runners.
Thank you for a great course!Ruba Al Barghouthi23/10/22Running Rehab: From Pain to Performance Very informative course. Highly recommended for every MSK Physiotherapist and any other health care providers who deal with runners.







