The Impact of Pain Neuroscience Education on Structural Brain Changes in Chronic Spinal Pain

Introduction
Chronic pain is an increasing problem and has been linked to structural changes in the brain’s white matter. Pain neuroscience education is an effective option for treating chronic pain, but it is unclear whether this approach is also effective in addressing structural brain changes. This study focuses on the white matter after an earlier study found no changes in grey matter brain structures.
Methods
This study was a secondary analysis of a randomized controlled trial by Malfliet et al. (2018) who investigated the effectiveness of pain neuroscience education combined with cognition-targeted motor control training versus usual physiotherapy in people with nonspecific chronic spinal pain who were between 18 and 65 years. Chronic pain could include, for example, chronic low back pain, failed back surgery syndrome (> 3 years), chronic whiplash or chronic nontraumatic neck pain. Pain had to be present for at least 3 days per week for at least 3 months to be eligible. Participants were asked to continue their usual medication only and not to start any new interventions or therapies during study participation and six weeks before study enrollment.
Neuropathic pain, recent back surgery (< 3 years), osteoporotic vertebral fractures, rheumatological diseases, chronic widespread pain syndromes (like fibromyalgia and chronic fatigue syndrome) were excluded.
Interventions
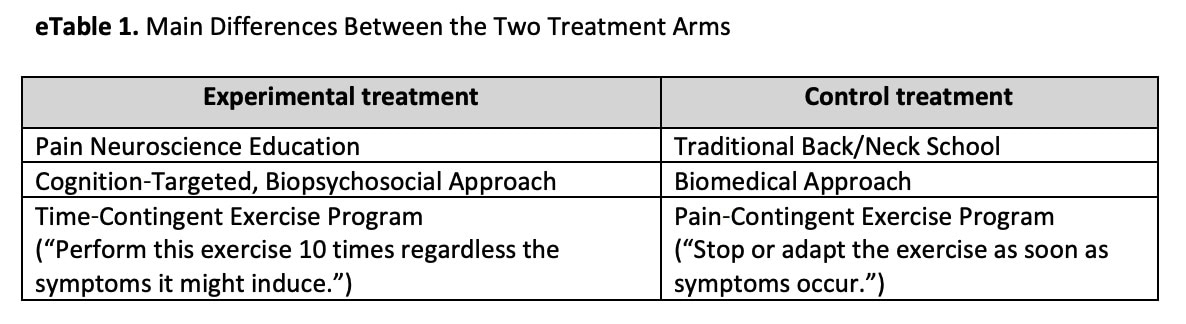
Two interventions were compared. The experimental intervention included a modern pain neuroscience approach as described by Nijs et al. (2014) that consists of 3 phases:
- Pain Neuroscience Education: three sessions covering pain mechanisms, central sensitization and neuroplasticity were held. Once adaptive beliefs about pain were acquired, phase 2 was initiated.
- Cognition-targeted neuromuscular training: in a time-contingent manner, sensorimotor control exercises were included to improve proprioception and muscle coordination. Thereafter, a graded exposure to feared movements took place. Graded Motor Imagery could be used if the level of fear was too high.
- Cognition-targeted dynamic and functional exercises were used to expose the participants to challenging and physically demanding tasks and feared movements.
The control intervention consisted of a biomedically-oriented treatment of traditional neck or back school with general physical exercise therapy. Rather than learning the neuroscience behind pain, the participants in the control group learned about mechanical causes of neck and back pain, the anatomy, physiology, and biomechanics (for example, ergonomics, joint forces, intradiscal pressure). They were also informed about the importance of strength, endurance, physical fitness, and strain associated with postural changes. Hereafter, the participants in the control group received exercises that focused on possible biomedical dysfunctions of the spine (like mobility, strength, etc), with progression to functional activities and physically demanding tasks. Participants were taught how to keep their spine in a neutral position during the exercises. Besides the more biomedical-oriented approach, another important difference with the experimental intervention was that in the control group a symptom-contingent approach was used. This means that when symptoms occurred during or after an exercise, the intensity or the frequency of the exercise was reduced.
Both interventions were held during 12 weeks and 18 sessions in total.
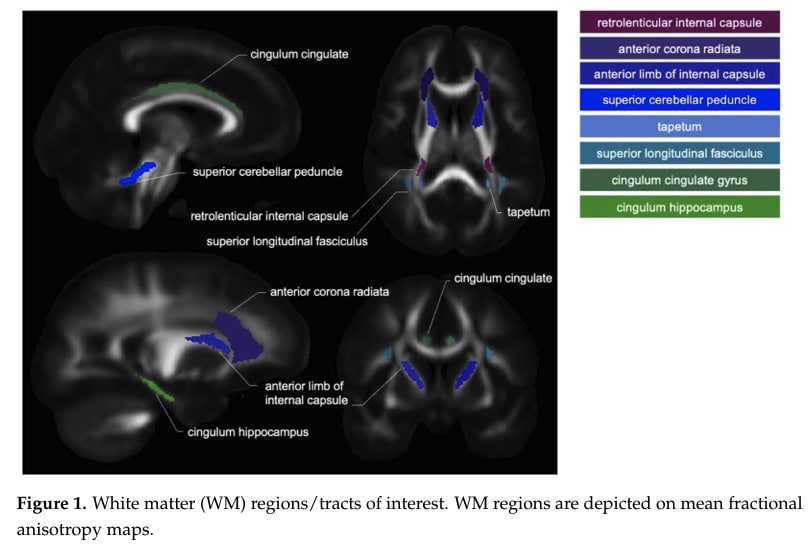
In this secondary analysis, the investigators delved into the impact of pain neuroscience education on the brain, specifically on structural components like white and grey matter. Therefore they compared the groups from the original RCT for structural brain parameters:
- anterior corona radiate,
- internal capsule,
- cingulum hippocampus,
- superior cerebellar peduncle,
- superior longitudinal fasciculus
Outcomes
Two weeks before the start of the study, all participants underwent baseline Magnetic Resonance Imaging (MRI). Pain pressure thresholds (PPTs) were assessed using a digital algometer on a different day. The mean of two measurements at the upper trapezius muscle (midway between C7 and the tip of the acromion), 5 centimeters lateral of the spinous process of L3, and at the quadriceps muscle were recorded. The most painful side was chosen for the PPT assessment in case of bilateral pain.
Several patient-related outcome measures were collected:
- The Numeric Rating Scale (NRS) was used to measure the spinal pain over the last 3 days on a 0-10 scale.
- The Central Sensitization Inventory (CSI) assessed somatic and emotional symptoms related to central sensitization
- The Pain Catastrophizing Scale (PCS) measured aspects of catastrophic cognitions about pain rumination.
- The 17-item Tampa Scale for Kinesiophobia (TSK) assessed fear of movement and re-injury.
- The Pain Disability Index (PDI) captured disability associated with pain in social roles (family/household responsibilities, recreation, social activities, occupation, sexual behavior, self-care, and life support activities)
- The Short-Form 36 Health Status Survey (SF-36) measured the functional status and state of well-being and health-related quality of life and results in two main subscales: physical health (SFPH) and mental health (SFMH)
These measurements were collected at baseline, post-intervention and after 1 year. The study aimed to identify structural brain changes (white matter) and chronic spinal pain and the potential response to therapy.
Results
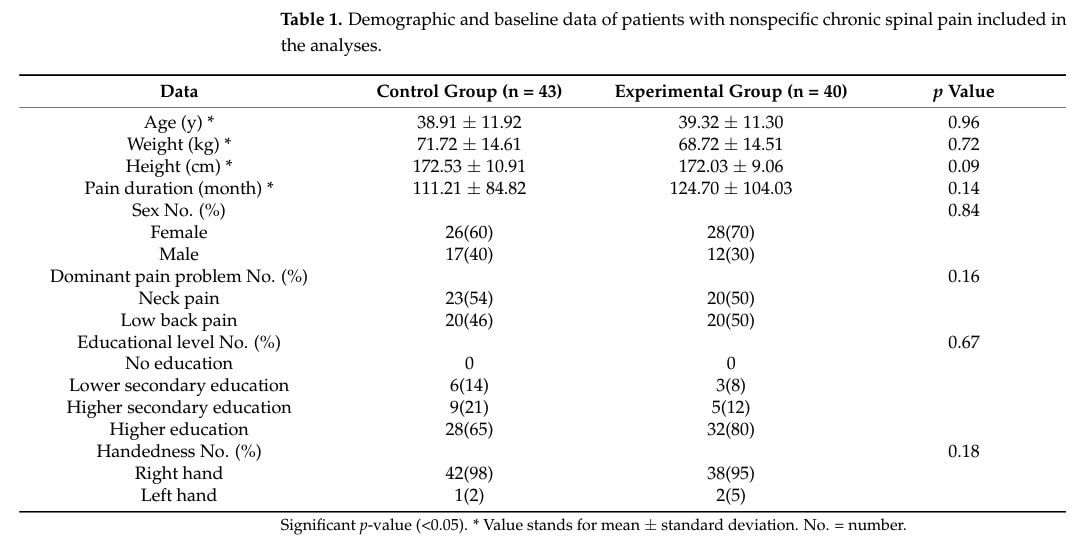
A sample of 120 participants was included in the original RCT and equally divided over the experimental intervention of pain neuroscience education or the biomedically-oriented control intervention. In this secondary analysis, 40 participants were analyzed in the experimental intervention and 43 in the control group, since poor data quality and drop-out occurred. Both groups were comparable at baseline.
For the primary outcome, changes in white matter brain structure, no significant main effect of treatment or interaction effects were observed. There were various significant effects of time, indicating that throughout the study both groups experienced changes in white matter brain structure, regardless of the treatment group they were in.
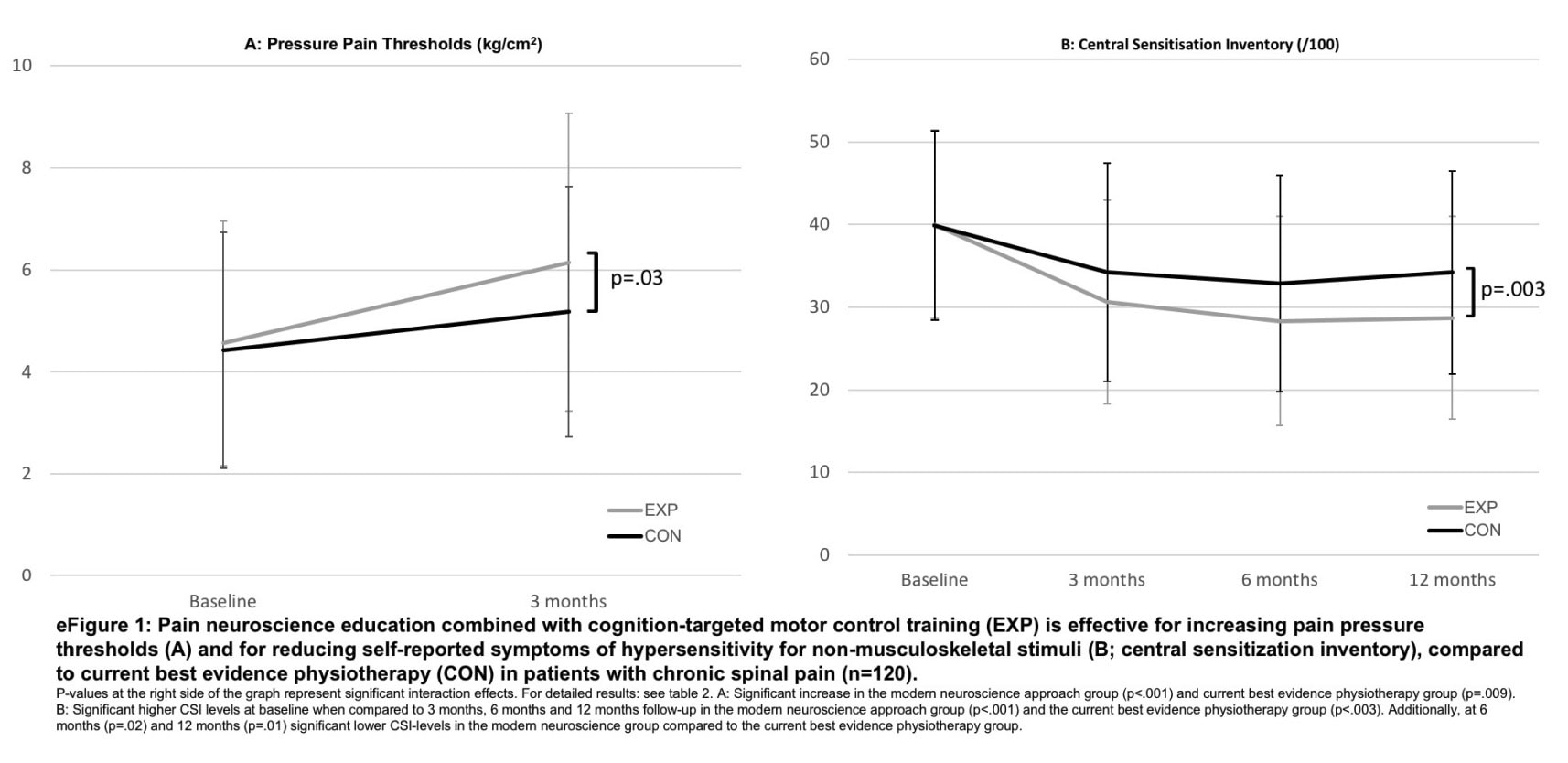
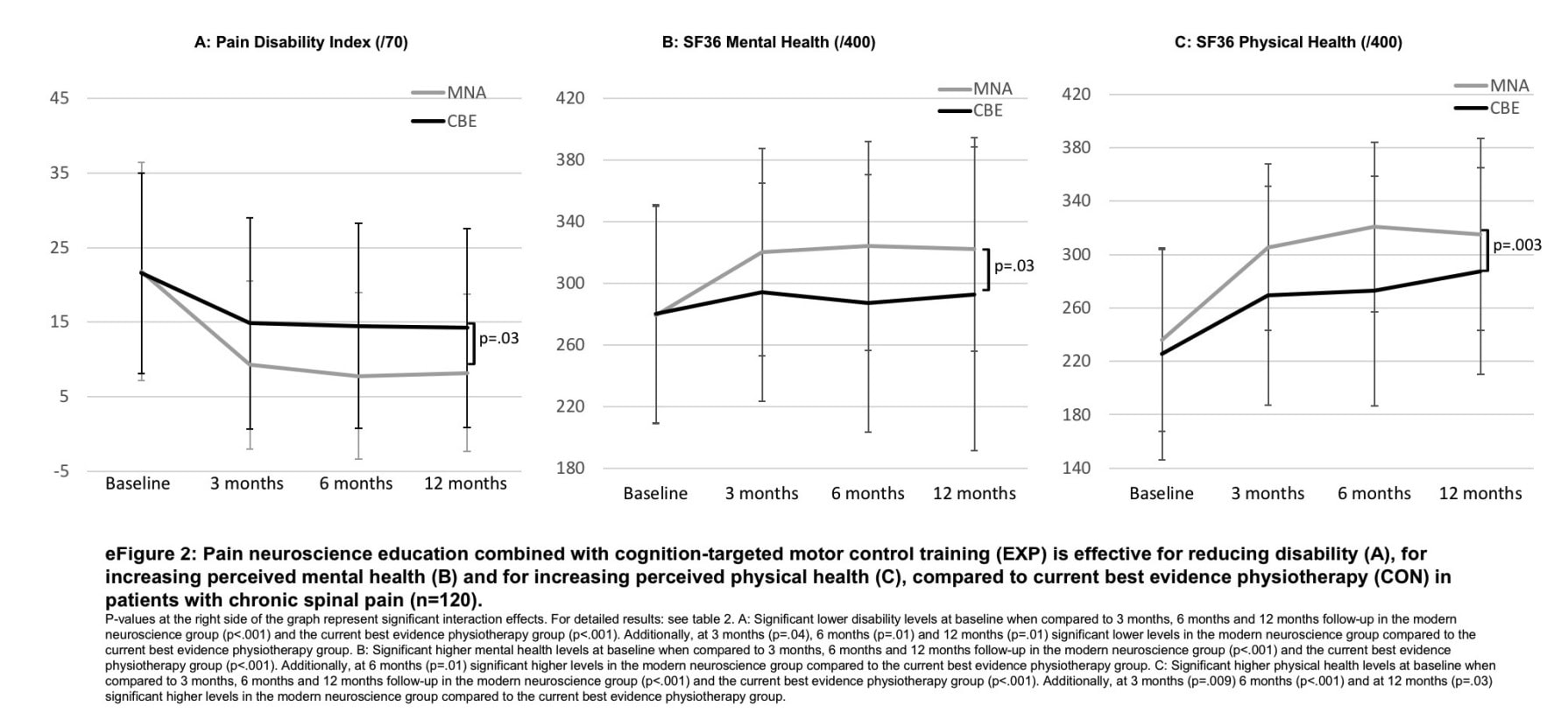
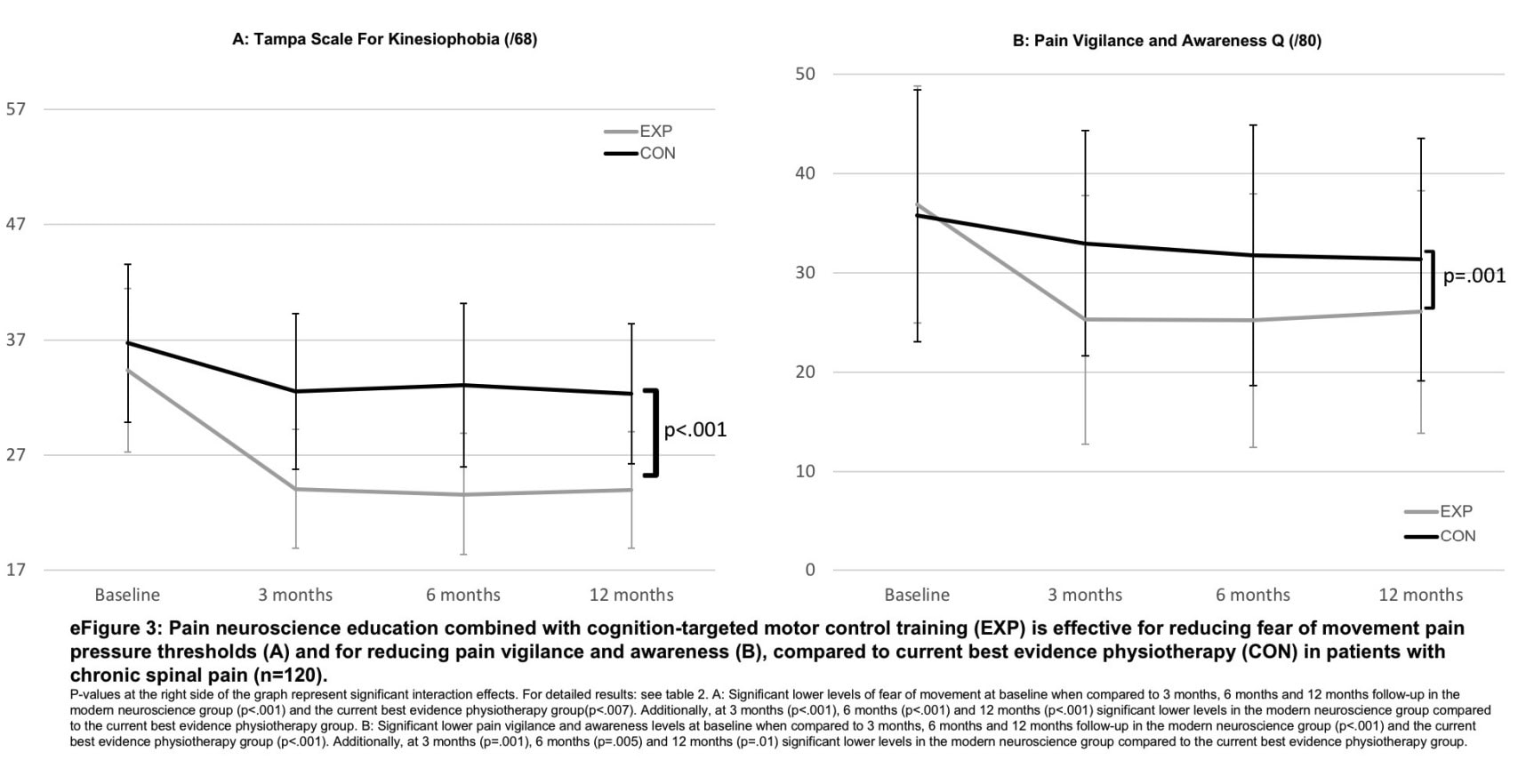
The original trial revealed significant clinical improvements in both groups, with a greater improvement in the group following the experimental pain neuroscience education. The current trial indicates that these improvements were not related to white matter changes in the brain.
Questions and thoughts
The original RCT from 2018 was able to show meaningful reductions in pain, symptoms related to central sensitization, disability, and kinesiophobia. Also, function was improved and people experienced improved pain pressure thresholds. However, the current study had no significant treatment effect regarding the changes in white matter brain structure. There might be several reasons that no effect in the brain was observed, despite the clinical improvements after pain neuroscience education in this population.
- It is possible that the intervention was able to cause clinical improvements but that the brain needs more time to adapt. Therefore, longer studies might answer whether the duration of the pain neuroscience education helps structural changes in the brain manifest.
- Another possibility is that the imaging was not sensitive enough to capture changes in the white matter. Changes might be very subtle and although modern imaging can capture a lot of information, subtle changes might have slipped through the cracks.
- Further, another possible explanation might be that other brain areas than those studied here are more involved in the improvement of pain and function. Or maybe, no structural brain changes occurred at all, but rather functional changes such as improved connectivity or neurotransmitter balance or synaptic plasticity are achieved.
- Baseline white matter integrity can also have influenced the findings. Since the population included people from various ages (18 to 65 years), local changes in blood flow or blood vessels can cause damage to the white matter and altered function. We know that white matter lesions can be subclinical (i.e. not causing symptoms) and the health of the white matter is intrinsically linked to cardiovascular health. So, as these people were analyzed together between 18 and 65 years, a lot of variability in cardiovascular health status (e.g. the presence of atherosclerosis) can have impacted white matter integrity and caused unbalanced groups. An upcoming study is designed to investigate early brain alterations associated with subclinical atherosclerosis in healthy middle-aged individuals (40-54 years), which made me wonder whether this could have impacted the current study’s results. The analyses were controlled for age, but subclinical changes might have had a spell on these results.
- Migraine was not excluded, while in these people, an increased risk of developing white matter lesions and an increased prevalence of white matter lesions was shown. Indirectly, a study showed that smoking can increase headache frequency in migraine, and therefore smoking can indirectly influence the white matter of one’s brain. No correction for smoking status or migraine was made and this could have impacted the results.
- The fact that white matter changes was a secondary outcome variable of the original 2018 RCT may have caused the study to be not powerful enough to capture differences
Talk nerdy to me
This was the first study that assessed structural brain changes in response to pain neuroscience education. The study included participants from multiple primary care centers. The authors have successfully included a Bonferroni correction approach to account for the multiple comparisons. This approach refrained the study from relying on apparently statistically significant findings which disappeared after correction.
A limitation of this study is that no pain-free control group was included. Equally important, no group was included that did not receive treatment. Pain pressure thresholds were not measured at the 1-year follow-up. Unfortunately, a significant amount of people (n=37) were lost to follow-up, due to technical difficulties in the imaging (poor imaging quality due to excessive head motion during MRI acquisition).
Caution is also required since this was a secondary analysis of a randomized controlled trial conducted in 2018 with the primary aim to study the effects of pain neuroscience education on clinical outcomes such as pain, disability and pain cognitions.
Take-home messages
Pain neuroscience education combined with a time-contingent exercise approach was able to improve clinical outcomes in people affected by chronic spinal pain, but no differences were observed in structural white matter changes over time.
Reference
How Nutrition Can Be a Crucial Factor for Central Sensitisation - Video Lecture
Watch this FREE video lecture on Nutrition & Central Sensitisation by Europe’s #1 chronic pain researcher Jo Nijs. Which food patients should avoid will probably surprise you!



