Achilles Tendinopathy Rehab – Everything you need to know!
De Vos et al (2021) published a new guideline on the multidisciplinary management of Achilles tendinopathies. If you want to know the paper's core components regarding physical therapy, keep on reading.

In this blog article, we discuss Achilles Tendinopathy Rehab and you will learn everything you need to know from diagnosis to treatment!
De Vos et al (2021) published a new guideline on the multidisciplinary management of Achilles tendinopathies. If you want to know the paper’s core components regarding physical therapy, keep on reading.
More of a listener/watcher than a reader? Make sure to watch this synopsis video on the topic.
Risk factors and primary prevention
Dutch multidisciplinary guideline on Achilles tendinopathy
There is currently insufficient knowledge about modifiable and non-modifiable risk factors for the onset of Achilles tendinopathy.
Consider informing individuals with a history of lower limb tendinopathy who would like to increase or their training load on the risk of Achilles tendinopathies.
- Gradual training build-up (type, frequency, intensity, size)
- Targeted calf muscle strengthening exercises pre-season
- Wear enough warm clothing during winter
- Avoid fluoroquinolone antibiotics if alternatives are available
Diagnosis
Mid-portion based on the following findings:
- Symptoms 2-7 cm proximal to the insertion
- Painful on loading
- Local thickening of the tendon mid-portion (may be absent with short symptom duration)
- Pain on palpation
Insertional based on the following findings:
- Symptoms within 2 cm proximal of the insertion
- Painful on loading
- Local thickening of the tendon mid-portion (may be absent with short symptom duration)
- Pain on palpation
Consider imaging if the symptoms do not fit with all four criteria, when there’s an unexpected course of symptoms, or when surgery is being considered.
Options include:
- MRI of the ankle
- Ultrasonography of the tendon
- X-Ray of the calcaneus
Make sure you remember this statement:
Treatment
Consider using the VISA-A questionnaire to evaluate your treatment progression or regression. Inform your patient that no or only limited improvements are expected in the short-term.
Treatment components:
- Education about the condition, prognosis
- Addressing psychological factors
- Loading advice: temporary cessation or replacement of pain provoking activities
- Gradually increase the activity
- Use a pain scale to monitor activities and adjust accordingly
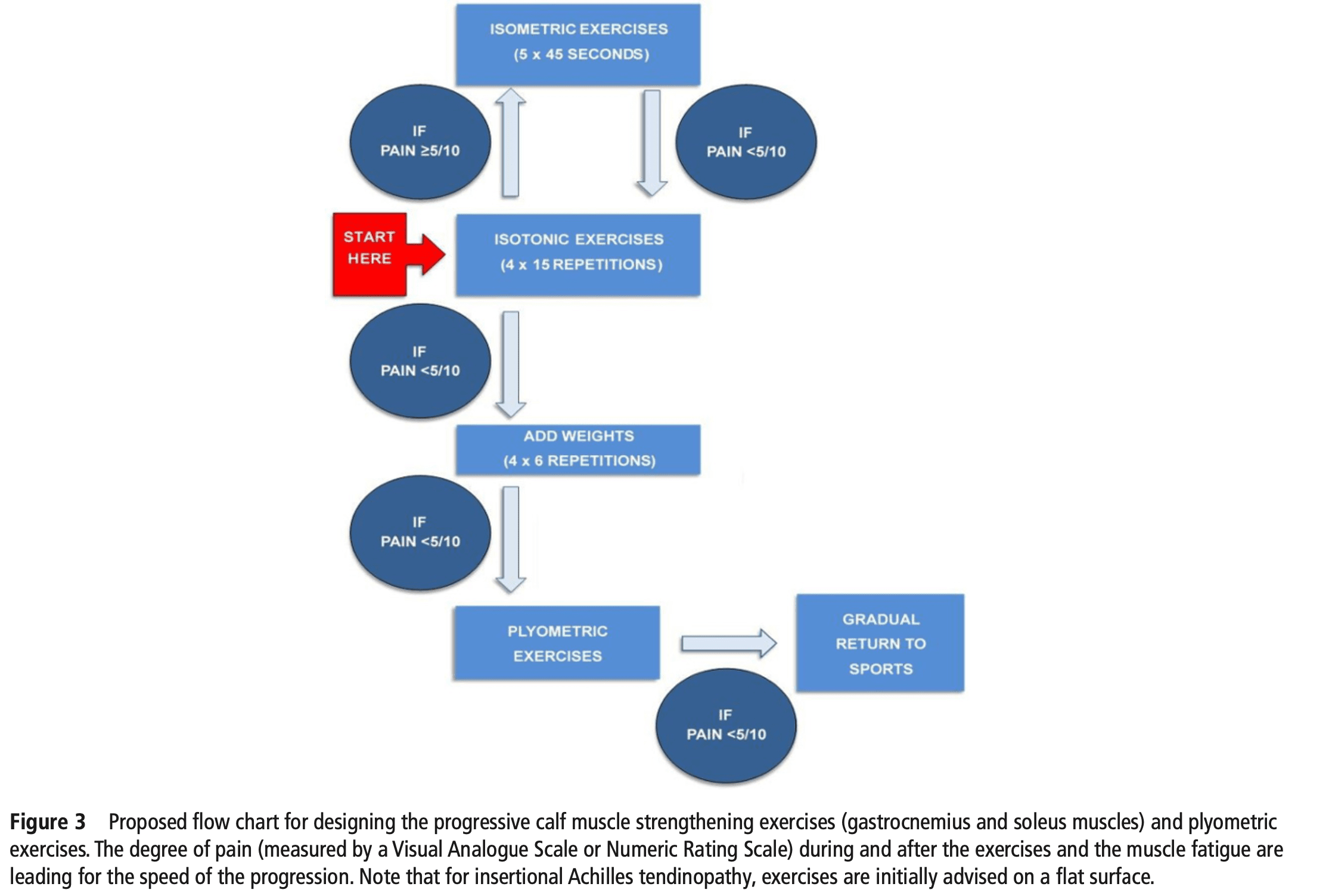
- At least 12 weeks of calf strengthening
- Form of exercise should be suited to the individual (flat surface for insertional complaints to start)
THE BIG 3 – ADVANCED REHABILITATION OF HAMSTRING, QUADRICEPS, AND CALF MUSCLE- AND TENDON INJURIES
Many therapists simply don’t know how to structure their rehab program which prevents their patients to unlock their potential, we’ve done all the hard work for you.
If these core components provide insufficient relief. One could consider the following options:
- ESWT
- Other passive modalities: night splint, inlays, collagen supplements, ultrasound, friction massages, laser therapy, light therapy, injection therapy, acupunture
Be cautious with NSAID’s and corticosteroid injections.
The authors propose the following flow chart for exercise progression:
Surgery of the Achilles tendon is only considered after at least 6 months of active treatment without recovery.
Prognosis
“The majority of patients recover, but there is a chance that symptoms may persist in the long term (at least up to 10 years with 23-37% having persistent symptoms), despite treatment.”
Eighty-five percent of athletes return to sport — return to performance is unknown.
Make sure the patient knows that you cannot provide a long-term prognosis, since these factors are unidentified.
Recurrence
Sufficient time (months) should be spent on active activities before full return to sport. A quick return to sport (days) is associated with a higher recurrence. Build up gradually, even after recovery when the patient had a period of relative inactivity. Consider continuing exercise therapy for the calf — even after recovery.
Reference
Open access article: https://pubmed.ncbi.nlm.nih.gov/34187784/

Max van der Velden
Research Manager
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







