Cauda Equina Syndrome | Diagnosis & Treatment

Cauda Equina Syndrome | Diagnosis & Treatment
Introduction & Pathomechanism
The cauda equina is the termination of the spinal cord. Typically the spinal cord ends at the level of L2, where it ends in cord-like nerves. It resembles a horse’s tail and therefore it is called the cauda equina. Cauda equina syndrome is typically a result of compression of the lower nerves S2, S3, S4, and S5. Compression of the higher nerve roots mainly affects the leg(s) and does not lead to the typical symptoms of for example saddle anesthesia. Cauda equina syndrome is a serious pathology requiring prompt action.
Pathomechanism
The most common cause is a massive lumbar disc herniation or prolapse which compresses the roots of the cauda equina. Other possible causes can be a mass caused by an infection or a hematoma or a bony fragment from a vertebral insufficiency fracture. In the prospective multi-center observational cohort study by Woodfield et al. in The Lancet (2022), the most affected levels were L4-L5 and L5-S1.
Epidemiology
Woodfield et al. in 2022 found that females between 30 and 39 years had the highest incidence of CES at 7.2 (95% CI: 4.7–10.6) per 100.000 females in the population per year. In the Scottish population referred for emergency surgical decompression, the crude incidence was 2.7 patients per 100.000 adults per year. According to Greenhalgh et al. (2018), cauda equina syndrome most frequently occurs between the ages of 31-50 years.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture
Signs and Symptoms
One or more of the following symptoms have to be present.
- Bladder and/or bowel dysfunction
- Reduced sensation in the saddle area
- Sexual dysfunction, with possible neurological deficit in the lower limb (motor/sensory loss, reflex change).
These symptoms can be associated with low back pain, as the most common cause of cauda equina syndrome is a lumbar disc herniation.
Three types of cauda equina syndrome onset can be observed, based on the patient’s presentation:
- Rapid onset of cauda equina symptoms with an absent history of back problems
- Acute onset of bladder dysfunction and or cauda equina symptoms together with a history of back problems and sciatica
- Gradually progressing onset of cauda equina symptoms with longstanding back problems. Often spinal stenosis is present.
The first cauda equina syndrome presentation type is rare. Type 2 is the most common form of cauda equina syndrome. The last type, with slow progression, occurs more frequently in older people and is usually not urgent. However, careful monitoring of symptoms is required, especially as people in this age group can be unaware of the importance of changing bladder and bowel function. They may often attribute it to their increasing age. Also, they may be less sexually active, which may mask symptoms of sexual dysfunction.
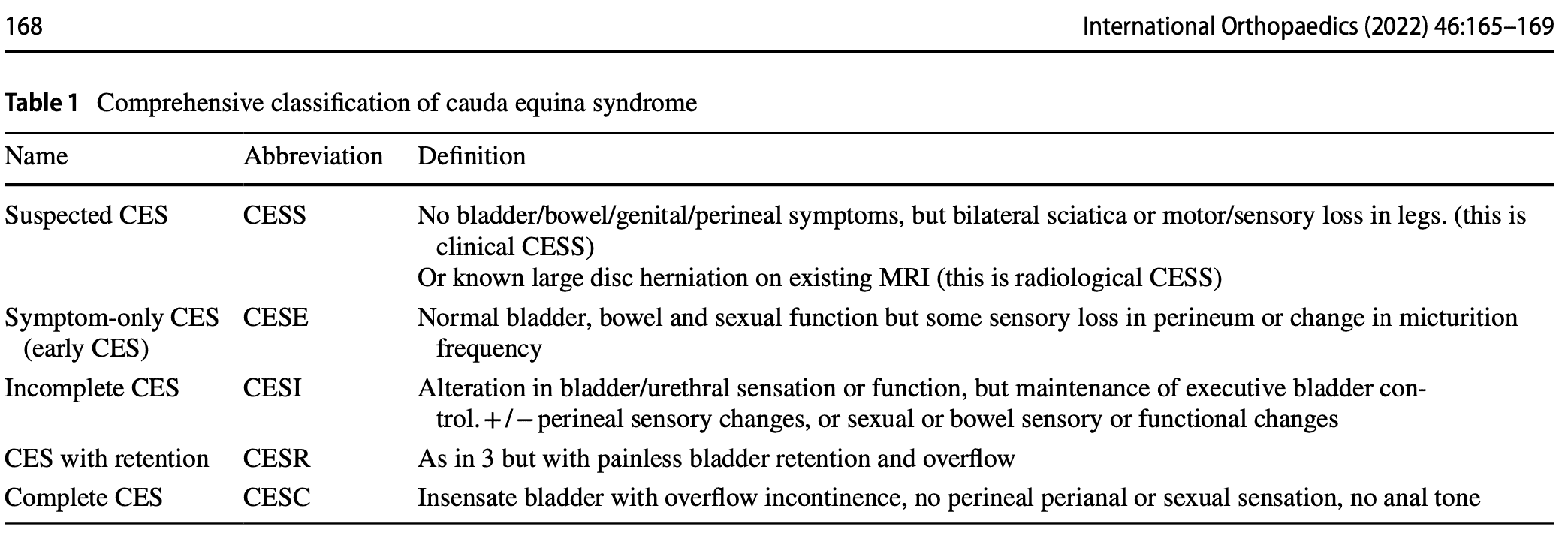
The classification above is based on the presentation of the symptoms. However useful and easy to remember, the following classification is the most commonly used.
CESI/CESR classification
This classification system defines 5 stages of cauda equina syndrome.
- Suspected cauda equina syndrome (CESS) is when there is bilateral sciatica or a loss of motor or sensory function in the legs. In the case of these symptoms, this is referred to as clinical CESS. Radiological CESS on the other hand is when a large disc herniation is present on MRI, which compresses the cauda equina. This stage can be accompanied by variable neurological symptoms and signs and a suggestion of sphincter disturbance.
- Early cauda equina syndrome (CESE) is defined as symptom-only cauda equina syndrome. There is a normal bladder, bowel, and sexual function. There may be a change in the micturition pattern, but the perineal sensation is normal. Or there may be a change in the perineal sensation with normal bladder function.
- CESI is defined as incomplete cauda equina syndrome. The patient has problems with urinating and these arise due to a neurogenic origin. These symptoms may include altered sensation with urinating, loss of desire to void, poor urinary flow, the need to strain, and an altered perineal sensation. But these symptoms do not lead to a loss of bladder function. These people have still executive control over the bladder and they may still void, even if it is more difficult.
- Cauda equina syndrome with retention (CESR) on the other hand refers to cauda equina syndrome with painless bladder retention. These patients are no longer in control of their bladder. Urine is retained and overflow is present, although painless. When patients get to this stage, it is impossible to reverse things around.
- Complete cauda equina syndrome (CESC) refers to a total loss of sensory and motor function
Examination
It is inappropriate to simply ask if the patient is incontinent. Incontinence is a late stage of CES, and in most cases before incontinence is reached there are subtle changes of urinary sensation, flow and frequency that must be enquired about. Similarly, both subjective and objective features of perineal, perianal and genital sensation need to be assessed. – From Lavy et al., International Orthopaedics (2022)
Subjective examination
The subjective examination is very important, especially early in the presentation of cauda equina syndrome. Five characteristic features of cauda equina syndrome have been recognized. There is however no chronology in the presentation of symptoms.
- Bilateral neurogenic sciatica, perception of bilateral weaknessReduced perineal sensation: sensory disturbance in the “saddle region”
- Urinary dysfunction and bowel dysfunction
- Bladder dysfunction is the most commonly reported symptom and can range from increased urinary frequency, difficulty in micturition, change in urine stream, urinary incontinence, and urinary retention.
- Loss or reduced anal tone may be evident if a patient reports bowel dysfunction.
- Bowel dysfunction may include fecal incontinence, inability to control bowel motions, and/or inability to feel when the bowel is full with consequent overflow.
- Loss of sexual function
- Saddle numbness
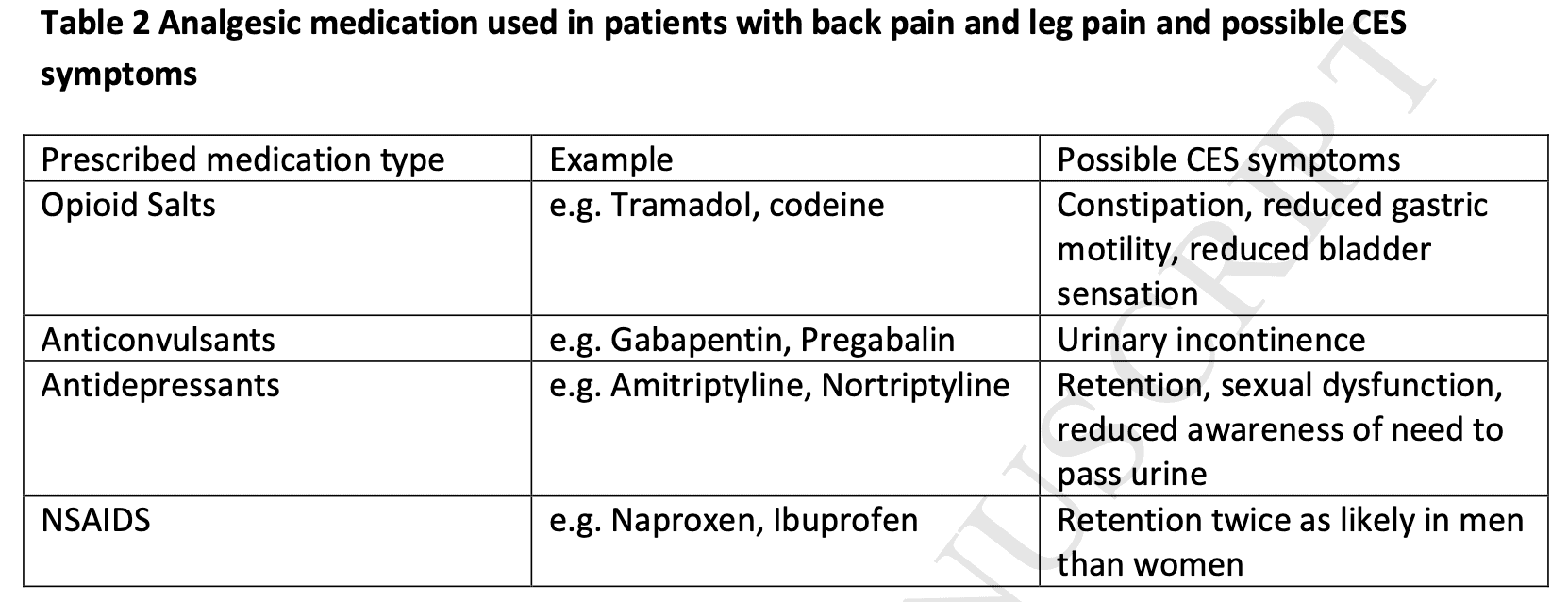
Importantly, regularly prescribed analgesic drugs for (back) pain like opioids can cause symptoms that masquerade as CES.
Clinical examination
The systematic review of Hoeritzauer et al. (2018) found 7 diagnostic accuracy studies for cauda equina syndrome but none was accurate in identifying the presence of the pathology.
A full neurological examination includes dermatome testing, myotome testing to find muscle weakness, and reflex testing. Sensory testing can be performed by evaluating the sensation to light touch and pinpricks in the saddle area including the buttocks, inner thighs, and perianal region.
If you suspect that the lesion is higher up (central nervous system), upper motor neuron tests such as the Babinski reflex, clonus testing, muscle tone testing, joint position sense, and gait testing should be performed.
Angus et al. (2021) retrospectively found that people with cauda equina syndrome more frequently had a loss of Achilles tendon reflex both unilaterally and bilaterally.
Cauda equina syndrome is a clinical diagnosis but should be supported by imaging (MRI) as there can be different causes for the symptoms to arise.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Timely and appropriate referral
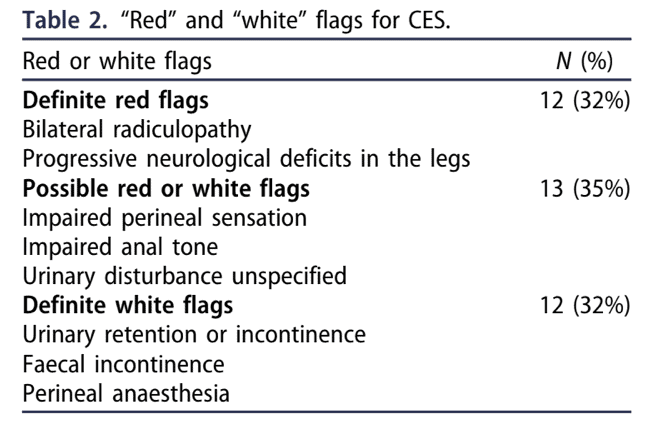
Individuals with cauda equina syndrome (CES) are typically referred late at a point when neurological damage cannot be restored. The symptoms and/or signs listed in guidelines for emergency referral, imaging, and treatment of CES are those of late-onset, irreversible CES. It might be too late to refer the patient at this point. Todd in 2017 proposed a set of true red flags and white flags. White flags refer to flags of “defeat and surrender”, meaning that if you find those signs and symptoms, the damage can be already irreversible, and thus, referral for that patient may already be too late. Therefore it is essential to screen for definite red flags as they warn for further avoidable damage ahead.
Emergency referral
When a patient complains of back pain, leg pain, or both, of recent onset (within two weeks) of any of the following symptoms, an emergency referral to the closest facility with Emergency MRI service is needed.
- Difficulty initiating micturition or impaired sensation of urinary flow;
- Altered perianal, perineal, or genital sensation S2-S5 dermatomes – the area may be small or as big as a horse’s saddle (subjectively reported or objectively tested);
- Severe or progressive neurological deficit of both legs, such as major motor weakness with knee extension, ankle eversion or foot dorsiflexion;
- Loss of sensation of rectal fullness;
- Sexual dysfunction – inability to achieve an erection or to ejaculate, or loss of vaginal sensation.
Urgent referral = referral within 2 weeks
In case your patient presents with sudden onset bilateral leg pain or unilateral leg pain that progressed to bilateral leg pain without CES signs or symptoms, you should make an urgent referral, meaning the patient needs to be seen within 2 weeks.
Safety netting
In early stages of cauda equina syndrome, symptoms can be vague. In order to make sure patients know how and when to seek care at the right moment, safety nets for patients experiencing back pain along with other symptoms are essential. When you make an urgent referral, it is also important to educate the patient in recognizing possible warning signs. In case signs and symptoms progress, you should make an emergency referral. The patient card below may be valuable to safety net your patient. This card can be found in 30 different languages at the following link.
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Learn More About the Most Common Spinal Pathologies

What customers have to say about this online course
- Ybe Boesveld17/06/25Erg informatieve cursus Vorig jaar opleiding manueel afgerond en deze cursus sluit goed aan op het niveau hiervan. veel artikelen weer op kunnen halen. Zeker aan te bevelen!Martijn17/06/25Duidelijke cursus Mooie, leuke en duidelijke cursus. Enige nadeel vond ik soms de vertaling van engels naar nederlands. Voor de rest was dit een hele fijne cursus om online te doen!
- Luis Humberto dos Santos Soares16/04/25Orthopedic Physiotherapy of the Spine "Clear and practical explanations — my knowledge has been seriously upgraded! Helped me pass my course with confidence."Michel Veerman16/04/25Top Super cursus. Alles mooi op een rijtje gezet over de wervelkolom.
- Orkun Buyukyilmaz06/04/25Take every course on physiotutors! This knowledge will make you a more relaxed physio. Because you know more!Ruud31/03/25orthopedische fysiotherapie van de wervelkolom top cursus, goed om alles weer even op te frissen.
- Robin28/03/25Top Cursus Perfecte cursus om je kennis op te frissen. Informatie is Straight to the point, aangevuld met handige video's.Emre Keskin02/01/25Very good cursus! Thanks to this course, I am more confident to examine and treat patients with spine-related complaints. It was a good refresher for me.
- Bas31/12/24Leerzame cursus Een hele fijne en leerzame cursus waarbij mijn kennis is uitgebreid door de behandelde stof. Zeer tevreden en aan te raden aan andere collega's
 Alex Pluijmert30/12/24The Spine Ideal course to get your facts strait on the latest evidence.
Alex Pluijmert30/12/24The Spine Ideal course to get your facts strait on the latest evidence.  Tom Wellens29/12/24Orthopedic physiotherapy of the spine Zeer uitgebreide en duidelijke cursus.
Tom Wellens29/12/24Orthopedic physiotherapy of the spine Zeer uitgebreide en duidelijke cursus.
Goed om het geheugen nogmaals op te frissen. Aanrader voor iedereen die werkt met patiënten met wervelkolom gerelateerde klachten!Jaime van der Lugt27/12/24Orthopedics Physiotherapy of the Spine Well organised and clear set-up course to refresh and to learn new things around the spine. Would definitely recommend it!- Erik Plandsoen26/12/24Cursus: 'The spine' Fijne opfrissingscursus en met momenten zeker ook vernieuwend. Voor mij als fysiotherapeut soms het gevoel dat de mobilisatietechnieken vooral Manueel therapie gericht waren, maar daarom niet minder leerzaam!Rud Raymakers24/12/24Course the Spine Fijne cursus! Overzichtelijk en leerzaam en goed recap na MT opleiding!
- Salih Kuzal23/12/24Cursus The Spine De cursus was zeer behulpzaam voor mijn vaardigheden en handelingen om mijn patienten effectiever te behandelen.
Ik vond het ook heel leuk en leerzaam om het uit te voeren.Steffie van der Niet22/12/24Orthopedic Physiotherapy of the spine Ook voor ervaren therapeuten een leerzame Online course, waarbij soms wat heilige huisjes van fysiotherapie uit de "oude" tijd omver geschopt worden. - Stefan Verbruggen17/12/24Cursus Goed opgezette cursus met een quiz aan het eind van elke onderdeel.
Heel overzichtelijk en leerzaam.Jordy17/12/24Valuable and well-organized I am very satisfied with this course. The setup was clear and well-structured, making the material easy to follow. The videos were helpful and of good quality, with clear explanations that really helped in understanding the content better. The combination of theory and practical examples ensured that the information is directly applicable. All in all, it is a valuable and well-organized course that I would definitely recommend to others! - Todd A. Baker15/12/24Thorough and comprehensive course Well executed and organized course.Roland Zwiggelaar08/12/24Nice learning course I found this course very good because it updates my total knowledge of the spine.Also it shows you the info with the latest articles there are for now.