Achilles Tendon Rupture | Diagnosis & Treatment
Achilles Tendon Rupture | Diagnosis & Treatment
Introduction & Pathophysiology
The Achilles tendon is the biggest and strongest tendon in the human body. It is formed by the tendons of the soleus and gastrocnemius muscles and 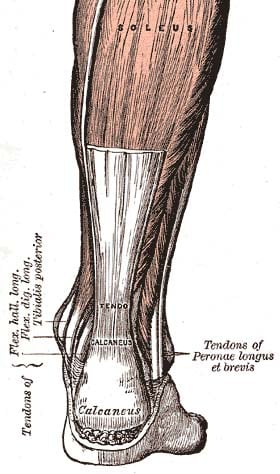
A rupture of the Achilles tendon usually occurs during athletic activities when heavy loads are placed on the tendon as occurs during acceleration or jumping (push-off). So the mechanism of injury can be (Arner et al. 1959):
- Weight-bearing push-off with extended knee
- Sudden, unanticipated dorsiflexion of the ankle
- Forceful dorsiflexion of the plantarflexed foot
When the tendon ruptures, this usually occurs between 3-6 cm proximal to the calcaneal insertion (Moon et al. 2017).
Epidemiology
Achilles tendon ruptures are mostly seen in high-impact sports and occur more often in the male population. A study in Denmark reports an increase from 25.95/100.000 persons in 1994 to 31.13/100.000 in 2013 (Ganestam et al. 2016).
The literature lists a couple of risk factors that may predispose an individual to ruptures of the Achilles tendon (Jarvinen et al. 2005, McQuillan et al. 2005, Seeger et al. 2006, Kraemer et al. 2012)
These are:
- Tendon degeneration
- Poor tendon vascularity
- Corticosteroid use
- Fluoroquinolone use
- Previous contralateral rupture
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
If the tendon ruptures, patients report a distinct “pop”, “snap” or “crack” sound and immediate pain. The latter resolves rather quickly (Leppilahti et al. 1998). The patient may show gait abnormalities due to limited plantar flexion caused by the compromised tendon. This can be masked by overactivity of the posterior tibial, peroneal, and plantar muscles (Kauwe 2017).
Interestingly, 66% of all Achilles tendon ruptures are asymptomatic or patients have no pain, stiffness, or dysfunction in the tendon prior to rupture. Despite this, it is the case that 98% of all ruptured Achilles tendons show signs of degeneration. In 2014, Reiman et al published a systematic review including a meta-analysis on the diagnostic accuracy of various clinical assessments for diagnosing Achilles tendon ruptures. Probably the most widely used test is the Thompson test. With a sensitivity of 96% and specificity of 93%, it has a high clinical value in the diagnosis as well as in the exclusion of Achilles tendon ruptures.
To perform the test, the patient lies on the bench with the lower legs extended in the prone position. The patient’s ankles extend beyond the edge of the bench. Now compress the calf with one hand and pay attention to the movement of the foot. If compression of the calf results in plantar flexion of the foot, it can be assumed that the tendon is intact. However, if there is a lack of some degree of preload on the plantar flexion in the prone position and no further plantar flexion occurs due to compression of the calf, a rupture is likely.
Other commonly used orthopedic tests are:
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
A recent systematic review comparing the rate of re-rupture, functional outcomes, complication rate, return to sports and work, as well as differences between early and delayed weight-bearing concluded that the differences in these factors were non-significant across multiple RCTs and observational studies (Ochen et al. 2019). However, the decision remains with the patient and treating physician as no decision algorithms are available to date.
In the videos below you will find a couple of exercises a patient can do after Achilles tendon rupture repair from the acute phase onto later rehab phases.
Interestingly enough, these same principles are applied in patients who are receiving conservative management (Ollson et al. 2013, Lantto et al 2016).
The Achilles tendon is the biggest and strongest tendon in the human body and is formed by the tendons of the soleus and gastrocnemius muscles which both insert at the calcaneus. We mostly see ruptures of the Achilles tendon in high-impact sports predominantly in the male athlete.
While a scientific review from the year 2017 showed no significant differences in the outcomes of surgical and conservative management the re-rupture rate of conservatively managed tendons was higher and conservative management might not be suitable for every injury depending on its severity. However, there is a clear benefit of an accelerated rehab program including early mobilization versus immobilization as has been researched by Brumann et al. (2014).
In the 1st phase post-surgery, usually lasting about two weeks, the goal should be to properly educate the patient on the expected course. Make sure that the wound heals properly and swelling is under control The patient will likely wear a walker boot with 30° of plantar flexion, but should be able to walk with full weight-bearing. Your aim is going to be to strengthen the surrounding muscles.
So let’s look at what this could look like:
Having no pain at rest and no increase in swelling the patient may progress to more ankle mobility. In the second phase which can last up to three weeks, your goal should be to obtain a neutral ankle position and full plantarflexion range of motion. Make sure that the wound is healing properly and swelling continues to decrease, as well as work on restoring a normal gait pattern. You can continue to load the exercises from phase 1. But in phase 2 we are going to focus more closely on the ankle.
The 3rd stage – Late Achilles Tendon Rupture Repair Rehab – which can last up to 9 weeks will aim to restore the full function of the angle in terms of the range of motion. Proprioception, balance, and coordination as well as further increased strength to prepare the individual for possible sports-specific rehab.
So let’s take a look at what kind of exercises one could do here:
Would you like to learn more about Achilles Tendon Ruptures? Check out the following resources:
- Rehabilitation Regimen for Non-Surgical Treatment of Achilles Tendon Rupture (Research Review)
- Podcast Episode 040 – Achilles Tendon Rupture Rehab with Liz Marlow
- The Role of Shockwave Therapy in the Management of Chronic Tendinopathy – Common Q&As
References
ARNER, ORED, A. Lindholm, and S. R. Orell. “Histologic changes in subcutaneous rupture of the Achilles tendon; a study of 74 cases.” Acta Chirurgica Scandinavica 116.5-6 (1959): 484-490.
Ganestam, Ann, et al. “Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients.” Knee Surgery, Sports Traumatology, Arthroscopy 24.12 (2016): 3730-3737.
Moon Y, Choi KY, Ahn JH. “Acute Achilles tendon rupture”. Arthrosc Orthop Sports Med (2017): 59-65
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Running Expert Reveals His 5 Step Formula to Become a Running Rehab Specialist!

What customers have to say about this course
- gustaf hübinette05/02/25A fantastic course A fantastic and comprehensive course that I feel has both broadened and deepened my knowledge of running-related injuries and their rehabilitation. The content maintains a clear and cohesive structure, firmly grounded in research. A big plus is that even after completing the course, you can revisit the material whenever you need to review certain areas.Simon20/01/25Good, but too much! It's of course a luxury problem. It delivers, absolutely. I know a lot more about running injuries now. But you need to review how much time it takes to finish this monster.
- Salih Kuzal30/12/24Running Rehab Salih Kuzal Een hele leuke uitgebreide cursus wat goed toepasbaar is in de dagelijkse praktijk. Heb er veel van geleerd!Sander Wierstra27/12/24Leerzame cursus Deze cursus heeft me inzicht gegeven om topatleten en sporters beter te begeleiden richting een duurzame herstel, ik raad deze cursus zeker aan!
- Jaime van der Lugt27/12/24Running Rehab 2.0 Well organised and clear set-up course to dive deeper into Running Rehab. Very extensive. Would definitely recommend it!Jasper Campfens24/12/24Top cursus Erg sterke cursus. Zeer uitgebreid wordt er ingegaan op alle meest voorkomende hardloopblessures. Van diagnose tot RTR.
- Carmen21/12/24Running Rehab Very good en clear course!Thorin21/12/24Sterke aanrader! Zeer uitgebreide cursus over een grote populatie binnen de bevolking. Elke kinesitherapeut zal hier veel uit bijleren, of hij nu zelf aan lopen doet of niet! Gestructureerde cursus bestaande uit Evidence-Based teksten en video's. Duidelijke toepassing van de theorie terug te vinden in de video's.
- Ivo Rigter03/12/24Running Rehab: From Pain to Performance Bedankt voor de zeer uitgebreide en informatieve cursusEllen Oosting27/11/24Veel geleerd! Veel geleerd over blessures, behandeling, training en terugkeer naar sport. Afwisselende inhoud. Veel praktische tools. Punten ook snel bijgeschreven na afronding.
- Olivier19/11/24Goede cursus! Ik kan deze cursus alle fysiotherapeuten aanraden!Joas de Bijl07/11/24Fijne cursus Goede cursus waar wetenschap en klinische ervaring in terug komt. Leuke video’s die wat mij betreft goed aansluiten op de praktijk!
- Koen24/10/24Leerzame Cursus Een cursus die een absolute bijdrage levert voor therapeuten die veel patiënten zien met hardloopblessures.
Vooral de praktische tips en de opbouw na een blessure zijn erg bruikbaar en toepasbaar in een eerste lijn praktijk.
Tevens zijn de evidence based artikelen een mooie toevoeging op de kennis die al wordt gegeven.Tim14/10/24Great course Learned a lot about running injuries. So much more structure in assessing and treating all lower limb injuries. - Maria Kramer14/10/24Running Rehab: From Pain to Performance Goede cursus voor therapeuten die veel hardloopblessures behandelen en hier meer over willen weten. Veel evidence based informatie en praktische tips voor de opbouw na een blessure.Emin Yildiz26/08/24Running Rehab: From Pain to Performance Leerzaam, uitleg en inhoud van top kwaliteit!
- Daniel Deyhle02/02/24Running Rehab: From Pain to Performance A VERY DETAILED COURSE
Really nice! Lot´s of high quality content! I learned so much. Thank you!Jarne Standaert18/04/23Running Rehab: From Pain to Performance Dit is een uitstekende cursus voor therapeuten die patiënten met loopblessures gerichter en efficiënter willen behandelen. Je krijgt enerzijds een uitgebreid overzicht van welke loopgerelateerde blessures zich vaak voordoen. Anderzijds krijg je een goed onderzoekskader om de tekorten bij je patiënten op te sporen en dus ook gerichter te behandelen. De cursus is heel duidelijk. Je krijgt ook een goed beeld van welke oefentherapie je best toepast in een bepaald stadium van een bepaalde pathologie - Hannah Yelin09/04/23Running Rehab: From Pain to Performance A great course that gives you a comprehensive and detailed knowledge of various running complaints. The content is evidence based and the literature is attached. It is very well taught how to transfer the evidence into everyday practice. I highly recommend this course to all physios who work with runners.
Thank you for a great course!Ruba Al Barghouthi23/10/22Running Rehab: From Pain to Performance Very informative course. Highly recommended for every MSK Physiotherapist and any other health care providers who deal with runners.







