Heavy Slow Resistance Training in Lateral Epicondylalgia - How To Conduct Research
Introduction
Despite the consensus on exercise for lateral epicondylalgia, there’s a lack of detailed descriptions of optimal exercise components, making it difficult to recommend the “best” exercise protocol. Heavy slow resistance training has emerged as a treatment option for tendinopathies. While there is an abundance of trials examining the effectiveness of HSR training in the lower limb, evidence in the upper limb is scarce. Two recent studies developed a protocol for examining the effectiveness of heavy slow resistance training in lateral epicondylalgia. Last week, we delved into the first, a pilot study by Divya Mary et al. (2025), which had several methodological issues and flaws that invalidated the study’s conclusions. In part 2, which we’ll cover today, we present a feasibility study by Sveinall et al. (2024), which serves as a go-to example of how to conduct research. Sveinall’s study was eager to look into the feasibility of conducting a RCT comparing heavy slow resistance training in lateral epicondylalgia to shockwave therapy, or information and advice only.
Methods
This study was a feasibility trial, meaning it aimed to see if different interventions for lateral epicondylalgia (tennis elbow) were practical to deliver and receive, rather than definitively proving which one is most effective. This is an essential first step before a true superiority RCT should be conducted.
Adult participants were included in case a clinical diagnosis of lateral epicondylalgia was confirmed by 2 out of 5 positive provocation tests:
- Pain on palpation
- Cozen’s Test
- Pain during power grip
- Maudsley’s Test
- Mill’s Test
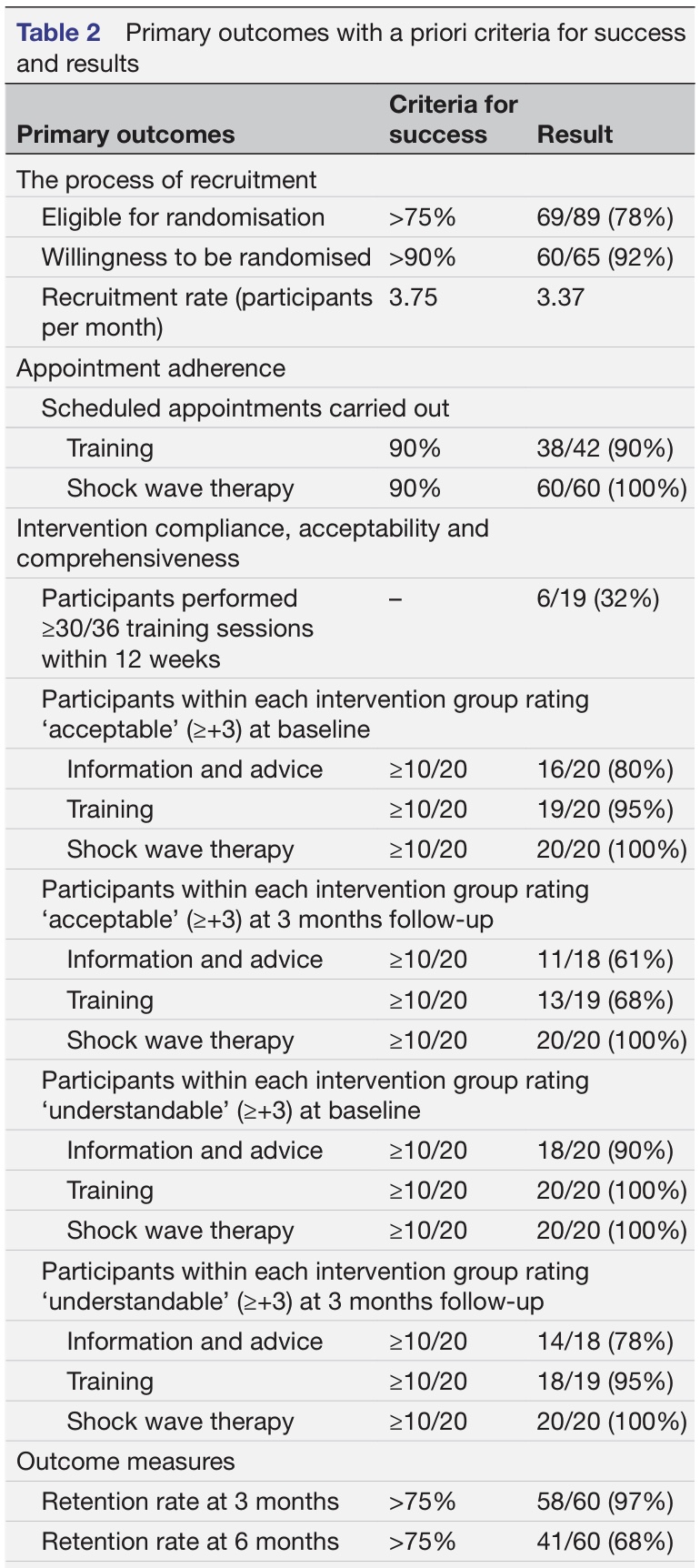
At baseline, essential demographics were collected, alongside information on pain characteristics and analgesic medications, and previous treatments.
Participants were randomly assigned to one of the three groups, but all groups received the same written and oral information about the etiology of lateral epicondylalgia, pathogenesis, treatment options, and the prognosis of lateral epicondylalgia. Furthermore, participants were informed that it is safe to use their elbow despite pain, since pain is not always a signal of harm. They were encouraged to use their arm as a way to regain and maintain function, but load management was recommended to guide gradual functional increases within tolerable pain.
Three different treatment arms were compared:
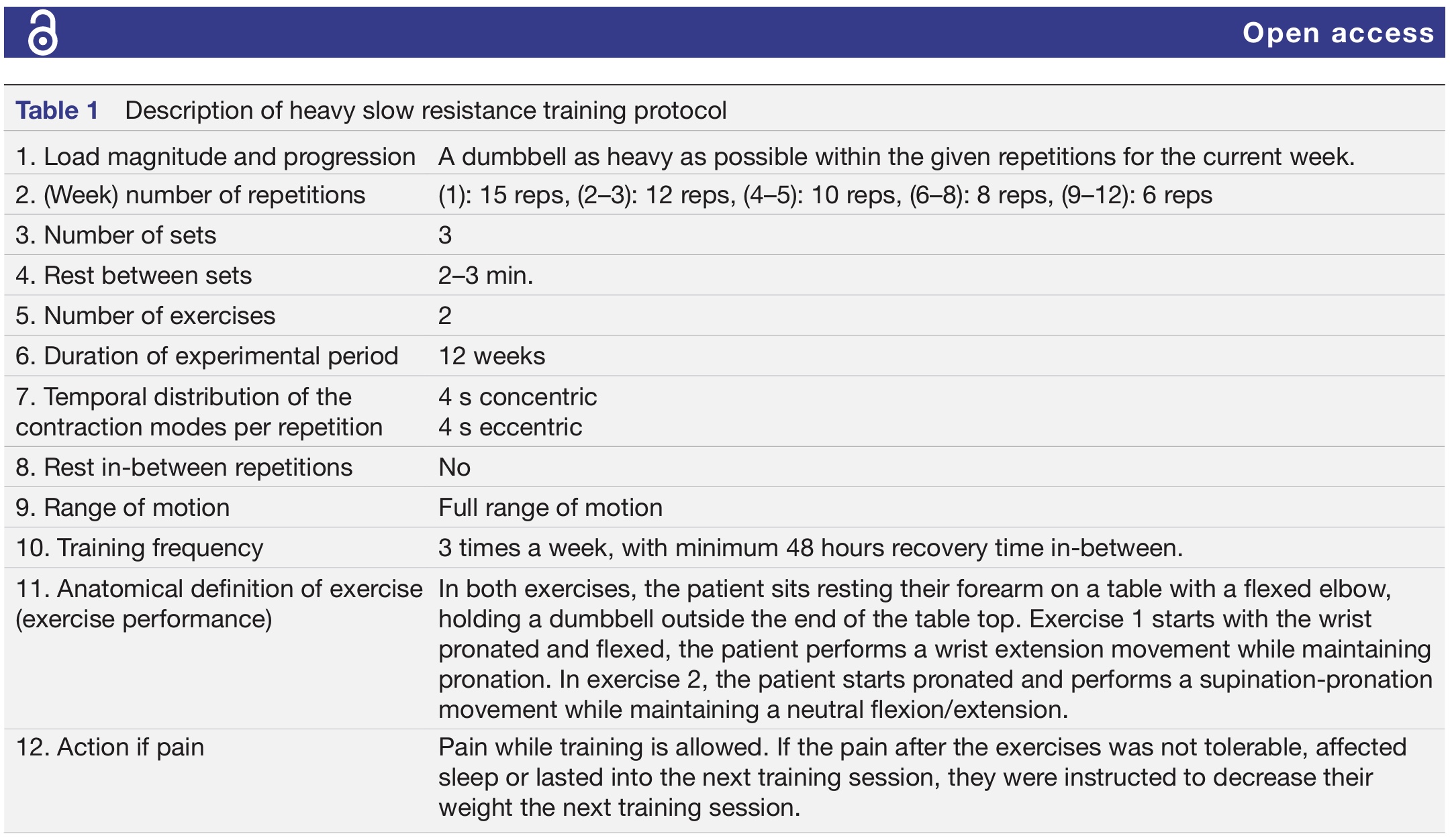
- Heavy slow resistance training
The exercise components were discussed individually and face-to-face by a postgraduate physiotherapist. A 12-week home exercise program was prescribed with a 3-times-per-week training requirement, totaling 36 sessions. Only two exercises were implemented: wrist extension exercise with eccentric control, and wrist pronation and supination. They were also taught how to stretch the wrist extensors and instructed to perform this stretch three times daily for three sets of 30 seconds.
Supervised appointments were made available according to the participant’s needs, allowing supervision for up to once per week, digitally or in person. They filled out a workout diary and were instructed on how to manage pain flares (see point 12 in the table under).
- Radial extracorporeal shockwave therapy
Patients randomized to this group were informed about the shockwave treatment and received 3 sessions spaced by approximately 1 week. They received 2000 impulses at 10 Hz with a low energy treatment between 1.5 and 3 BAR, at the area of maximal pain over the lateral epicondyle. No post-treatment restrictions were given.
- Information and advice
In a single individual face-to-face session with a postgraduate physiotherapist, information and advice was delivered according to the protocol. This session lasted up to 45 minutes and contained the same advice and information that was given to the other participants. In this session, participants were asked to specify their primary challenges and set their own recovery goals. Next, pacing and load management were discussed.
The physiotherapist also asked about their pain beliefs and pain coping strategies. Further, they were informed about the robustness of their elbow, despite their elbow pain. The natural course and good prognosis were emphasized, but it was told that it took time. They did not get restrictions, but instead, they were encouraged to use their elbows as normally as possible, regardless of pain.
Outcomes
The primary outcome measure was the feasibility of the trial, so the authors defined criteria for success a priori. To assess feasibility, the following outcomes were evaluated:
- Recruitment: the process of how many participants could be recruited and the recruitment rate were inspected.
- Appointment adherence: measured how many sessions were completedIntervention compliance: measured the number of completed training sessions
- Acceptability: scored on a 19-point Likert scale from -9 (I do not accept my treatment) to +9 (I completely accept my treatment)
- Comprehensiveness: scored on a 19-point Likert scale from -9 (I do not understand my treatment) to +9 (I completely understand my treatment)
- Retention rate: The completeness of data at 3 and 6 months was evaluated.
Based on these outcomes, a stoplight approach was used:
- Green-Go: Proceed with the RCT
- Amber-Amend: Proceed with changes
- Red-Stop: Do not proceed unless changes are possible
The following secondary outcome measures were defined:
- Patient-rated tennis elbow evaluation (PRTEE): with higher scores representing more disability
- Quick-Disabilities of the Arm, Shoulder, and Hand (Quick-DASH): from 0-100 with higher scores reflecting more disability
- 5-Level EuroQol-5D (EQ-5D-5L): from 0 (worst imaginable health state) to 100 (best imaginable health state)
- Numeric rating scale for current pain: from 0 (no pain) to 10 (worst imaginable pain)
- Global Rating of Change (GROC): from -6 (maximal worsening) to +6 (completely recovered)
- Pain-free grip strength, expressed in kilograms
Results
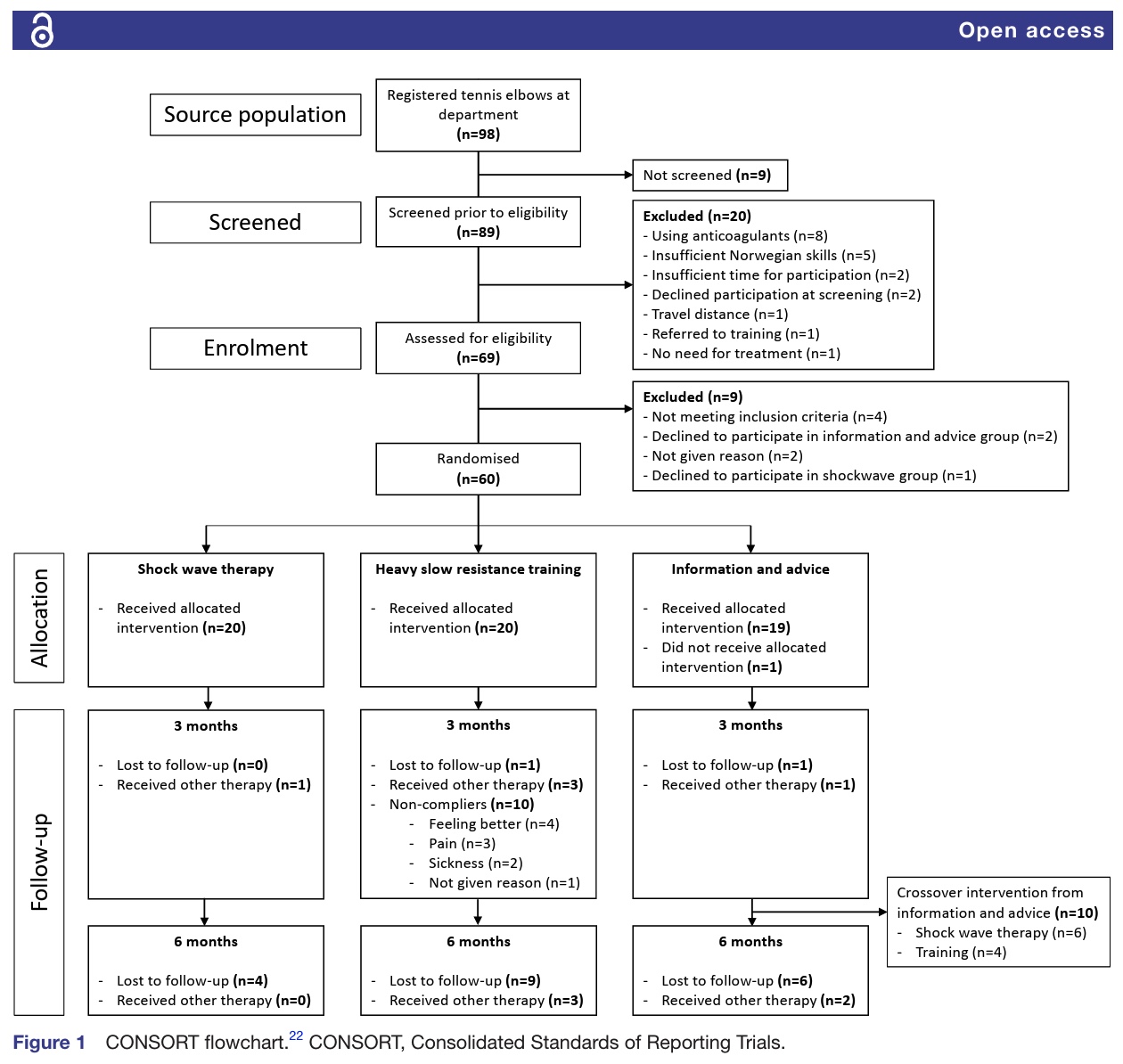
Sixty participants were included in the study, most of whom were female (68%). The sample had a mean age of 47.8 years (SD: 9.3 years). Ninety percent had an average symptom duration of more than 3 months. About two-thirds of the sample had received exercises for their lateral epicondylalgia before. Twenty participants were included in each group.
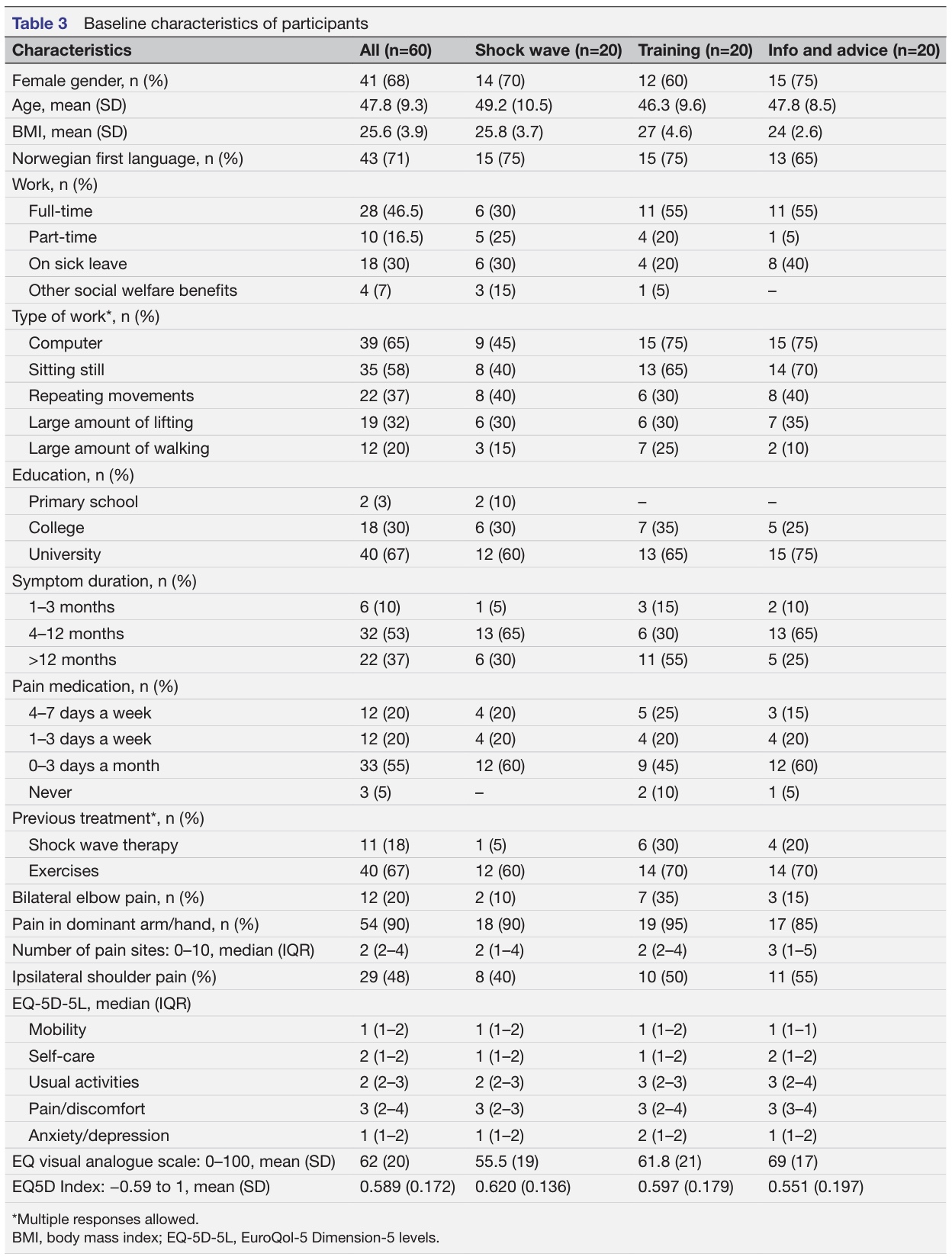
- Recruitment:
- 78% of screened patients were eligible for randomization (criterion was >75%)
- 92% of eligible patients were willing to be randomized (criterion was >90%)
- The recruitment rate was 3.37 participants per month, which was slightly below the a priori success cutoff of 3.75 participants per month.
- Appointment Adherence:
- Heavy Slow Resistance Training Group: 90% adherence to scheduled follow-up appointments (38 out of 42 appointments undertaken, successful).
- Shock Wave Therapy Group: 100% adherence to the three shock wave therapy sessions (60 out of 60 sessions completed; 3 sessions for every 20 participants).
- Intervention Compliance:
- Heavy Slow Resistance Training Group: Only 32% (6 out of 19 participants) complied by performing at least 30 out of 36 recommended training sessions within 12 weeks. This was below the success criteria for compliance. The main reason for non-compliance was reported as pain aggravation.
- Acceptance and Comprehensibility:
- All interventions were rated by participants as above the criteria for success for both acceptability and comprehensibility at baseline and 3-month follow-up. This means participants generally found their assigned treatment acceptable and easy to understand.
- Retention Rate:
- At 3 months: 97% retention (58 out of 60 participants), which was successful (criterion >75%).
- At 6 months: 68% retention (41 out of 60 participants), which was below the criteria for success (criterion >75%).
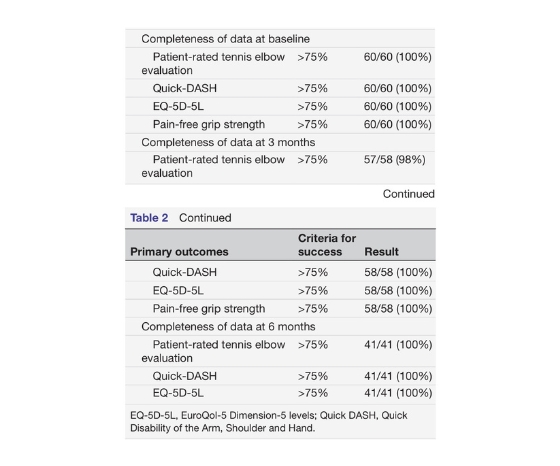
- Data Completeness:
- At baseline and 3 months: Completeness of data for all primary and secondary outcome measures was 98-100%, which was successful (>75%).
- At 6 months: Completeness of data remained 100% for the retained participants. However, given the lower retention rate at 6 months, the overall completeness of data relative to the initial sample size would naturally be affected.
In the heavy slow resistance training group, five participants reported pain aggravation following the exercises as an adverse event. Eight participants indicated that pain aggravation was the reason of non-compliance. Three participants from this group sought treatment alternatives during the 3-month follow-up period, followed by another three at 6 months.
In the shockwave group one participant reported seeking other treatments during the 3-month follow-up, but none did during the 6-month follow-up.
Ten participants from the information and advice group wanted a crossover treatment after the 3-month follow-up. Six of them opted for shockwave therapy, and four of them preferred heavy slow resistance training. One participant sought treatment alternatives at 3 months and two did at 6 months.
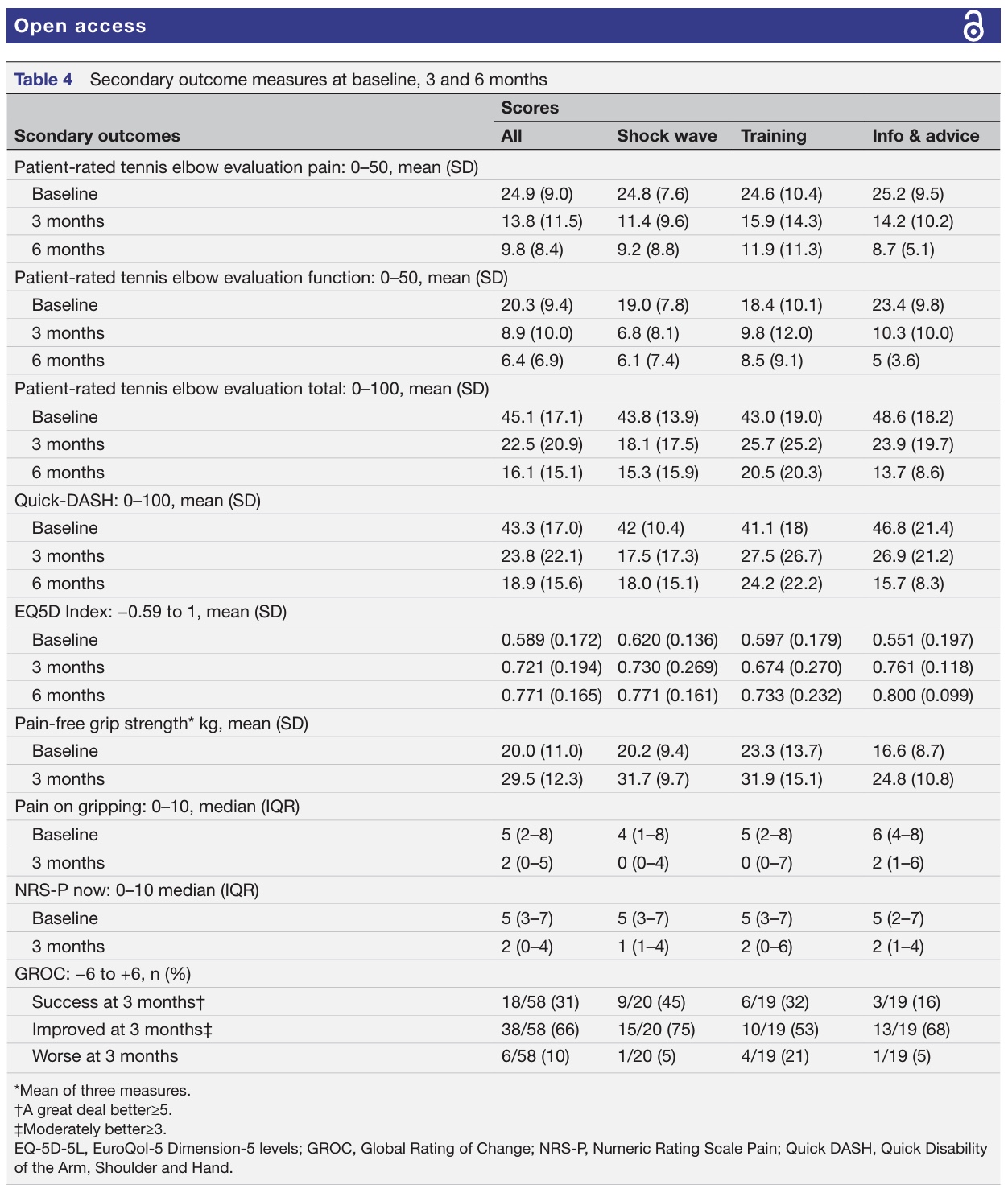
Secondary within-group changes revealed that all groups improved in the patient-reported outcomes measures and in the pain-free grip strength over the course of 3 and 6 months. All groups surpassed the minimal detectable change for the PRTEE (MDC: 8.9) and Quick-DASH (MDC: 11.2). Two-thirds of the participants reported being improved, while 10% indicated a worsening of their condition.
Questions and thoughts
The groups were informed about the possible treatment options before randomization. However, patient expectations were not evaluated. Since the majority of the participants had tried exercising before, it is realistic to assume that their expectations for exercise, since they did not achieve symptom resolution before, were on the low-end side. As this was not taken into account, this is a potential confounding factor, which should be considered in the full-scale RCT.
A simple exercise approach was used, no fancy exercises or equipment, but just the basics: progressive loading and consistency. But the trial revealed that for many, sticking to the plan was difficult, as compliance was low.
- Adherence in this study specifically referred to appointment adherence. Patients could opt for in-person appointments when deemed necessary. Adherence in this study measured whether participants actually showed up for scheduled in-person sessions and follow-up appointments.
- For the shockwave group, adherence was measured by whether participants attended the three shockwave therapy sessions. They had 100% adherence here.
- For the heavy slow resistance training group, adherence was measured by whether participants attended scheduled follow-up appointments. They had 90% adherence to these.
- Essentially, adherence was about showing up for the planned interactions with the researchers or therapists.
- Compliance, on the other hand, referred to intervention compliance, specifically for the home-based heavy slow resistance training program. It measured whether participants completed the recommended number of training sessions at home over the 12-week period.
- The protocol recommended 36 sessions (3 times a week for 12 weeks). The study set a criterion for compliance as performing at least 30 out of these 36 sessions.
- The result was that only 32% of the HSR group met this compliance criterion, that is, 6 out of 19 participants.
- Compliance was about doing the prescribed activity as instructed, particularly for the self-managed home exercise program.
So, summarized:
- Adherence = Showing up for appointments/sessions.
- Compliance = Doing the home exercises as recommended.
A patient panel was included to give recommendations to enhance the comprehensibility of the study information and materials. This helps to ensure the study’s design and materials were patient-centered and pragmatic. As such, it is considered a strength of the study, as it increases the likelihood that the research addresses questions important to patients and is conducted in a way that is acceptable and comprehensible to them
The authors used a stoplight approach, which is essential to reduce research waste. This approach is helping researchers determine the readiness and necessary adjustments for a larger trial, which in essence the goal of a feasibility trial.
Talk nerdy to me
As I wanted to compare this feasibility study to the pilot study from Divya Mary et al. (2025) we reviewed last week, we can note the following:
- Trial Design & Reporting:
- Sveinall et al.:
- Clearly states it’s a randomized controlled feasibility trial with a parallel design. Reports according to the 26-item checklist from the CONSORT 2010 statement: extension to randomized pilot and feasibility trials. This is excellent and aligns perfectly with best practices for reporting such studies. Clearly defines its a priori success criteria for feasibility outcomes.
- Divya Mary et al.:
- Despite claiming to be an RCT (Level 1 evidence), it describes itself as a “pilot study” in the title and abstract, which typically precedes a full RCT and often has different methodological expectations (e.g., sample size calculations are for feasibility, not effectiveness). The reporting, particularly regarding randomization and blinding, is vague. It lacks a clear statement of adherence to any reporting guidelines (like CONSORT), making it harder to assess its quality comprehensively.
- Randomization & Blinding:
- Sveinall et al.:
- Details a computer-generated randomisation sequence with blocks of variable sizes, unknown to the treating physiotherapist. This is a robust method.
- Explicitly states that due to the nature of the interventions (exercise vs. shockwave vs. advice), neither the physiotherapist nor the participants could be blinded. This is an inherent limitation for pragmatic trials involving distinct interventions, but is openly acknowledged. The feasibility of assessor blinding was not evaluated, which is a minor limitation for secondary outcomes.
- Divya Mary et al.:
- States “Participants… were randomly assigned to either HSR Group or CE Group.”, but lacks crucial details on the randomisation process (e.g., method of generation, allocation concealment). Without this, true randomization and prevention of selection bias cannot be confirmed. There is no mention of blinding of participants, therapists, or outcome assessors, which is a major methodological shortcoming for an effectiveness trial, potentially introducing performance and detection bias.
- Participants & Recruitment:
- Sveinall et al.:
- Detailed inclusion and exclusion criteria, including clinical provocation tests. Pragmatic exclusion criteria reflecting real-world patients. Reports success rates for eligibility and willingness to be randomized.
- Recruitment rate slightly below the a priori target.
- Divya Mary et al.:
- Provides inclusion/exclusion criteria.
- Small sample size (N=24 total, 12 per group) is mentioned as “more than sufficient” based on power calculation for a 40% difference in effect, which is unrealistically large for a pilot study and highly susceptible to chance findings. Their demographics (45-65 years, unilateral LE, symptoms >12 months) are quite specific, potentially limiting generalizability.
- Interventions:
- Sveinall et al.:
- The heavy slow resistance training protocol is reported using the Consensus on Exercise Reporting Template (CERT), providing excellent detail for replication (e.g., load progression, sets/reps, tempo, pain guidance). The shockwave protocol is also detailed. All groups received the same common general information.
- The “voluntary supervision” for the heavy slow resistance training group and varied uptake could introduce inconsistency.
- Divya Mary et al.:
- Descriptions are less detailed than CERT, making exact replication difficult. For example, the heavy slow resistance training in this study mentions “higher intensities… 70%-80% of 1RM” but then “initiating with… 15RM,” which are contradictory if 1RM is a single max lift. The conventional exercise group includes a broad range of exercises (rotations with/without weight, lifts, bends, stretches, squeeze, twist) which makes it hard to pinpoint what contributes to any observed effects, although effectiveness can not be primed due to the nature of the study and it shortcomings.
- Outcome Measures & Data Collection:
- Sveinall et al.:
- Clearly defined a priori feasibility criteria for success. Uses validated outcome measures (PRTEE, Quick-DASH, EQ-5D-5L, pain-free grip strength). High data completeness at 3 months.
- Retention rate at 6 months below the success criteria. No health economic questionnaires, which could inflate data completeness impressions.
- Divya Mary et al.:
- Uses validated outcome measures (PRTEE, PSFS, grip strength), but relies heavily on self-reported measures with less focus on objective or blinded assessment. The primary outcome seems to be a statistical difference rather than feasibility metrics for a pilot study. “The study focused on short-term improvements… avoiding long-term follow-up due to participant burden and resource limitations,” which is acceptable for a pilot but limits clinical insight into sustained benefits.
Part 2: Feasibility Trial Requirements & Lessons Learned
- Sveinall et al.:
- Feasibility Focus: This study is a textbook example of a well-conducted feasibility trial. It explicitly sets a priori success criteria for recruitment, adherence, compliance, acceptance, retention, and data completeness.
- Key Feasibility Results:
- Successful: Eligibility, willingness to randomize, appointment adherence (especially shockwave), acceptability/comprehensibility of all interventions, retention/data completeness at 3 months.
- Challenging: Recruitment rate slightly under target. Crucially, low compliance with heavy slow resistance training in lateral epicondylalgia (32%) due to pain aggravation. Retention at 6 months also dropped.
- Lessons Learned: heavy slow resistance training needs significant adaptations (e.g., more supervision, careful pain management, slower progression) before a full effectiveness RCT can be considered. Shockwave and advice are feasible to study further, but shockwave needs a sham control. The 6-month follow-up method (using emails) might need a review.
- Divya Mary et al.:
- Feasibility Focus: Although titled a “pilot study,” its explicit conclusion is about effectiveness (“heavy slow resistance training exercise demonstrates superior effectiveness over conventional exercises”). This is a fundamental mismatch with the purpose of a pilot/feasibility study, which is to assess study processes, not treatment efficacy.
- Key Feasibility Aspects (implicitly inferred):
- Recruitment of 24 participants was seemingly achieved.
- Compliance/adherence are not reported as primary outcomes, but the fact that a 12-week intervention was completed for 24 participants suggests it was possible, albeit without specific metrics.
- Lessons Learned: This study, despite its findings, highlights the pitfall of premature effectiveness claims from pilot data. Its primary value is perhaps as a small, early signal, but not as definitive evidence for heavy slow resistance training’s superiority.
Summary
- Sveinall et al.:
- Clear study design, explicit feasibility objectives with a priori success criteria, robust randomization process, detailed intervention reporting (CERT), and patient and public involvement in study design. Its transparency in reporting limitations (e.g., lack of blinding, low HSR compliance) is a major strength.
- Provides valuable information for designing a future definitive trial.
- The low heavy slow resistance training compliance is a key finding that needs addressing.
- Reduced retention at 6 months (highlights challenges with longer follow-ups).
- Lack of sham shockwave group (limits conclusions on shockwave effectiveness, but this was a feasibility trial, so acceptable in this context).
- Divya Mary et al.:
- Attempts to investigate heavy slow resistance training in lateral epicondylalgia, where evidence is scarce. Uses relevant outcome measures (PRTEE, grip strength), but the sheer ambition to claim “superior effectiveness” from such a small pilot can not be endorsed.
- Significant methodological shortcomings: Vague randomization and lack of allocation concealment, no blinding of participants, therapists, or assessors.
- Inappropriate sample size calculation and effectiveness claims for a pilot study.
- Less detailed intervention reporting, making replication difficult.
Take-home messages
The study found high adherence to in-person exercise appointments and shockwave sessions, indicating that participants were willing and able to attend in-person interactions. However, compliance with the home program was low, suggesting that while participants might have accepted the idea of heavy slow resistance training in lateral epicondylalgia (high acceptability), consistently performing the exercises at home proved challenging, largely due to pain aggravation. Shockwave may be a valid alternative, but, considering the feasibility nature of the study, it should first be thoroughly evaluated using a sham-controlled RCT.
Several issues encountered in this study can be taken into account when you want to implement resistance training in lateral epicondylalgia patients:
- As adherence to resistance training was successful, you might want to consider in-person appointments rather than just prescribing home exercises, or at least prescribe home exercises with an obligatory follow-up appointment every week.
- Monitor pain, and keep educating your patient about the stubbornness of lateral epicondylalgia. But emphasize that pain does not equal harm, and repeat! Especially since pain was the most important factor for people to be less compliant.
- Don’t overcomplicate rehabilitation; rather, focus on correcting pain behavior and cognitions, especially when they are maladaptive.
- Don’t waste prescribed sessions, knowing that the natural course of lateral epicondylalgia requires time
Reference
Sveinall H, Brox JI, Engebretsen KB, Hoksrud AF, Røe C, Johnsen MB. Heavy slow resistance training, radial extracorporeal shock wave therapy or advice for patients with tennis elbow in the Norwegian secondary care: a randomised controlled feasibility trial. BMJ Open. 2024 Dec 20;14(12):e085916. doi: 10.1136/bmjopen-2024-085916. PMID: 39806585; PMCID: PMC11667321. https://pubmed.ncbi.nlm.nih.gov/39806585/
21 OF THE MOST USEFUL ORTHOPAEDIC TESTS IN CLINICAL PRACTICE
We have comprised a 100% Free E-Book containing 21 of the hands-down most useful orthopedic tests per body region guaranteed to help you reach a proper diagnosis today!