Recognizing Degenerative Cervical Myelopathy in Physiotherapy Practice

Introduction
Degenerative cervical myelopathy, or cervical spondylotic myelopathy, is a clinical syndrome in which progressive narrowing of the spinal canal due to degenerative changes leads to spinal cord compression. Due to the progressive nature (in atraumatic cases), early symptoms can be mild and easy to miss in clinical practice. Missing those early signs and symptoms of this condition can lead to ongoing worsening over time, with some cases developing severe signs of spinal cord compression that may include bladder and bowel dysfunction, paralysis, etc.
Physiotherapists play an important role in early identification, as we will encounter people presenting with subtle signs of this condition. This article delves into the aspects every physiotherapist should know about, since recognizing degenerative cervical myelopathy early allows for adequate follow-up and prevention of the occurrence of severe and irreversible neurological damage.
Methods
This paper involved a comprehensive expert-led, non-systematic literature review designed to create an educational and practical resource, specifically designed for physiotherapists. Timely recognition of degenerative cervical myelopathy is tough, as there is no go-to approach or validated screening tool available. Therefore, the authors aimed to summarize and enhance physiotherapists’ essential knowledge regarding the differential diagnosis and management of patients with degenerative cervical myelopathy.
Results
The authors delved into the literature, covering the following aspects.
Neuroanatomy and etiopathogenesis
The spinal cord consists of the gray matter, centrally located, and the white matter surrounding it. The anterior part of the white matter contains the ascending contralateral spinothalamic tract, which is responsible for carrying signals of pain, temperature, and fine touch to the brain, and the descending ipsilateral anterior corticospinal tract, responsible for motor function.
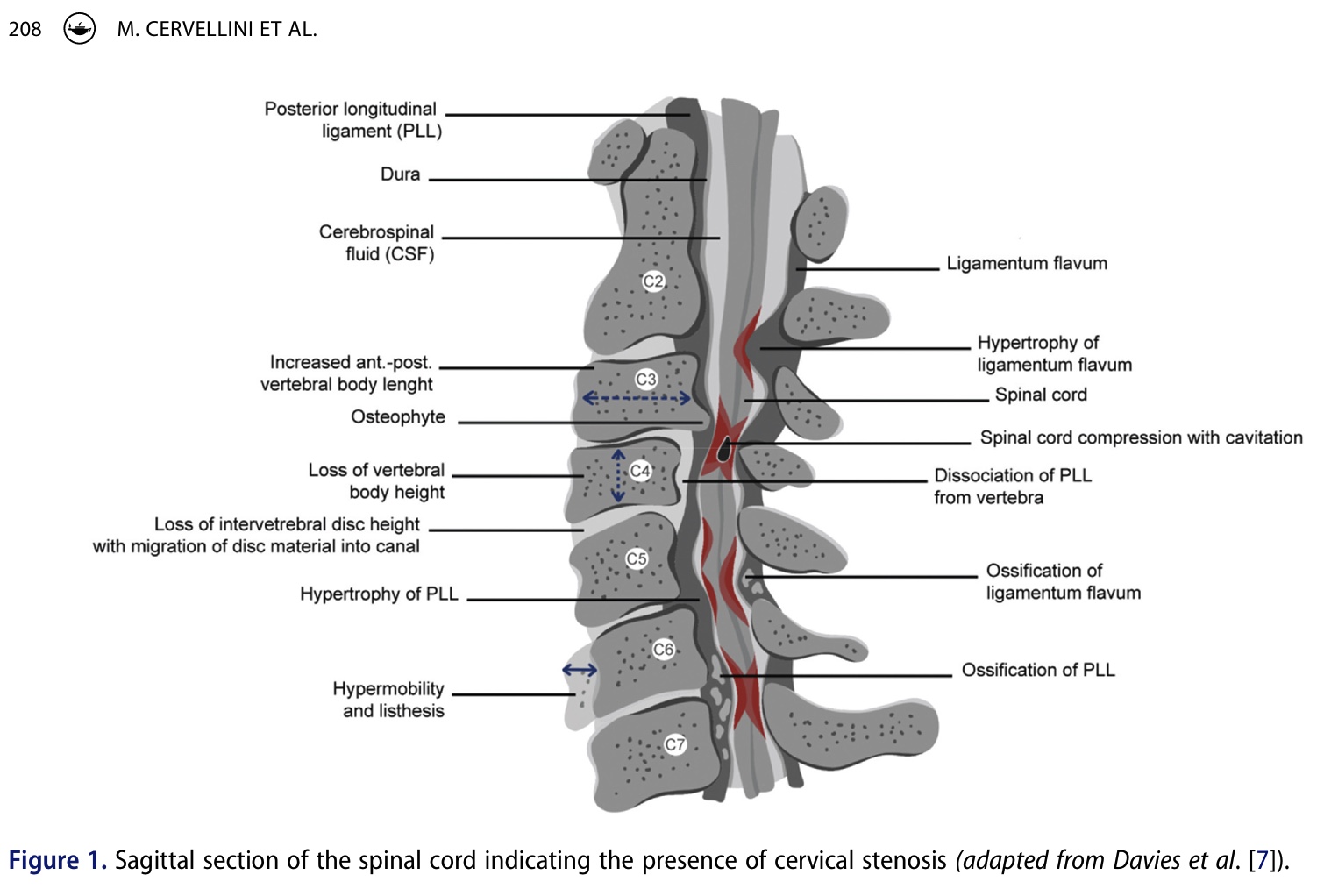
In degenerative cervical myelopathy, the most common cause is cervical spine stenosis. The stenosis can be congenital or acquired, where the latter is mostly due to intervertebral disc degeneration and spondylosis. The stenosis leads to reduced local blood flow, which in turn results in ischemia of the spinal cord. By this reduced perfusion, the nerve fibers are demyelinating, axons degenerate, and ultimately, this impairs signal transmission.
The symptoms fluctuate depending on the location of the cord compression. Pain can be present in the neck, shoulders, arms, and signs of sensory deficits, motor weaknesses, impaired gait, and/or bladder dysfunction can be present. When the anterior white matter is involved, characteristically, upper motor neuron syndrome occurs with spasticity and hyperreflexia. According to the authors, grey matter involvement seems to be less severe and has a more favorable prognosis.
Besides the upper motor neuron signs, degenerative cervical myelopathy patients can also experience lower motor neuron problems due to nerve root compression co-occurring with the central canal stenosis.
History taking
In history taking, a wide variety of symptoms can be present. The table below summarizes the frequencies of symptoms reported by people with degenerative cervical myelopathy, and classifies them per stage of occurrence (into early signs, middle, and late signs). Ideally, we should already recognize the early signs and symptoms. Inquiring about signs of hand numbness, hand paresthesia, gait impairment, neck and/or shoulder pain, and the impact on fine motor skills may help recognizing degenerative cervical myelopathy early on. When a patient is confronted with bilateral carpal tunnel syndrome, you should always be aware that there may be an underlying myelopathy present. The Lhermitte’s sign, which is “a transient electric shock sensation down the spine and extremities caused by neck flexion”, can be present, but mostly in a minority of subjects. When it is present, the Lhermitte sign is highly specific (Sp 97%).
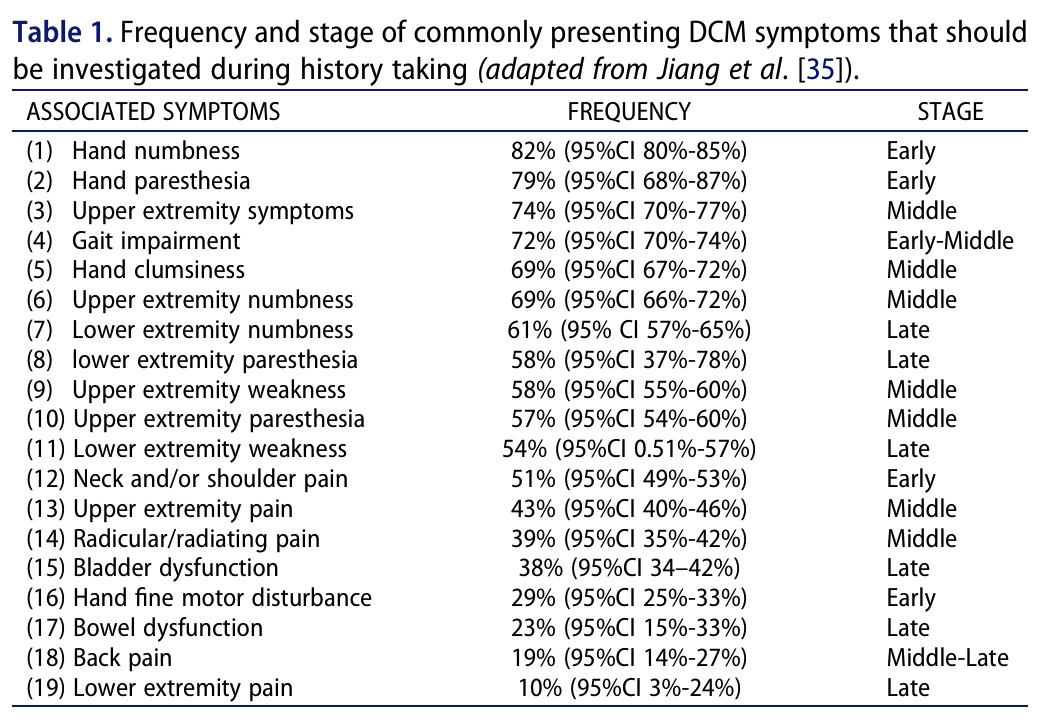
It is crucial to ask patients if they are experiencing these symptoms, as for patients, the possible symptoms may seem unrelated to their neck or shoulder pain. A thorough assessment of red flags is essential.
Clinical testing
A thorough examination involves both upper and lower motor neuron assessment. For the upper motor neuron, focusing on hypertonic reflexes is essential. You should examine the following reflexes:
- Hoffmann’s sign
- Tromner sign
- Babinski sign
- Romberg’s sign
- deep tendon hyperreflexia of the upper and lower limbs
- Inverted supinator sign
The Tromner sign showed the highest diagnostic utility. The Babinski sign, though highly specific, indicates a poor mJOA score and is a key clinical indicator warranting expedited referral for diagnostic imaging and surgical consultation. Deep tendon hyperreflexia is highly sensitive, particularly in the lower extremities. The presence of these signs is associated with greater disease severity, so the absence does not necessarily mean that degenerative cervical myelopathy is absent. Your patient can be in the early stages of the condition, where such signs and symptoms are not (always) present (yet). Reevaluation over time might be indicated.
With regard to the lower motor neuron assessment, we should evaluate the motor function of the patient. This includes assessment for:
- Motor dysfunction: Early signs include progressive weakness of intrinsic hand muscles. Grip strength and hand clumsiness are early indicators. While accuracy is not reported, positive grip and release tests and the finger escape sign can suggest cord impairment. Weakness is typically non-myotomal, unlike cervical radiculopathy.
- Gait changes: Reduced cadence, increased step width, decreased step length, and longer stride time are observed. Gait impairments are early manifestations in 80% of cases according to the Nurick grading system. The 30-meter walking test and tandem gait/heel-to-toe walking can quantify these. The Romberg test is another option, yet less sensitive since a positive Romberg test may be caused by a variety of conditions. Similarly, gait impairments are not exclusively caused by degenerative cervical myelopathy, hence why these findings should be integrated alongside other clinical signs and findings from the patient history.
The authors recommend conducting a cervical range of motion assessment in all directions to determine symptom reproduction and to discriminate between cervical radiculopathy and degenerative cervical myelopathy.
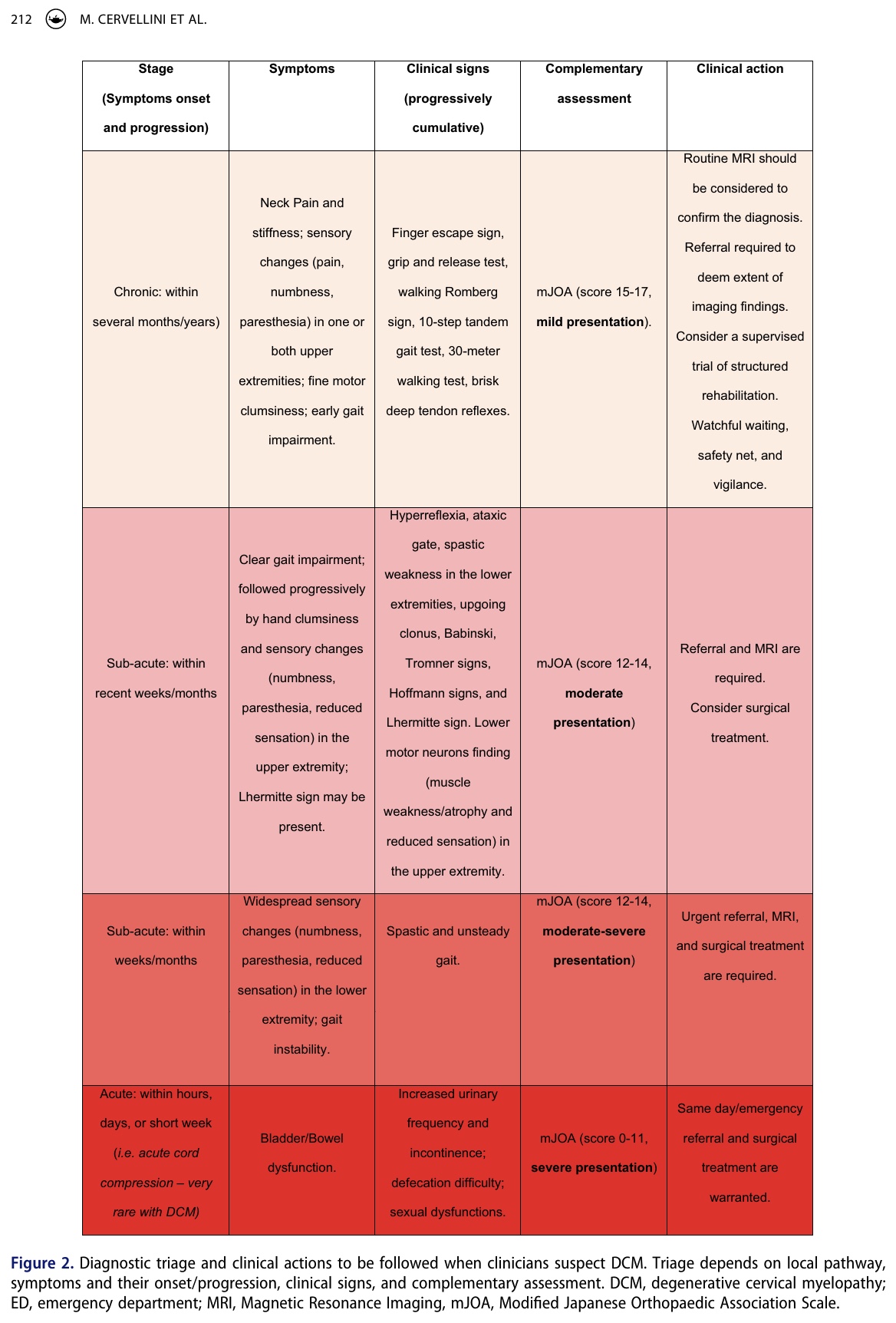
In the early stages of degenerative cervical myelopathy, clinical tests may be negative, and early signs and symptoms may seem mild or fluctuating over time. That is where your clinical reasoning may make a difference. The IFOMPT framework developed a decision tool to help you make the right decisions depending on the stage and severity of the presentation.
Outcome measures and complementary assessment
Functional impairments and their severity can be evaluated using the modified Japanese Orthopedic Association (mJOA) scoring system or the Nurick classification. While the mJOA focuses on functional abilities, including upper and lower limb motor function, sensation, and sphincter function, the Nurick grading system evaluates functional status, including gait impairments. Scores of 12 or less on the mJOAS are related to poorer neurological recovery, compared to those with scores above 12.
Imaging
When clinical signs point to a possible presence, a gold standard T2-weighted MRI scan is necessary for recognizing degenerative cervical myelopathy. This demonstrates high specificity and sensitivity when there is a correlation between the clinical findings and the imaging results. Imaging findings in the absence of clinical symptoms are not a valid diagnosis of degenerative cervical myelopathy, as there is a high prevalence of asymptomatic spinal cord compression.
MRI is the gold standard. The authors recommend referring for MRI, even if electromyography suggests bilateral carpal tunnel syndrome.
CT scans may help in surgical planning and decision-making, or can be used in case an MRI is contraindicated. Plain radiography is not diagnostic, but flexion-extension radiographs can be taken if a spondylolisthesis with suspected instability is present.
Interpretation of findings and physiotherapy management
As physiotherapists, we play a crucial role in recognizing degenerative cervical myelopathy. But it can be difficult to differentiate between other conditions as the condition can masquerade as cervical radiculopathy or bilateral carpal tunnel syndrome. The unpredictable and variable progression of degenerative cervical myelopathy symptoms means that physiotherapists should always inquire about a patient’s full past medical history. We need to be adept at recognizing subtle clues during the subjective history taking that might point towards a degenerative cervical myelopathy hypothesis. This hypothesis should then be confirmed with a targeted physical examination. Clinical action to take (safety-netting, watchful waiting, referral, urgent referrals) can be aided by the clinical decision tool presented above (Figure 2).
Education and safety-netting
Physiotherapists are responsible for educating patients about the potential progression of degenerative cervical myelopathy, as we are often the first in line to be confronted with affected patients. This includes explaining the nature of the condition and what symptoms to watch for.
- Safety Netting: In the context of Degenerative Cervical Myelopathy, safety netting refers to the proactive steps taken by healthcare professionals to educate patients and minimize the risk of worsening their condition or experiencing further injury. Essentially, safety netting empowers patients with the knowledge to manage their condition responsibly, avoid potential harm, and know when to seek timely medical care. Key aspects include:
- Educating patients by informing them about the potential progression and the symptoms to watch for
- Avoiding harmful activities: A key piece of advice, according to the authors, is to strongly recommend that patients avoid whiplash-type injuries and cervical manipulation, as these can potentially exacerbate spinal cord compression and lead to further neurological deficits. While avoiding the latter is fairly easy, whiplash events are unpredictable. In the case of a patient sustaining a whiplash, he or she should have received information in the safety-netting “briefing” on how to monitor related symptoms and when to undertake action.
- Recognizing red flags by ensuring patients are aware of “red flag” symptoms that require urgent medical attention, such as spastic paraparesis or bowel/bladder dysfunction.
Patients often find it beneficial to get information regarding the diagnosis, therapy, rehabilitation, residual disability, and adopting lifestyle changes. Using patients’ MRI scans as an instructional tool may improve comprehension of pathophysiology, foster the need for treatment, and provide a sense of validation. Be aware that degenerative cervical myelopathy is a problem that is mostly managed by surgeons, so physiotherapists must collaborate with other healthcare providers. Given the condition’s complexity and the high potential of misdiagnosis, open communication, timely access, and a common language should be encouraged.
Management
While mild cases can be managed conservatively, under the supervision of the treating physician and physiotherapist, surgery is recommended for moderate to severe cases of degenerative cervical myelopathy. When the management of this condition is conservative, the focus is to avoid progression of the condition, but a great deal of people who are managed conservatively at first will eventually require surgical care. It is reported that 23%-54% of patients will progress to surgery within a follow-up period between 29 and 74 months. In this light, physiotherapists should try to avoid progression and monitor signs and symptoms over time, ultimately delaying the need for surgery. Yet, surgery may be required eventually, as conservative care typically does not lead to long-lasting effects.
Questions and thoughts
Reading this review on degenerative cervical myelopathy has certainly got me thinking… It highlights how often we might be seeing these patients in our musculoskeletal clinics without even realizing it, mistaking their symptoms for more common things like radiculopathy or just age-related changes.
Given the massive diagnostic delays this paper talks about, averaging over two years, I can’t help but wonder: could we, as physiotherapists, be better equipped on the front lines? Is there a way to develop a really practical, validated screening tool specifically for us in musculoskeletal practice? What would that even look like? What essential criteria would it need to include to be effective without being overly complex? Jiang et al. in 2023 performed a meta-analysis of the value of clinical signs and tests for recognizing degenerative cervical myelopathy, which we summarized in the following video.
The review stresses how important it is to work with other healthcare professionals. But honestly, what are the most effective ways for us to collaborate with neurologists, surgeons, and others involved? How can we ensure smooth communication and timely referrals? It feels like sometimes there are disconnects, and this paper reinforces that we need to bridge those gaps for our patients’ sake.
When it comes to managing the milder cases conservatively, I’m always looking for clearer guidance. The paper mentions exercise, but mentions no specific types, intensities, frequencies, or durations that have actually been shown to work.
Overall, this paper is a great reminder of the complexities of degenerative cervical myelopathy and our vital role in identifying and helping manage it, but it also sparks a lot of practical questions about how we can do that even better in our day-to-day practice.
Talk nerdy to me
This article is a narrative review, meaning the authors selected and synthesized existing literature to provide a broad overview of degenerative cervical myelopathy. Unlike a systematic review or meta-analysis, there isn’t a pre-specified methodology for literature searching, study selection, or critical appraisal of individual studies. This means the information presented reflects the authors’ interpretation of the available evidence.
While convenient for summarizing a large body of knowledge, it introduces the potential for selection bias (authors might unknowingly favor studies that align with their perspectives) and a lack of transparency in how the evidence was weighted.
When discussing the accuracy of clinical signs, the review provides values for sensitivity (Sn) and specificity (Sp), along with positive likelihood ratios (+LR) and negative likelihood ratios (-LR). Let’s break down what these mean:
- Sensitivity (Sn): The proportion of people with the condition who test positive. A high sensitivity means the test is good at ruling out the condition when the result is negative (SNOUT – Sensitivity Negative, Out). For example, the Tromner sign has a high sensitivity (93-94%), suggesting if it’s negative, degenerative cervical myelopathy is less likely.
- Specificity (Sp): The proportion of people without the condition who test negative. A high specificity means the test is good at ruling in the condition when the result is positive (SPIN – Specificity Positive, In). The Lhermitte sign has a high specificity (97%), meaning if it’s positive, degenerative cervical myelopathy is highly likely.
- Positive Likelihood Ratio (+LR): How many times more likely it is that a person with the condition will have a positive test result compared to a person without the condition. A +LR > 10 is considered strong evidence to rule in a diagnosis, while a +LR between 5-10 is moderate, and 2-5 is weak.
- Negative Likelihood Ratio (-LR): How many times more likely it is that a person with the condition will have a negative test result compared to a person without the condition. A -LR < 0.1 is considered strong evidence to rule out a diagnosis, while a -LR between 0.1-0.2 is moderate, and 0.2-0.5 is weak.
Looking at the provided values:
- Tromner Sign (Sn 93-94%; Sp 79-100%; +LR 4.41; -LR 0.065-0.071): High sensitivity and moderate-to-high specificity. The low -LR (strong evidence to rule out) suggests it’s a good screening test, while the moderate +LR suggests it’s helpful for ruling in, but not definitively.
- Babinski Sign (Sn 7-36%; Sp 93-100%; +LR 4.50; -LR 0.064-0.093): Low sensitivity but very high specificity. This means it’s not good at detecting all cases (many people with degenerative cervical myelopathy might have a negative Babinski), but if it’s positive, it’s highly suggestive of degenerative cervical myelopathy. The low -LR is still useful for ruling out when negative, but the low sensitivity means a negative result doesn’t rule it out strongly enough on its own.
- Hoffmann Sign (Sn 31-89%; Sp 50-100%; +LR 1.15-10.50; -LR 0.011-0.095): This sign shows a wide range in both sensitivity and specificity across different studies, indicating less consistency in its diagnostic utility compared to the Tromner and Babinski signs. The +LR and -LR values are less extreme, suggesting it provides weaker evidence for both ruling in and ruling out degenerative cervical myelopathy.
While this review provides a valuable overview for physiotherapists, it’s important to consider its potential limitations:
- Non-systematic nature: As a non-systematic review, the authors’ search strategy and selection of literature are not explicitly defined. This can introduce bias in the presented information, as certain studies or perspectives might be inadvertently or intentionally favored. The lack of a critical appraisal of individual study quality also means the strength of the evidence for each point is not consistently evaluated.
- Reliance on existing literature: The review is a synthesis of existing research. If the underlying literature has gaps, biases, or limitations (e.g., small sample sizes, methodological flaws, lack of diverse populations), these will be reflected in the review.
- Generalizability: The findings and recommendations are based on a review of literature, which may not perfectly translate to every individual patient or clinical setting. Factors like patient comorbidities, cultural context, and access to resources can influence the applicability of the information. No information about specific populations (ages, clinical settings, etc) was provided, which is a limitation.
- Lack of specific intervention protocols: While the review discusses physiotherapy management in general terms, it doesn’t provide detailed, evidence-based protocols for specific interventions. Physiotherapists looking for step-by-step guides on exercise programs or manual therapy techniques for degenerative cervical myelopathy may need to consult additional resources.
Take-home messages
Degenerative cervical myelopathy is a serious condition caused by progressive compression of the spinal cord in the neck. It can often be mistaken for more common musculoskeletal issues, leading to significant delays in diagnosis. These delays can have severe and irreversible neurological consequences.
Physiotherapists play a crucial role in early recognizing degenerative cervical myelopathy. By having a strong understanding of its clinical presentation, key signs, and the limitations of diagnostic tools, physiotherapists can identify potential cases and ensure timely referral for definitive diagnosis and management.
While conservative management may be considered for mild cases, surgery is often necessary for moderate-to-severe degenerative cervical myelopathy to prevent further neurological deterioration and potentially improve function. Interdisciplinary collaboration is essential for optimal patient care.
A potential threatening limitation to the conclusions and validity of the findings in this review is its non-systematic nature. Without a transparent and rigorous methodology for searching, selecting, and appraising the literature, there’s a risk of bias in the information presented, which could influence the understanding and management recommendations for degenerative cervical myelopathy.
Reference
21 OF THE MOST USEFUL ORTHOPAEDIC TESTS IN CLINICAL PRACTICE
We have comprised a 100% Free E-Book containing 21 of the hands-down most useful orthopedic tests per body region guaranteed to help you reach a proper diagnosis today!