When to Consider a Corticosteroid Injection for RCRSP?

Introduction
Rotator cuff-related shoulder pain (RCRSP) remains one of the most commonly encountered musculoskeletal conditions for which people seek care. The debate of whether to use a corticosteroid injection for RCRSP relief or not is ongoing, despite active interventions are recommended. The potential (short-term) benefits should be captured and analyzed for their associated risks and side effects. In this light, the current systematic review tried to focus on the effectiveness of a corticosteroid injection in RCRSP and compared it to physiotherapy-related interventions or as a standalone treatment.
Methods
A systematic review with meta-analysis was conducted, and the protocol was prospectively registered. Adults from 18 years and older who were affected by RCRSP were included. The authors used a broad definition of RCRSP (including the search terms “impingement”, “tendinitis”, “tendinopathy”, “subacromial bursitis”, and “partial rotator cuff tears”) due to inconsistencies in reporting and uncertainties around the diagnosis of this condition.
The studied interventions included:
- The experimental: single or multiple corticosteroid injections in the subacromial space only, alone or in combination with an anesthetic injection or any other physiotherapy intervention.
- The comparator: physiotherapy intervention alone, including exercise, manual therapy or physical agents, alone or in combination with each other.
Outcomes of interest included:
- Pain, measured
- Function or disability
- Quality of life
- Patient-rated overall improvement
- Adverse events
The data was collected and subdivided into short (≤ 6 weeks), mid (6-12 weeks), and long-term (> 12 weeks) follow-up. In case studies had multiple assessment times, the longest one was used. Negative differences favor the experimental intervention.
Results
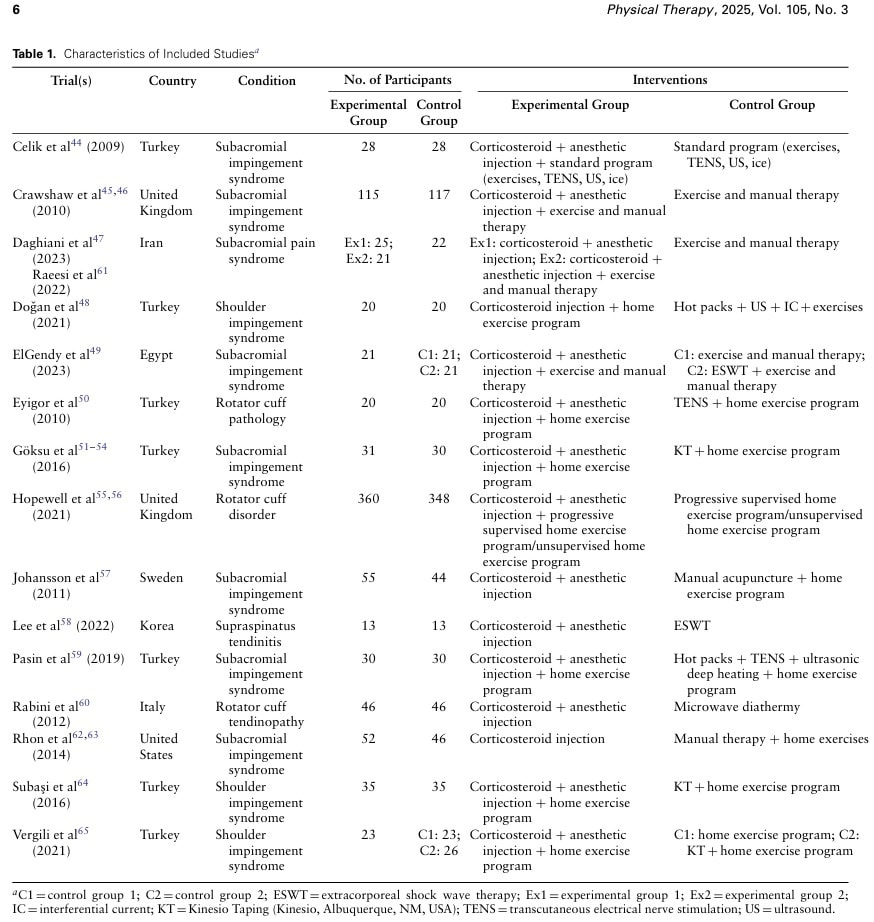
A total of 15 studies were included in the systematic review, analysing 1785 participants. Nearly half of the studies were conducted in Turkey, but this accounted for less than 25% of the total population included.
All studies were judged as having a high risk of performance and detection biases.
Corticosteroid injection for RCRSP plus anesthetic plus exercise versus exercise
From the meta-analysis of 708 participants (one study) was found, with moderate certainty, that additional corticosteroid injections were more effective in reducing pain and improving function at short term than exercise alone. There was no difference at the mid and long-term follow-up. Another RCT of 40 participants that was not suited for meta-analysis found no effect at short-, nor at long-term follow-up.
Corticosteroid injection plus anesthetic plus manual therapy plus exercise versus manual therapy plus exercise
Descriptive analysis of 317 participants revealed that adding a corticosteroid injection was more effective for relieving pain in the short term, but not at mid- or long-term follow-up, with low to very low certainty of evidence. Similarly, for functional improvements, the short but also mid-term follow-up favored an additional corticosteroid injection, which was not retained in the long term.
Corticosteroid injection plus anesthetic plus exercise versus physical agents plus exercise
Very low-certainty evidence from descriptive analyses in 196 participants concluded that there was no difference in pain and function between the groups at short or mid-term follow-up. The physical agents studied were interferential current, transcutaneous electrical nerve stimulation, ultrasound therapy, and heat/ice packs.
Corticosteroid injection versus manual therapy plus exercise
In 145 participants, descriptive analyses found very low certainty evidence for no difference in pain and function between the groups at short, mid, or long-term follow-up.
Corticosteroid injection plus anesthetic plus exercise versus Kinesio Taping plus exercise
Meta-analyzed data from 131 participants showed, on the basis of very low certainty evidence, no difference in pain and function between the interventions at short or mid-term follow-up. The data from the non-meta-analyzed study, including 39 participants, found that Kinesio Taping plus exercise was more effective for functional improvement in the short and mid-term follow-up compared with the same exercise program with additional corticosteroid injection.
Corticosteroid injection plus anesthetic versus acupuncture plus exercise
One RCT (descriptive analysis) with 99 participants concluded that there was very low certainty evidence for no difference in pain and function at short, mid, and long-term follow-up.
Corticosteroid injection plus anesthetic versus microwave diathermy
One RCT (descriptive analysis) with 92 participants had very low certainty evidence showing no difference in pain and function between the interventions at short, mid, and long-term follow-up. Except that pain at the mid-term follow-up favored the corticosteroid injection.
Corticosteroid injection plus anesthetic plus manual therapy plus exercise versus manual therapy plus exercise plus ESWT
Very low certainty evidence from 42 participants found no evidence of a difference in function at the short term in a descriptive analysis. Yet, in the mid-term follow-up, manual therapy, exercise and ESWT were more effective regarding functional improvements.
Corticosteroid injection plus anesthetic versus ESWT
One RCT with 26 participants descriptively showed, with very low certainty, that a corticosteroid injection plus anesthetic injection was more effective in pain reduction and improving function in the short term, compared with a single ESWT session.
Adverse events
Sadly, only 8 studies reported on adverse effects. The reported adverse events were luckily transient in nature and mostly associated with the needle insertion giving some pain.
Questions and thoughts
Only one of the comparisons was based on moderate certainty evidence: corticosteroid injections plus anesthetic injection plus exercise were more effective in reducing pain and improving function at 8 weeks compared to exercise alone. This effect was not retained at mid-term (26 weeks) or long-term (52 weeks). Meaning that from week 8 to 26, the exercise group achieves similar results compared to the group receiving injections on top of exercise. This may be important information for the patient to decide whether or not to opt for a corticosteroid injection for RCRSP with an additional analgesic injection. The extent of pain and the individual’s situation will be crucial in making this decision.
On the other hand, because not every study reported on the adverse effects of these injections, we should not underestimate the possibility of associated risks. The fact that some studies did not report on adverse effects does not mean that no adverse effects took place. Importantly, other types of injections beyond corticosteroid injections for RCRSP (platelet-rich plasma, non-steroidal anti-inflammatory drugs, hyaluronic acid) or corticosteroid injections at other anatomical locations than the subacromial space were excluded.
Heterogeneity in the studies should be closely analyzed in future studies. As RCRSP is an umbrella term encompassing different pain etiologies, the study subject itself can also have substantial heterogeneity, which can not be accounted for directly. RCRSP typically includes rotator cuff tendinopathy, subacromial pain syndrome, partial-thickness rotator cuff tears, and subacromial bursitis. But as symptoms overlap, this pathology is covered under the RCRSP umbrella. Despite the fact that we are confronted with poor diagnostic precision around the shoulder, the use of RCRSP to include a broad spectrum of disorders leading to similar pain characteristics, the shift from structure-specific pathologic labels can be made toward a functional and load-based manner.
How the patient’s pain is labeled can significantly influence expectations. For instance, the label impingement can negatively affect and hamper someone’s recovery due to incorrect pain beliefs. In this study we reviewed, other definitions than RCRSP were included, including impingement, which may have also led to inconsistencies in the outcomes. For example: someone who thinks the tendon is inflamed (-itis) may respond better to a corticosteroid injection than someone who knows the tendon is less tolerant of load.
The systematic review did not rely on orthopedic tests for diagnosis, because of their low reliability. However, a cluster of tests has adequate reliability since it combines the best orthopedic tests. A combination of 3 or more of 5 positive tests of the tests mentioned below is considered positive, and this is related to 75% sensitivity, 74% specificity, 2.93 positive likelihood ratio, and 0.34 negative likelihood ratio.
- Perform the Hawkins-Kennedy Test
- Perform the Neer Test
- Perform the Painful Arc Sign
- Perform the Empty Can/Jobe Test
- Perform resisted external rotation in the zero position
Partial RC tears were also eligible for inclusion, along the spectrum of rotator cuff-related pathology, but important to note is that full-thickness tears were excluded. It was, unfortunately, not exactly mentioned on which basis partial tears were differentiated from full-thickness tears. Shouldn’t we have to avoid having the corticosteroid injection for RCRSP at all, knowing that having one in case of a partial thickness tear raises the risk of a 12-week full-thickness tear? In the prospective study of Ramírez et al. (2014), 17 percent of participants with partial tears developed a full-thickness tear at 12 weeks post-corticosteroid injection. Although this was not a controlled study and thus confounding factors could have influenced the findings, putting patients at this risk seems to be carefully considered in each individual’s case instead of being routinely performed.
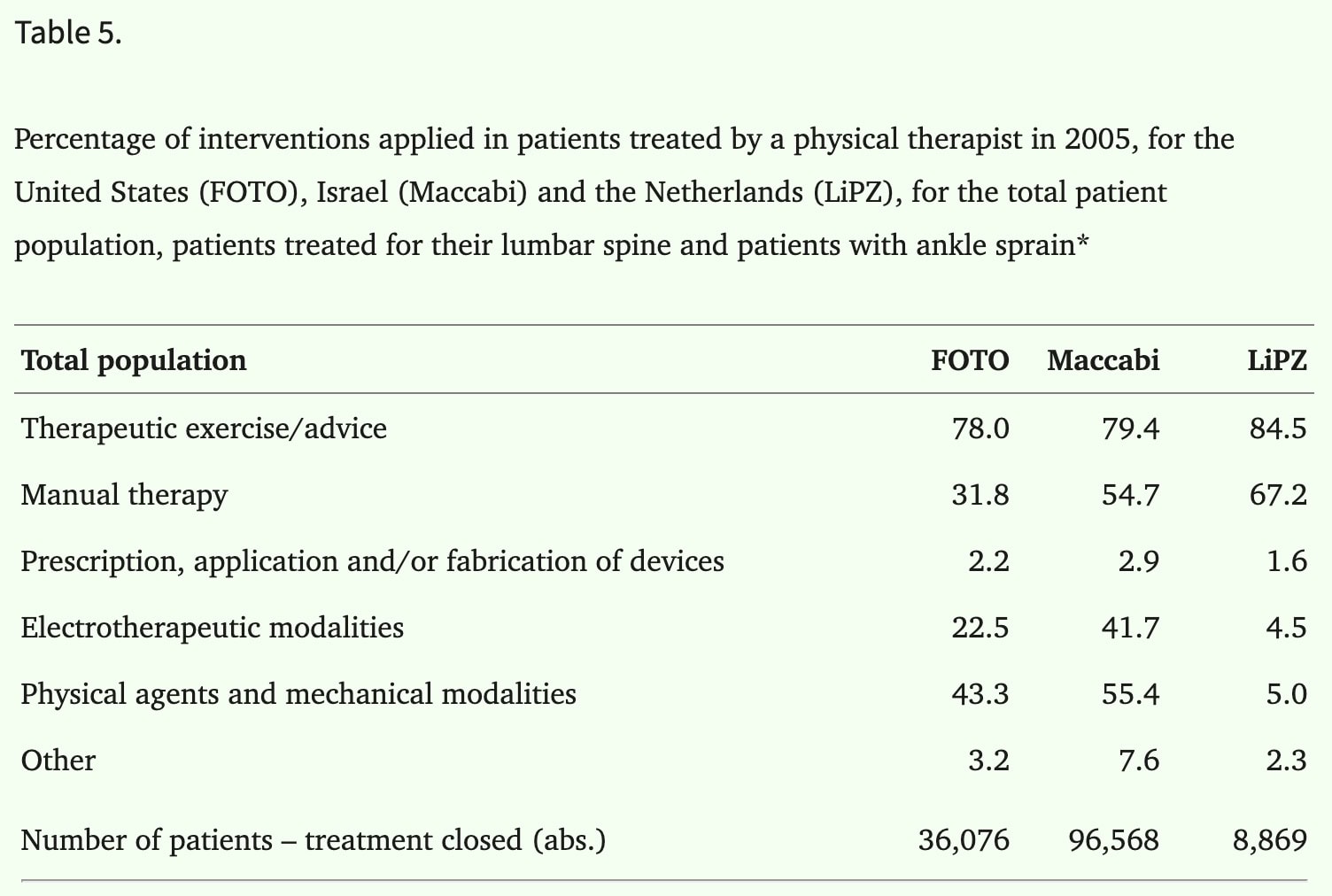
The authors chose to include a broad spectrum of physical therapy, including some forms that used physical application like heat or microwave diathermy. Apart from the fact that no difference was found in this comparison, these applications should not be considered as the focus of our profession. The use of these applications can vary widely between countries, as demonstrated by Swinkels et al. already in 2008, as can be seen in the table below. The fact that nearly half of the studies were conducted in Turkey, for example, can be regarded as a form of geographic bias. Contextual factors may be different across care settings and countries. Although the Turkey studies did account for <25% of the study population, this is something to bear in mind. It does not make the study results invalid, but generalizability can be impacted.
Talk nerdy to me
It is important to take into account that the comparison of corticosteroid injections plus anesthetic injection plus exercise versus exercise was meta-analysed based on a single study. Hence, this can not be viewed as a meta-analysis, although this was the aim of this paper. Since there was only one study, there are no results to pool, no heterogeneity to assess, and there can not be a gain in precision of the effects. The title of the article can be regarded as misleading, and those who can not access the PDF will likely mistakenly rely on the findings derived from the abstract, stating the conclusions from only one RCT (Hopewell et al. 2021). Although this RCT had the least risk of bias of all studies, the current paper summarizing this RCT should not be regarded as level 1a evidence.
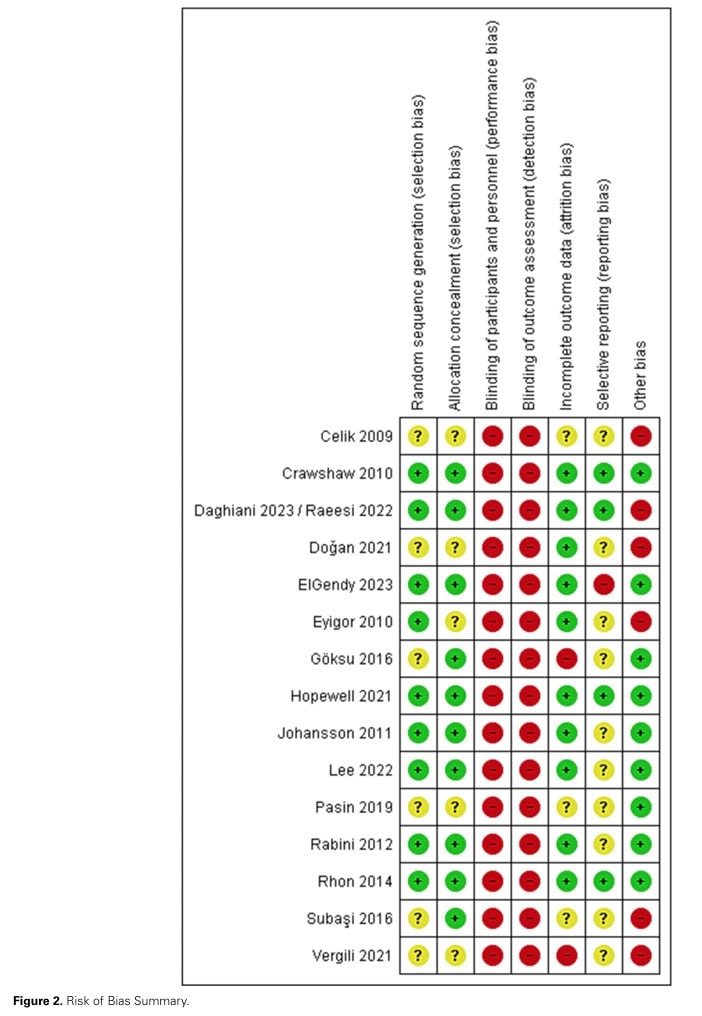
The other studies that provided data for meta-analysis were of questionable risk of bias. They included 131 participants in total, but both studies were conducted in Turkey, which may limit generalizability. The meta-analysis found no difference between corticosteroid injection plus anesthetic injection plus exercise compared to Kinesio Taping plus exercise. This evidence was rated as very low certainty. Other results are narratively described in the text, but are merely descriptive and of very low evidence.
Subgroup analyses on the influence of injection guidance based on palpation or ultrasound-guided were, although planned, not conducted because of insufficient data available. So was the case for publication bias. Because of too few studies included, no publication bias could be assessed.
About 80% of included studies measured pain, while all measured function, which is essential. Pain is highly individual and influenced by much more than the nociceptive trigger itself, if it is still present. This shift from focusing on pain to functionality can, in my opinion, give more meaning to the outcomes in general.
Take-home messages
Despite being labeled a “systematic review and meta-analysis,” this paper mostly presents narrative and single-study comparisons, with minimal pooling of data. The only conclusion based on moderate certainty is that in the short term, having an additional corticosteroid injection for RCRSP on top of physiotherapy and prescribed exercise can relieve pain and improve function, but this effect disappears in the mid and long term. However, we can be critical of the moderate-certainty evidence since no reports of adverse events were made, and this effect was based on the findings of one single study. Therefore, evidence remains scarce, and the conclusions of this article are disputable.
Reference
LEARN TO DISTINGUISH SHOULDER FACTS FROM FICTION
Awarded World Leading Shoulder Expert Filip Struyf takes you on a 5-Day Video Course to Bust Lots of Shoulder Myths that Prevent you From Delivering the Best Care for your patients with Shoulder Pain