Rotator Cuff Related Shoulder Pain | Diagnosis & Treatment

Rotator Cuff Related Shoulder Pain / Subacromial Shoulder Pain | Diagnosis & Treatment
Rotator cuff related shoulder pain (RCRSP) is a common condition that affects a large proportion of the population. It is characterized by pain and discomfort in the shoulder region, often accompanied by a limited active range of motion and inability to produce force. The etiology of RCRSP is multifactorial, with several potential contributing factors, including anatomical, mechanical, and biological factors.
There are numerous terminology options for this pathology such as subacromial shoulder pain, subacromial impingement syndrome, subacromial bursitis, and subacromial bursopathy. However, “Rotator cuff related shoulder pain” or a weak and painful shoulder are preferred and the term ‘impingement’ should be avoided (Littlewood et al., 2019).
Pathomechanism
Tendinopathy is a persistent pain and loss of function in tendons due to mechanical loading. It is most commonly seen in the rotator cuff, patellar, and Achilles tendons. The pathogenesis of rotator cuff tendinopathies is still mostly unknown and based on animal studies and surgically removed tendons. Tendinopathy is caused by collagen disruption, inflammation, or tendon cell response and the imbalance of synthesis and degradation may lead to disorganization. There is no direct relationship between structure, pain, and dysfunction, and tendinopathy can result in decreased muscle strength and control.
Tendinopathy may be driven by reduced stimulation of the tendon cell, secondary hyperalgesia, and intrinsic factors such as genetics, age, and loading history. Despite many scientific articles published on this subject, it is still challenging to construct a simple and robust model that accommodates all aspects of the condition (Scott et al. 2015).
The pain mechanisms in tendinopathy are not clear but are thought to involve local nociception mediated by changes within the tenocytes (Rio et al. 2014). The etiology of chronic tendinopathy is complex and multifactorial. The current understanding is the imbalance between the load demands placed on the tendon and its capacity to remodel (Cook et al. 2009).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
More than 80% of shoulder pain is classified as rotator cuff-related shoulder pain (Ostör et al 2005). According to the 2022 clinical guidelines, rotator cuff tendinopathy encompasses subacromial pain syndrome, rotator cuff-related shoulder pain, subacromial impingement syndrome, subacromial bursopathy, long head biceps tendinopathy, and partial thickness rotator cuff tear (Lafrance et al 2022). In this article, RCRSP is seen as an overlapping diagnosis, and synonymous with rotator cuff tendinopathy.
To classify as one of these conditions pain should be broadly over the deltoid and upper arm region. The pain will be activity-related and worse with overhead or behind-the-back reaching. Pain in the neck, reproduction of shoulder pain with neck movements, and distal neurovascular symptoms reduce suspicion. Changes in occupation and participation – rather than nature alone – might raise the index of suspicion.
When doing your clinical examination, there should be no significant loss of passive range of movement, particularly in external rotation. Familiar pain should be reproduced with resisted abduction and/or lateral rotation. Assessment of sleep, nutrition, alcohol, physical activity, and smoking should be done with the promotion of change where relevant (Littlewood et al 2019).
Orthopedic tests
Most diagnostic tests for the shoulder are unreliable or not validated and combining provides little use for clinical practice (Hegedus et al 2012). However, in the clinical practice guideline by Lafrance and colleagues, there are several recommendations — although caution is required. These are seen in the bullet points below.
Use the following tests to confirm or rule out a diagnosis of tendinopathy or full-thickness rotator cuff tear.
Combinations to confirm a diagnosis:
· Full-thickness supraspinatus tear: Jobe/Empty Can + Full Can + External Rotation Lag Sign
· Full-thickness infraspinatus tear: External Rotation Lag Sign
· Full-thickness subscapularis tear: Lift-off + Belly Press or Belly Press + Bear Hug
· Rotator cuff tendinopathy/Partial tear: Painful Arc Test
Tests to rule out a diagnosis:
· Full-thickness supraspinatus, infraspinatus, or subscapularis tear: none
· Rotator cuff tendinopathy/partial tear: painful arc test or Hawkins-Kennedy test
To perform these tests, watch the following videos closely:
Jobe test/empty can test:
Full can test:
External rotation lag sign:
Lift off test:
Belly press test:
Bear hug test:
Painful arc test:
Hawkins-Kennedy test:
Other orthopedic tests for RCRSP are:
Imaging
Medical imaging is usually not needed, except when you are suspicious of a more sinister pathology during the history taking. Outside of this exclusion use, imaging results will not change non-surgical management in RCRSP (Littlewood et al 2019).
Imaging can be useful when the patient experiences shoulder trauma, when there’s a suspicion of a full-thickness tear, or when non-surgical management isn’t going according to plan. Consider using ultrasound as opposed to MRI since it is cheaper, often quicker, and has similar diagnostic properties for tears. It is important to discuss the diagnostic values and interpretation of the imaging results with the patient (Lafrance et al 2022).
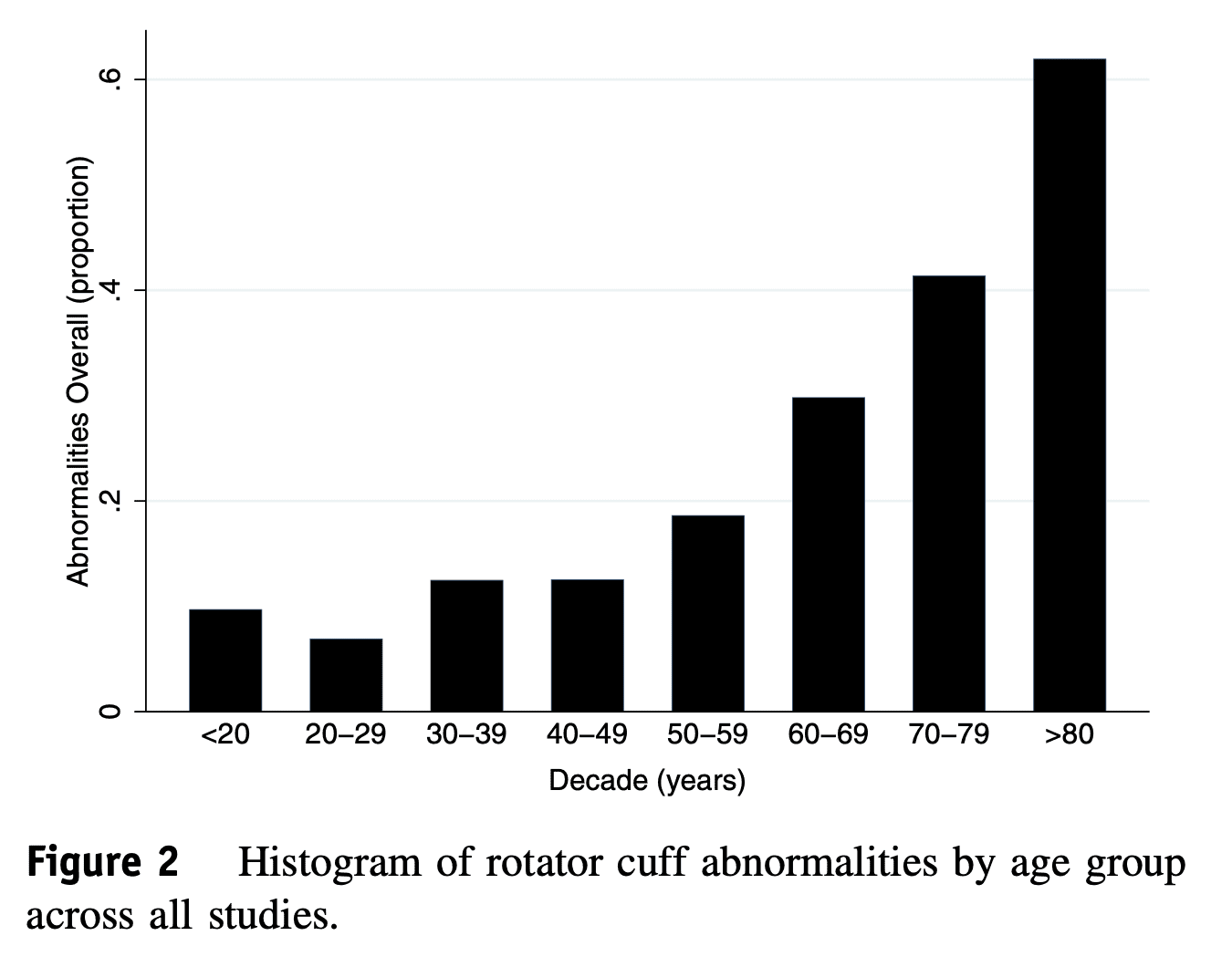
If your patient already got an MRI or ultrasound, know that ‘abnormalities’ are normal, even in asymptomatic individuals. Be aware of this when interpreting imaging results. Teunis et al (2014) investigated this. The following image gives an overview of rotator cuff abnormalities per age group.
Differential diagnoses
- Rotator cuff full-thickness tear
- Glenohumeral osteoarthritis
- AC joint pain
- Frozen shoulder
- Shoulder instability
- Parsonage-Turner syndrome
LEVEL UP YOUR ROTATOR CUFF DISORDER KNOWLEDGE – FOR FREE!

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
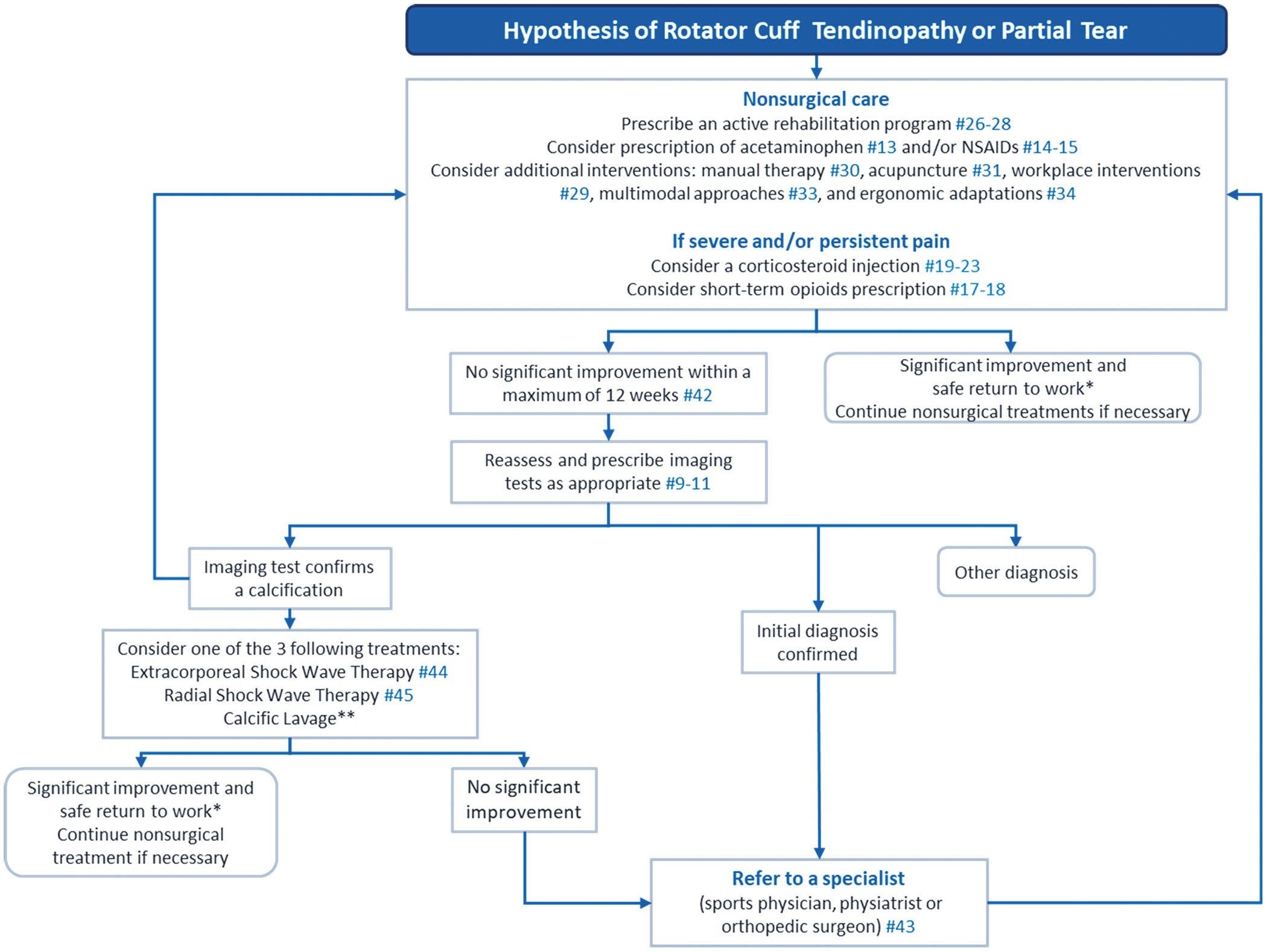
The guidelines recommend the following treatment pathway for individuals suffering with RCRSP:
Education
How can you explain what’s going on to your patients? You could tell them that there’s an issue with the muscles and tendons of the shoulder. They lack strength, capacity, tolerance, and fitness; making them complain when you lift your arm.
Medication
With medications, most recommendations are based on indirect evidence (Lafrance et al 2022), and corticosteroid injections may reduce pain in the short term but increase the risk of retearing and revision after surgery (Puzzitiello et al 2019).
Surgery
If surgery is necessary, repairing the cuff is an option. However, it is important to consider prognostic factors associated with an increased disability after surgery, such as a large tear, lower preoperative strength, low patient expectations, diabetes, obesity, and a sedentary lifestyle (Lafrance et al 2022). A Cochrane review shows high-quality evidence against the use of decompression surgery in rotator cuff disease (Karjaleinen et al 2019).
Exercise & manual therapy
There is strong evidence to suggest that exercise therapy is the way to go for RCRSP. This can be combined with manual therapy (Pieters et al 2020, Franco et al 2019). A treatment program for at least 12 weeks is suggested (Lafrance et al 2022).
Currently, the optimal dose and further specifics are unknown so further elaborations are hard to make (Lafrance et al 2022, Puzzitiello et al 2019). However, a consensus statement by Littlewood et al (2019), suggests the following:
It is essential to follow a comprehensive exercise program for at least 12 weeks for the best prognosis. The preferred treatment for rotator cuff injuries is loading through progressive exercise, including the kinetic chain, and working to fatigue with an acceptable symptom response. Exercising on alternate days is sufficient, and heavy loading or plyometrics may require two to three sessions per week. Three exercises are usually enough and should address personal functional limitations. While exercises can provoke pain, they should be continued as long as symptoms settle sufficiently.
Shockwave (ESWT)
If an ultrasound or MRI confirms calcification of the rotator cuff tendons and the patient remains refractory to initial nonsurgical management, shockwave or an arthroscopic lavage can be considered (Lafrance et al 2022). However, a Cochrane systematic review contradicts the shockwave statement (Surace et al 2020) and the lavage is supported by low-quality evidence (Lafrance et al 2019).
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Shoulder Expert Separates Fact from Fiction in All-Encompassing Online Course

What customers have to say about this course
- Tineke De Vries26/01/25Goede cursus. Goede cursus, gericht op de praktijk Veel geleerd. Met name wat betreft de opbouw van de oefeningenDempsey Thiele02/01/25Overzichtelijk en praktisch! Ik heb de cursus met plezier afgemaakt. Ik denk dat dit een relevante cursus is voor iedere fysiotherapeut die meer inzicht wil krijgen over de huidige evidence omtrent schouder rehabilitatie. Alle informatie wordt overzichtelijk aangeboden.
Ik kan weer kritisch aan de slag mijn patiënten te helpen in de toekomst! - Carlijn Duursma27/12/24Goede cursus Veel verdieping. duidelijke uitleg. misschien wat tekeningen toevoegen voor extra verduidelijking. Veel geleerd.Vanessa Burnet22/12/24Leerzame cursus Opfrissing van kennis wat is weg gezakt.
- Paul Mensink15/12/24Paul Mensink High level literature composed course, videos are perfect examples for used techniques and exercisesFrank Kleyn12/12/24CRSP Ik kan bovengenoemde cursus zeer aanbevelen , nieuwste inzichten , zin en onzin van Subacromiale ruimte , de duidelijke vertaling naar de praktijk en de behandeltafel .
- Marty26/11/24RCRSP CURSUS Niet heel veel nieuws maar wel een goed overzicht en duidelijke uitleg over biomechanica.
Goede filmpjes van Filip en technieken ook goed uitgelegd.
Goede toetsen die de lesstof vrij compleet behandeld..
Website werkt naar mijn mening niet goed. Nogal onoverzichtelijk…
Vergt wat tijd om er mee om te gaan maar voordeel van de cursus is de gunstige prijs per accreditatie punt. Netjes.maria Kramer01/11/24goede cursus voor rcrsp Goede cursus met veel praktische vaardigheden en oefeningen die je direct kunt toepassen, aanrader. - Erik Versluis13/08/24Rotator Cuff Related Shoulder Pain RCRSP by Filip Struijf
State of the art course and very useful for physiotherapists with shoulder expertise or who want to further develop their skills in research and treatment of patients with shoulder complaints. A nice addition is a shoulder case in which you can process the knowledge you have recently acquired.
A major advantage is the possibility to read the course material offered and to watch the video material again.Birgit Schmitz28/04/24Rotator Cuff Related Shoulder Pain RCRSP
Ik vond het een waardevolle cursus met onderbouwd wetenscahppelijk onderzoek dat ondersteunt in mijn praktisch handelen. Ik heb al een nieuwe cursus uitgezocht. 🙂 - Thijs de Jager22/04/24Rotator Cuff Related Shoulder Pain GOEDE RCRSP CURSUS.
Over het algemeen een goede cursus waarbij ik veel ben opgestoken. Goede, evidence based informatie met hier een daar wat uitleg video’s die zeker helpvol waren. Het is ook fijn dat je onder de cursusonderdelen vragen kan stellen en hier een antwoord op kan verwachten van Filip zelf. 4 sterren i.p.v. 5 sterren omdat ik graag meer duidelijkheid en uitleg in video format over de oefeningen had willen zien. Er worden een hoop oefeningen getoond maar het is aan de cursist zelf om te bedenken welke in te zetten in de praktijk.Larson de Neve16/04/24Rotator Cuff Related Shoulder Pain GOOD COURSE
Good theoretical and practical course with exercises that you can immediately use in practice. - Beppeke Molenaar13/04/24Rotator Cuff Related Shoulder Pain OVERALL A GREAT COURSE
This is a very informative and comprehensive course.
Some of the quiz answers that are correct are counted as incorrect, which is a pity.
(Comment Physiotutors: We are currently doing an overhaul of our quizzing system and have fixed this issue now.)Willem Zee28/01/24Rotator Cuff Related Shoulder Pain PRIMA CURSUS!
goed te doen, uiterst praktisch - Jason Pearson11/01/24Rotator Cuff Related Shoulder Pain RCRSP COURSE
Very satisfied with this course. Provides a great framework with which to build your assessment and rehabilitation strategiesMichal Wajdeczko09/01/24Rotator Cuff Related Shoulder Pain Ik ben super blij ermee.
Het was een zeer interessante training. Het cursus was rijk met ge-update informatie, alles wordt volledig en transparant uitgelegd. Ik moet ook toevoegen dat deel van nuttige sets oefeningen briljant is! Veel nuttige tips en combinaties om rotator cuff pijn te kunnen verminderen en alle spieren efficiënt te trainen. Ik ben er trots op dat ik weer mijn kennis en competenties kon ontwikkelen en om mijn patiënten een professionele benadering van schoudercomplexe aandoeningen te kunnen bieden.
Super bedankt!! - Ante Houben30/12/23Rotator Cuff Related Shoulder Pain RCRSP
This course is well designed and based on solid evidence. The information is presented in a structured manner, using text, images and videos to enhance understanding. In addition, I appreciated the course’s emphasis on effectively conveying this information to patients. However, I wished the exercise therapy was more extensive.
Naomi Tiller20/12/23Rotator Cuff Related Shoulder Pain RCRSP COURSE
Fantastic course that’s easy to follow, up to date and evidence based. I’ve immediately been able to implement what I’ve learnt in to my own work which has given me a lot more confidence as well as made it more enjoyable! A good refreshed for me on how the rotator cuff works, a better understanding of how to treat these problems and better communicate with my patients as well as exercise inspiration (always appreciated!). Overall very happy to have done this course!
Super bedankt!! - Stijn de Loof17/12/23Rotator Cuff Related Shoulder Pain GOOD THEORY, LESS EXERCESIS
I liked the theoretical part of the course. A good refresher about the shoulder and rotator cuff with new insights
I was a bit disappointed in the part ‘exercises’. They were super basic and without explinations.Mehdi Benkirane24/11/23Rotator Cuff Related Shoulder Pain REVIEW
Très bon cours, je le recommande pour se remettre à jour sur les tendinopathies de l’épaule.




