Clinical Pearls and Advice From a Young PT to Even Younger PTs
I must have read a lot of different blog posts as a newly graduate, but certainly one of the greatest was Jarod Hall’s “Clinical Pearls and advice from a young PT to even younger PTs”.
Can’t agree enough on most of the points! My number one advice would also be to learn as much as possible as fast as possible about pain!
Here’s Jarod in 2015(!):
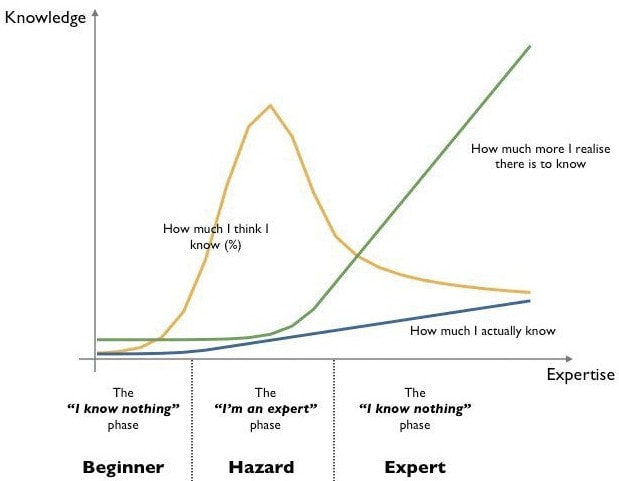
Having been out of school just shy of 2 years it might be hard to believe I have the ego to write a post giving advice to anyone or educating on clinical pearls. Maybe it’s my naivety or just an embodiment of the wonderful illustration that depicts the relationship between how much you think you know and how much you actually know.
However, I truly feel that I have been lucky enough to be plugged into and learn from some extremely smart clinicians (whether they realize I have been learning from them or not). One of my professors in PT school always said that there was an immense learning curve during your first year of clinical practice. I would have to say that it was an indescribable understatement of my own personal growth as a healthcare provider. The following is a shortlist of information I wish I knew/understood when I started practicing, and that I’ve had to learn the hard way.
- Learn AS MUCH AS YOU CAN about pain science and the biopsychosocial model AS FAST AS YOU CAN!
- Listen closely and carefully to your patient and they might just tell you exactly what is wrong and even how to fix it. Stop thinking about every test you should do and every movement you should evaluate while the patient is telling you their story. Earnestly listen to them because you are often the first person that has. 80-90% of your diagnosis comes from the history you take.
- STOP cranking on and cramming your patient’s total knee replacement right after surgery. They certainly aren’t limited in ROM due to massive amounts of scar tissue a few weeks after surgery. They are in pain and have muscle guarding as well as fluid in the knee restricting movement. Honey will catch the fly in this case. Try gentle ROM, Contract relax, grade 1-2 joint mobs (not 3-4), and light IASTM to the quads. If their knee really is burdened with scar tissue doesn’t it make more sense to have them exercise and move anyway? They can most likely put a lot more force through their knee into new ROMs than you can with your hands.
- Stop basing everything you do and the way you think on a patient’s x-ray or MRI. We now know and have a plethora of evidence that tissue damage often does not correlate to pain presentation. Imaging is important, but we need to talk patients off of the I have DDD/DJD cliff and onto you don’t have to be in pain because of your imaging ride.
- Use manual therapy and modalities if you must, as a means to get a patient to do MORE active therapy, not become passive and falsely reliant on your magic sound wand or massage.
- Do not be afraid to question your instructors. In school or on clinical affiliations. They can be wrong, and you may have something to teach no matter how high their position.
- Learn about the tissue homeostasis model and think about it during your treatments. A vast amount of the patients we treat in the outpatient patient setting have overuse injuries that have led to degenerative tissue pathology. To truly “heal” these patients we need to know how to appropriately load their tissues to stimulate healing. Learn the “sloptimal zone of loading”
- This bullet goes along with number 6. Learn to use isometrics! They can be very powerful for pain relief, improving motor unit recruitment, and loading tendons to stimulate collagen synthesis.
- Stop overcomplicating evaluation and treatment. With a doctoral education, I know there can be pressure to “find” all sorts of asymmetries that need correcting and give patients fancy Bosu body blade exercises to demonstrate some sort of face validity, intelligence, and value. Yet, the vast majority of those asymmetries, leg length discrepancies (if you are even able to get close to accurately diagnosing them), forward head rounded shoulder postures, increased lumbar lordosis, etc rarely actually have anything to do with your patient’s pain. Very often your patients sit in prolonged positions and don’t move/exercise much at all through the day. Merely getting them moving in a safe and progressive manner can be incredibly powerful.
- No, everyone doesn’t have a rotated pelvis and please stop correcting all of the theoretical innominate torsions. The end.
- Learn and become skilled in some basic manipulation techniques. I know many people may disagree with this, and yes I know the research surrounding manipulation techniques and their questionable benefit over other manual therapy treatments very well. However, the fact still remains that many of the patients that walk through your door will have had a manipulation done on them before. They likely even experienced resolution of a painful condition. It doesn’t matter if the technique fixed them or not if they THINK it fixed them. There is power in using a technique that a patient strongly believes will help. Not to mention there is increased theatrical placebo with audible joint pops. Just make sure you explain to the patient that you are NOT putting anything back into place and that the benefits of the treatment are likely due to global or possibly local neurophysiologic effects.
- Give patients small manageable home exercise programs that require very little if any equipment. A skilled therapist can make exercise easy and convenient for a patient, because we all know there is no way they will do it if it has 10 exercises, takes an hour, and they need dumbbells, swiss balls, therabands, and foam rollers. Not to mention if they are doing that much at home with good form and independently why in the world do they need to see you?
- Learn to use repeated motions as a way to decrease nervous system sensitivity/threat perception, decrease pain, and improve ROM for additional exercises.
- Stop chasing fads! They come and they go all in good time. Learn how to critically think and use evidence to guide your clinical decision-making.
- Remember that there are 3 pillars of evidence-based practice. Patient expectation, research/evidence, and clinical experience. They are all important, but you have to remember that evidence should dictate changes to your practice even if it goes against your personal experience as it is very easy to have a cognitive bias and overlook the shortcomings of your previous methods.
- GET ON SOCIAL MEDIA!!!! And I don’t mean to post funny cat pictures or follow Lady Gaga. Get on social media and follow the plethora of intelligent people out there regularly posting evidence-based blogs, posting research ahead of print, and engaging in clinical discussions that can convey years and years of knowledge and experience……ok well you can post some cat pictures as long as they’re funny.
I know you and the cat are probably thinking along the same lines, but thank you for taking the time to read this far. This is a shortlist and will definitely be expanded on many times over. Just remember to stay hungry for self-improvement. It helps you, your patients, and our profession.
Jarod Hall, PT, DPT, CSCS

Jarod Hall
Jarod Hall, PT, DPT, OCS, CSCS
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.







