Thoracic Outlet Syndrome | Diagnosis & Treatment for Physios
Thoracic Outlet Syndrome | Diagnosis & Treatment for Physios
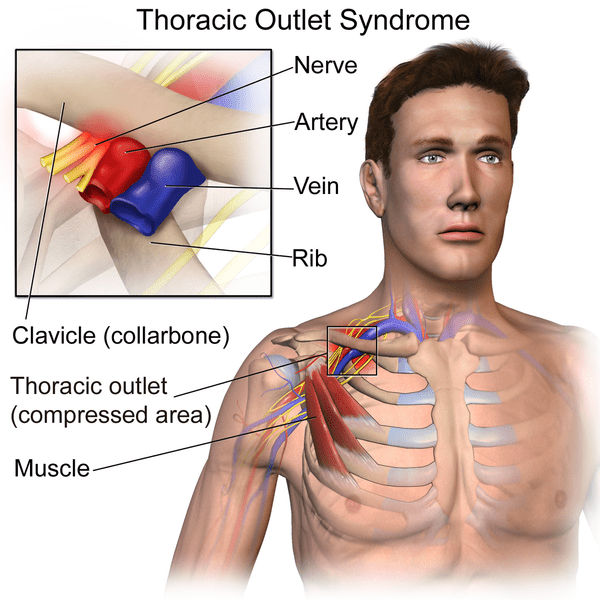
The term “Thoracic outlet syndrome” (TOS) was originally coined by Peet in 1956 and has emerged as one of the most controversial topics in musculoskeletal medicine and rehabilitation (Hooper et al. (2010). Thoracic outlet syndrome is defined as the compression of nerves or blood vessels near the base of the neck. Specifically, the compression of the brachial neural plexus, subclavian artery, subclavian vein, or any combination of these vessels may occur (Levine et al. 2018). The pain and discomfort of TOS are generally attributed to the compression of the subclavian vein, subclavian artery, and the lower trunk of the brachial plexus as they pass through the thoracic outlet (Watson et al. 2009).
The following video will give you an overview of the different forms of TOS as well as the pathophysiology behind it:
While the distinction between tnTOS and sTOS was common in the past, Illig et al. (2016) of the Society for Vascular Surgery published reporting standards for TOS and mention that the terms “true, disputed, or nonspecific nTOS” should be avoided as the difference between “true” and “disputed/nonspecific” TOS is only based on objective symptoms observed in nerve conduction abnormalities or hand muscle atrophy. Furthermore, the term vascular TOS should be avoided as well as this term offers insufficient detail by which to characterize patients with either venous TOS (vTOS) or arterial TOS (aTOS).
Epidemiology
Thoracic Outlet Syndrome is typically diagnosed in early adulthood (ages 20-40) and is more prevalent in those with the shoulder flexed for the majority of the work day, have repeated trauma to the shoulder joint, and those who exhibit abnormal posture, including positions required to play bow instruments (Levine et al. 2018).
The most commonly presented cause of TOS is thought to be whiplash motion which can result in instability at the atlantoaxial joint, causing the surrounding musculature (like the sternocleidomastoid and scalenes) to shorten, in order to compensate for the laxity in the joint.
The incidence of TOS is reported to be approximately 8% of the population and the female-to-male ratio is estimated between 2:1 to 4:1, while Urschel et al. (2008) report that vascular TOS is more equal between non-athletic men and women, but found to be even greater in competitive athletic men vs women (Melby et al. 2008). 98% of all patients with TOS fall into the neurogenic TOS (nTOS) category and only 2% have vascular TOS. While neurological symptoms appear more prominently, the majority of these cannot be evaluated objectively by nerve conduction abnormalities or atrophy and would thus fall within the formerly called “symptomatic or disputed” TOS classification (Davidovic et al. 2003).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
It is essential that the clinician carefully considers and at least attempts to clinically differentiate, where possible, exactly which component of the neurovascular complex is being affected and precisely where it is being compressed. This will dictate not only which further investigations are required, but may well impact on what is the most appropriate treatment strategy. In reality, this is often easier said than done (Watson et al. 2009). Unfortunately, there is no test or investigation that is able to consistently prove the diagnosis of TOS.
The following table is a modern adaption of Hooper et al. (2010) and presents an overview of the presentation of venous, arterial, and neurological TOS:
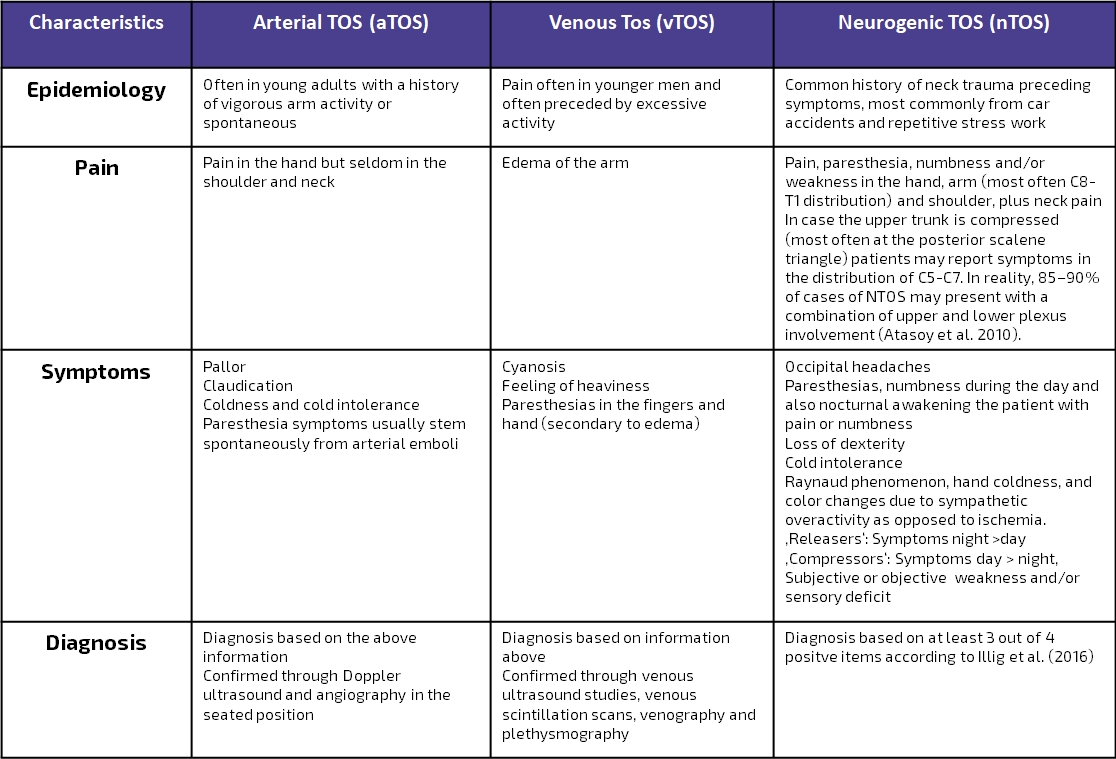
Due to the confusion around a clear definition of nTOS, Illig et al. (2016) of the Society for Vascular Surgery published reporting standards for TOS with the primary aim to provide a clear and consistent understanding and definition of what constitutes a diagnosis of nTOS. Watch the video below, to learn more about the consensus criteria:
Examination
In the following, we will explain how to use physical examination to confirm or reject the 3 criteria that you may have found during patient-history taking following the suggestions from Illig et al. (2016). The fourth criterion – a test injection – is outside of the scope and not feasible for a physiotherapist. The diagnosis of nTOS is confirmed if all 3 remaining items are positive:
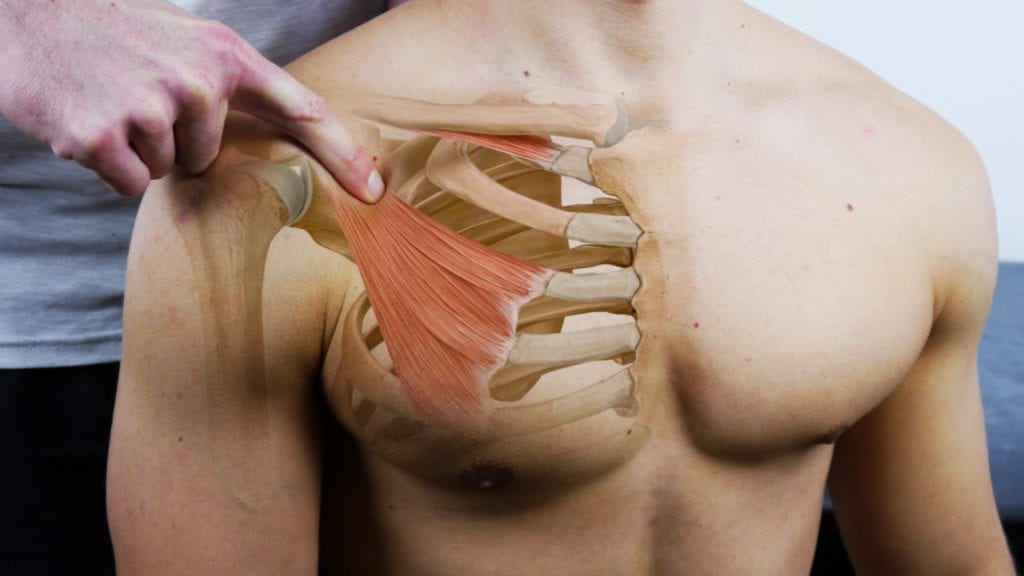
1) Local findings can be confirmed by tenderness upon palpation of the scalene triangle and pectoralis minor insertion.

2) Positive Peripheral Findings
Upper limb tension testing is sensitive for irritation of the neural tissue including cervical roots, brachial plexus, and peripheral nerves as well as for patients with arm pain syndrome. It has been advocated for the diagnosis of neurogenic TOS with reported high sensitivity. The test appears to be excellent for screening for sensitization of the neural tissue in the cervical spine, brachial plexus and upper limb but is not specific for one area. The test is recommended as part of the examination and for its usefulness in treatment that includes neural mobilization (Hooper et al. 2010).
There are several provocation tests for TOS that are designed to stress one of the 3 possible intervals for entrapment. These are:
- Roos / Elevated Arm Stress Test (All 3 intervals)
- Cyriax Release Test (All 3 intervals)
- Adson Test (Posterior Scalene Triangle)
- Eden Test (Costoclavicular Space
- Wright’s Test in 180°(Costoclavicular Space)
- Wright’s Test in 90° (Retropectoralis minor space)
3) Absence of other likely diagnoses
The physical examination of TOS is frequently long and complex as the clinician needs to examine the entire upper limb and cervical spine. Not only is a neurological examination required, but frequent peripheral nerve entrapment tests also need to be performed. In a substantial number of patients initially diagnosed with TOS, either radiculopathy or neuropathy is the eventual diagnosis. In more than 60% of patients referred to vascular surgeons for a TOS surgery, an alternate diagnosis was established (McGillicuddy et al. 2004). So the diagnosis of TOS should be only considered after the exclusion of cervical radicular syndrome and peripheral neuropathy. If you are unsure how to diagnose cervical radicular syndrome and how to distinguish it from peripheral nerve entrapment, we’d like to refer you to the chapter on cervical radicular syndrome.
There are many causes of similar pain symptoms, including rotator cuff tears, subacromial bursitis, adhesive capsulitis (so-called frozen shoulder), glenohumeral impingement syndromes, and lateral epicondylitis (tennis elbow). None of these, however, will manifest neurological abnormalities. Thus, a neurological evaluation will narrow this diagnosis to radiculopathy, neuropathy, or TOS (McGillicuddy et al. 2004). In the following video we will explain which characteristics distinguish TOS from similar diagnoses like cervical radicular syndrome of C6-8 and median or ulnar neuropathy:
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
If an individual is diagnosed with arterial or venous TOS, surgery is typically the only option due to the severity of the injury (Aligne et al. 1992). A systematic review and meta-analysis by Peek et al. (2017) showed that surgical treatment of TOS seems to be beneficial in most patients and is relatively safe.
The largest challenge remains the diagnosis of TOS, especially neurogenic TOS. This is one of the reasons why exercise should therefore be the first option in treating true neurogenic and symptomatic TOS. Lo et al. (2011) conducted a systematic review of the effectiveness of physical treatment for TOS. Although there is no firm evidence in the form of controlled studies, most of the reviewed articles show that conservative treatment is able to decrease pain in TOS. The authors also recommend that treatment should be maintained for at least 6 months to ensure sufficient effects.
Treatment should be focused on the positive findings during your examination. A common feature exhibited by individuals with TOS is a flexed head position, depressed and anteriorly shifted shoulder, and protracted scapula (Laulan et al. 2011). This abnormal shoulder position, combined with 90° of abduction or flexion (as is commonly observed with those whose occupations require reaching, especially overhead, and repeated loading), could lead to a decrease in the costoclavicular space, increased friction of the neurovascular bundle in the subpectoral bundle, and a shortening of the sternocleidomastoid. Resistance exercises can be performed with either resistance bands or dumbbells, and with the goal of achieving muscular endurance (i.e., low weight and a high number of repetitions). However, strengthening exercises alone will not alter the pathophysiology of TOS; a combination of strengthening, stretching, and postural adjustments must all be incorporated for improvements to be observed Watson et al. (2010).
The shortened sternocleidomastoid may cause the scalenes and pectoralis muscle groups to shorten, leading to improper head and neck alignment and postural dysfunction (Vanti et al. 2007). The following stretching exercises can be performed in order to decompress the thoracic outlet in the posterior scalene triangle, costoclavicular space and subcoracoid tunnel:
As contributing factors to TOS are multifactorial, addressing all treatment options is beyond the scope of this wiki. If you like this post and you would like to learn how to treat TOS in detail, check out our Orthopedic Physiotherapy of the Spine course.
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Finally! How to Master Treating Spinal Conditions in Just 40 Hours Without Spending Years of Your Life and Thousands of Euros - Guaranteed!

What customers have to say about this course
- Shachaf Alexander19/07/24Orthopedic Physiotherapy of the Spine Orthopedic Physiotherapy of the spine
Interesting course packed with useful data and practical tools.
I highly recommend.Verena Fric25/11/22Orthopedic Physiotherapy of the Spine GREAT COURSE ABOUT THE SPINE
great course, best overview about the different syndromes of the spine, very helpful and relevant for the work with patients - Peter Walsh01/09/22Orthopedic Physiotherapy of the Spine 5 starsChristoph21/12/21Orthopedic Physiotherapy of the Spine Really a well done course, using the modern ways of teaching. Compliments! Sometimes for me you entered too much into details instead of touching more important chapters of Spine treatment like techniques for the treatment of muscles and fascias
- John09/10/21Orthopedic Physiotherapy of the Spine EXCELLENT COURSE HIGHLY RECOMMEND
As a newly graduated physiotherapist i highly recommend this course just to know you are on the right track with your patients. the information presented is very clear and easy to follow as well as the great physiotherapy style videos. It makes learning actually fun , thanks guys for all your hard work. Well deserved.Alexander Bender06/09/21Orthopedic Physiotherapy of the Spine During the corona crisis, I booked many online courses and webinars, but none were as entertaining and well thought out as PhysioTutors’ courses.
All units are well summarized, meaningfully broken down and easy to understand.
I am looking forward to the other courses.
Many greetings from Germany. - GHADEER05/01/21Orthopedic Physiotherapy of the Spine VERY INFORMATIVE AND UPDATED
for anyone who is lost in handling spine cases, this course is very helpful.MICHAEL PROESMANS20/12/20Orthopedic Physiotherapy of the Spine HIGHLY METHODICAL, WITH PLENTY OF SCIENTIFIC REFERENCE
Clear, structured and well researched course concerning most common pathologies of the spinal complex.
Plenty of informative modules, with detailed video-analysis.
If you’re looking for a course to study in your own time, with enough depth and scientific background, then you’ve found a very good one here.
Bang for buck, a great course. - BENOIT08/05/20Orthopedic Physiotherapy of the Spine After finishing the Orthopedic course for Lower & Upper limbs, I was looking forward to begin this Spine specific course.
Really good overview about all spine pathologies from epidemiology to diagnosis & treatment which made me more confident to care for my future patients.
ANOTHER GREAT COURSE !
The courses are well detailed with lot of informations and videos.
For me these 2 courses are must to see to learn and update knowledge for most common pathologies in Physiotherapy.Nicolas Cardon27/04/20Orthopedic Physiotherapy of the Spine This is a very interesting course !
We can find many informations about the main pathologies and their differential diagnosis and about objective and subjective exam. Videos are clear and well designed.
It’s a very well course for these who wish complete their Orthopedic Manual Therapy curriculum.
A French Physio’







