Patellar Tendinopathy / Jumper's Knee | Diagnosis & Treatment

Patellar Tendinopathy / Jumper’s Knee | Diagnosis & Treatment
Introduction & Epidemiology
 Patellar tendinopathy is one of the most common sources of anterior knee pain and is most prevalent in young jumping men between 15 and 30 years of age. Paradoxically, the athletes who can jump the highest and run the fastest are the ones who are at the highest risk to suffer from patellar tendinopathy. According to Cook et al. (1997) one-third of athletes suffering from it were unable to return to sport within 6 months and an astonishing 53% with patellar tendinopathy were even forced to retire from sport.
Patellar tendinopathy is one of the most common sources of anterior knee pain and is most prevalent in young jumping men between 15 and 30 years of age. Paradoxically, the athletes who can jump the highest and run the fastest are the ones who are at the highest risk to suffer from patellar tendinopathy. According to Cook et al. (1997) one-third of athletes suffering from it were unable to return to sport within 6 months and an astonishing 53% with patellar tendinopathy were even forced to retire from sport.
The tendinopathy develops as a continuum where normal (in case of unloaded knees) or excess loads (in case of loaded knees) may induce reactive tendinopathy which initiates tendon disrepair and degeneration. Repetitive loading with insufficient rest may also induce pathology. The tendon’s mechanical properties change, with increases in tenocytes and ground substance and this leads to swelling, matrix degradation, and neovascular ingrowth, making the tendon vulnerable.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
If you watch our YouTube video regularly, then you might have watched our video on 6 tips to diagnose lower limb tendinopathy. They were:
- Epidemiological data (see above)
- Highly localized pain at the tendon enthesis
- Muscle wasting
- Hallmark signs
- Pain onset 24 hours after high+fast load activities
- A proportional load-pain relationship.
In this section, we will specify those 6 points for the patellar tendon and look at possible differential diagnoses
Localized pain:
While patellar tendinopathy can occur at the inferior pole of the patella, it can also occur at the insertion of the tendon at the tibial tuberosity which is rarer. If a patient reports pain at the base of the patella, you might suspect quadriceps tendinopathy.
A useful test to confirm patellar tendinopathy is the Royal London hospital test, which has a good sensitivity of 88% and a specificity of 98% to differentiate patients with patellar tendinopathy from other sources of anterior knee pain.
To perform the test, palpate the patellar tendon for tenderness from proximal to distal with the knee in full extension. Then palpate the tender spot again in 90 degrees of knee flexion. The test is positive if the pain in the flexed position is less or absent.
In this position, you can also directly perform Hoffa’s test to see if the fat pad is involved or not. The procedure for it is pretty much the same as for the Royal London hospital test only that you start in the flexed position and that you now palpate the infrapatellar fat pad for tenderness left and right of the patellar tendon. Then you palpate again with the knee straight. This test is also positive if the pain in the extended position is greater than in the flexed position.
Note that fat pad irritation usually presents with more diffuse pain and is usually aggravated by an overextension of the knee. In young athletes at the start of puberty, you’ll have to keep growth plate pathologies in the back of your mind: The most common one is Osgood-Schlatter disease, an overuse injury characterized by ossification of bone along the growth plate at the tibial tubercle. In the most severe version, Osgood Schlatter might result in an unfused tibial tuberosity growth plate. Sinding Larsen Johannson is the equivalent of Osgood Schlatter, only that now the apex of the patella is affected.
A very common differential diagnosis, namely patellofemoral pain presents with diffuse knee pain and is more prevalent in young women with marked knee valgus during squatting. If you’re doubting, applying a rigid tape with the McConnell technique to reduce patellar compression and lateralization can confirm PFPS in case the tape has a positive effect. At last, diffuse pain deep to the quadriceps tendon might be due to irritation of the suprapatellar fat pad and painful clicking might indicate suprapatellar plica syndrome. Both conditions can only be confirmed with imaging.
Muscle wasting:
To examine muscle wasting, observe the quads and calves for muscle bulk and differences and palpate them for tone, which is often reduced if patients have not been using them much.
Hallmark sign
The hallmark sign of patellar tendinopathy is pain when sitting with a bent knee like when sitting in the car for a prolonged time. Like with other tendinopathies of the lower limb, patellar tendinopathy presents with typical warm-up pain, so after a patient has warmed up, the pain gets less.
Pain onset or exacerbation 24 hours after high+fast load activities
In the case of the patellar tendon, you have to specifically ask for an increase in volume, intensity, or frequency of jumping that has led to the onset of symptoms. This is often the case after a prolonged break as well. And secondly, the pain is usually increased 24 hours after those high and fast load activities, so after an excessive jumping session.
Proportional load-pain relationship
Like with every tendinopathy you are looking for an increase in pain with an increase in load on the patellar tendon. A good starting provocation test can be decline squats in which very load-intolerant patients report pain from as early as 30 degrees of flexion. Then continue with double-leg hopping, single-leg hops, maximal hops, and maximal forward hops for distance. A very intense test is asking a patient to come to a sudden stop on one leg after jogging on running as if they were to change directions. Pain levels have to increase with increasing difficulty, so if the decline squat was scored with a 3 out of 10, single leg hopping should be higher with the highest scores at maximal hopping or a sudden stop from running.
Another common orthopedic test for patellar tendinopathy is Patellar Tendon Palpation.
WHAT TO LOOK FOR TO PREVENT HAMSTRING, CALF & QUADRICEPS INJURIES

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Traditionally, eccentric exercise has been recommended in the rehab of tendinopathies. However, a study by Kongsgaard et al. (2009) found equal results in terms of disability and pain after 12 weeks when they compared a group performing an eccentric decline squat program to a heavy slow resistance program in patients with patellar tendinopathy. Interestingly, only the heavy slow resistance group demonstrated pathology improvement and increased collagen turnover, and more importantly, 70% of all participants of the group were satisfied with their program at 6 months compared to 22% in the eccentric group.
The findings are confirmed by a systematic review from Malliaras et al. (2013) who found that heavy-slow loading for the patellar tendon had an equivalent or higher level of evidence than isolated eccentric loading.
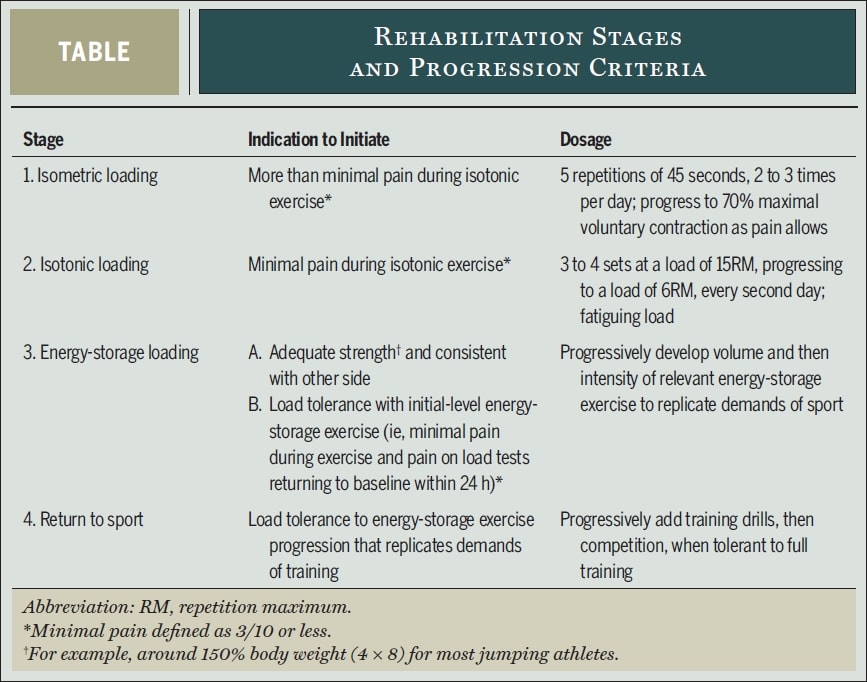
So how could such a heavy-slow resistance program look like? Tendinopathy top researchers Peter Malliaras, Jill Cook, Craig Purdam and Ebonie Rio propose the following evidence-based 4 –stage rehabilitation protocol in their paper from 2015:
First of all loading modification of high-load energy storage activities that aggravate the pain should be used. In the case of athletes in mid-season volume and frequency of those activities should be reduced in consultation with the athlete and coach. Some pain was deemed acceptable during and after the exercises, but symptoms should have settled within 24 hours post. In their paper, Malliaras used one repetition of single-leg decline squat to 90 degrees of knee flexion or maximum angle allowed by pain as a pain-provocation test to determine load tolerance on a daily basis. If the pain score on the load test has returned to baseline within 24 hours of the activity or rehabilitation session, the load has been tolerated. If the pain is worse, load tolerance has been exceeded.
Let’s have a closer look at each rehabilitation stage:
Stage 1 – Pain reduction: Isometric loading
- 5 repetitions of 45s isometric mid-range (30-60° of knee flexion) single leg quadriceps exercise at 70% of MVIC 2-3x/day.
- Resistance should be increased as quickly as tolerated.
- Spanish squat
- Address other strength deficits along the kinetic chain
Rio et al. (2015) started a bit of a trend when they conducted a cross-over trial on 6 volleyball players with patellar tendinopathy. Their results were astonishing with all players experiencing an immediate decrease in pain from an average of 7/10 on the NRS to 0 with only one of the 6 reporting a remaining pain of 1– for at least 45 minutes after the isometric contractions. The protocol they used was 5 sets with 45 seconds contraction in a leg extension machine and an effort of 70% of the maximal voluntary effort. They also found that isometrics were able to decrease cortical inhibition and increase strength by 19%. They compared the isometric intervention with an isotonic intervention and the effects seen in the isometric group could not be achieved in the isotonic group:
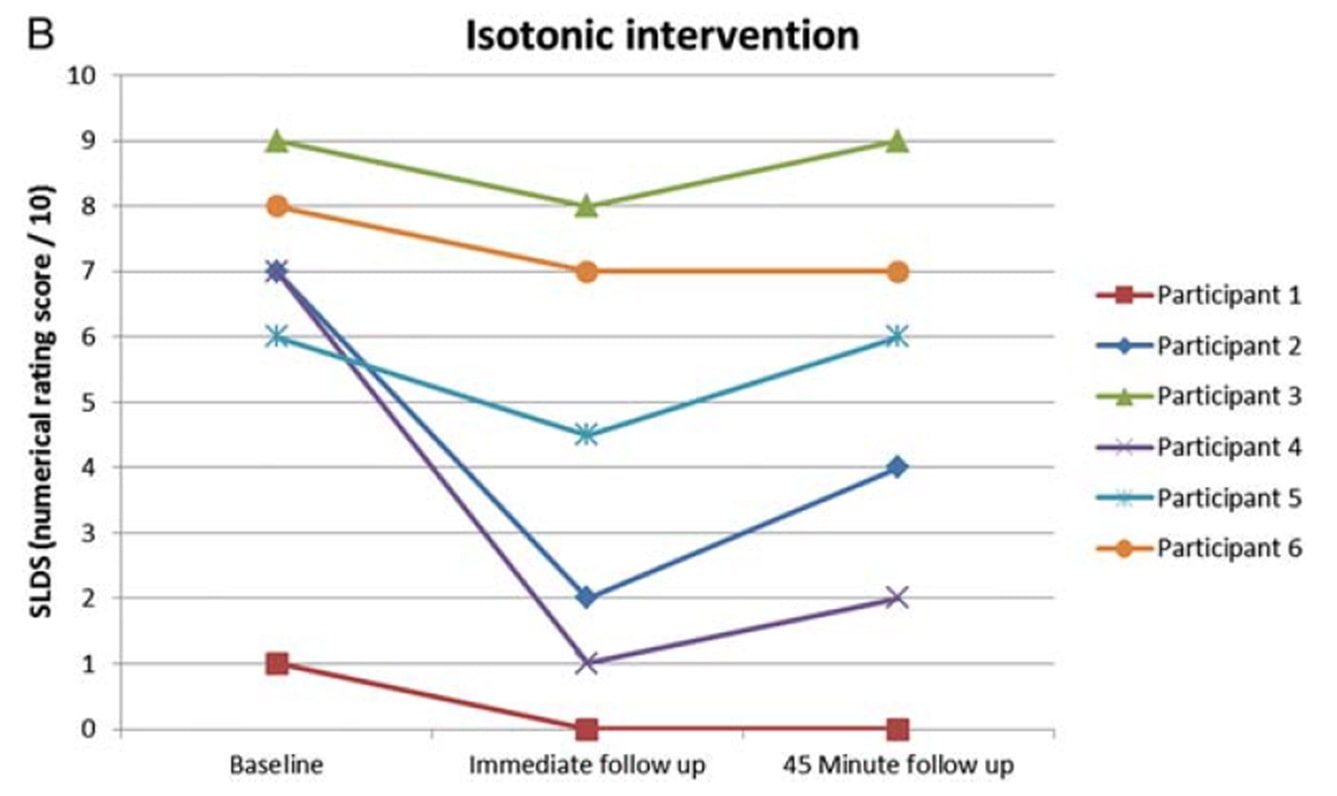
The same authors did a follow-up in-season study with jumping athletes two years later (Rio et al. 2017) in which they compared an isometric program and an isotonic program to each other. In this study the results were a bit more heterogeneous with both groups with a greater immediate pain decrease in the isometric group:
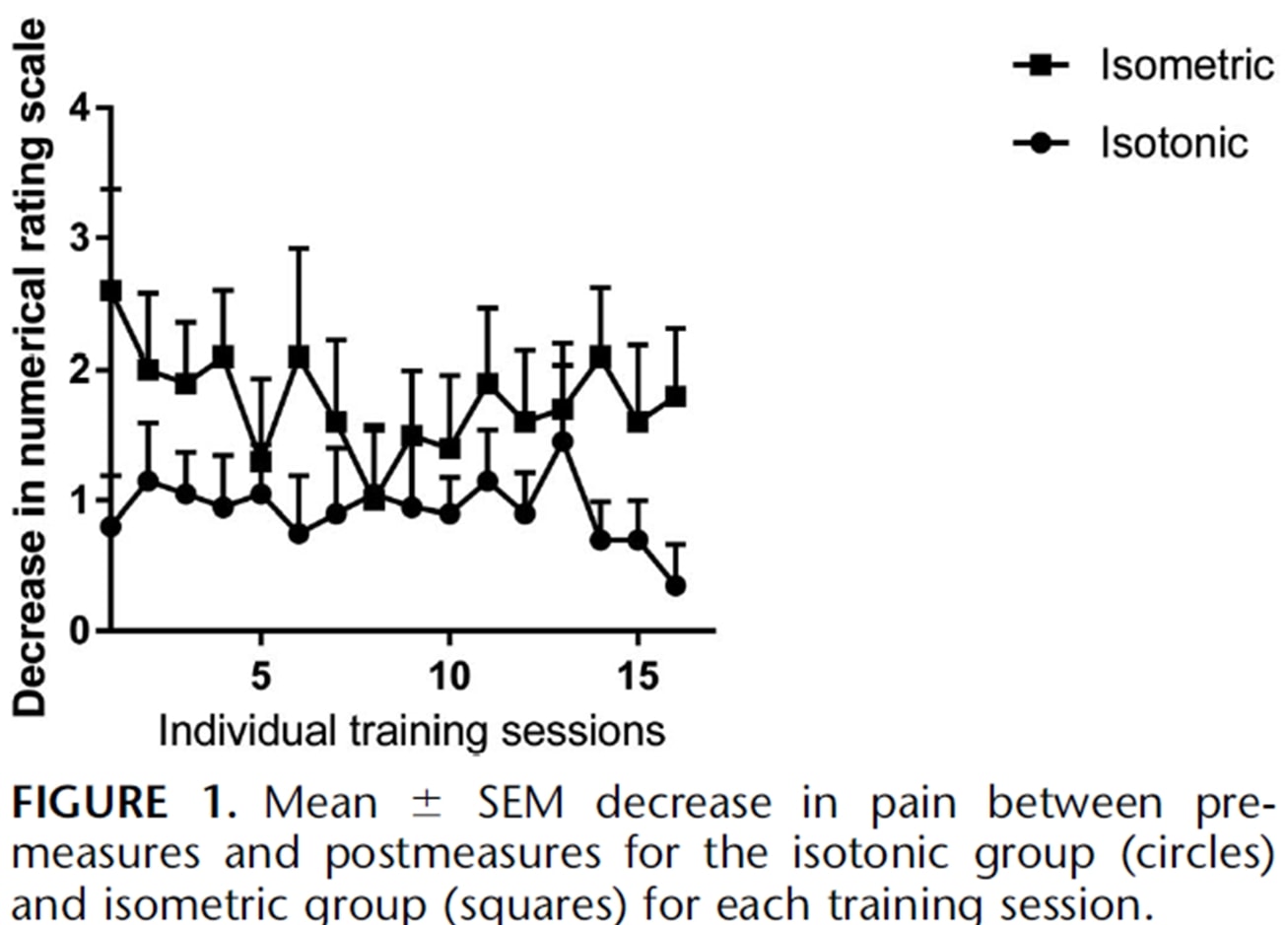
A recent study by Holden et al. (2019) looked at the effect of isometrics in patellar tendinopathy as well and did not find any analgesic effect:
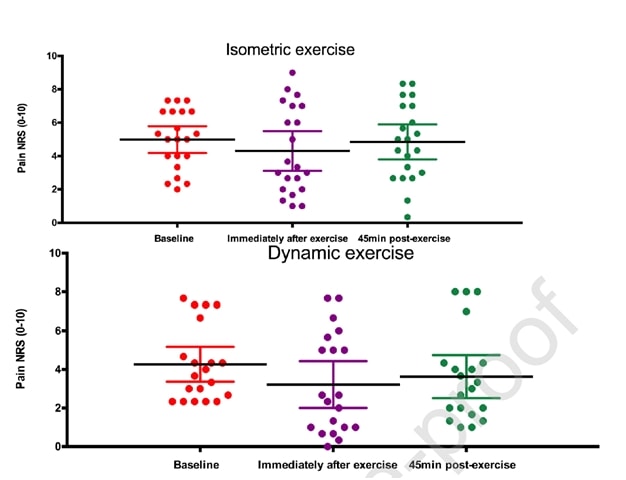
Figure from Holden et al. (2019)
However, a high percentage of women and a relatively high average age is untypical for patellar tendinopathy, which is usually a disease of young jumping men. So it could be that the diagnosis of patellar tendinopathy was not correct in some cases. Now while those two studies were conducted for patellar tendinopathy, let’s look if we can transfer these results to other tendons.
Stage 2 – Restoration of muscle bulk and strength and induce tendon adaptation: Isotonic loading
- When the quads can be loaded isotonically with no pain exceeding NRS 3/10, this stage can be initiated.
- Heavy slow resistance activities between 10° and 60° of knee flexion initially and progressed toward and beyond 90° of flexion as pain permits. These include leg presses, squats, hack squats, split-squat, and seated knee extensions. Double-legged initially and progress towards single-leg as soon as pain allows. Kongsgaard et al. used 3 to 4 sets every second day at a resistance corresponding to 15RM and progressed to 6RM. Continue stage 1 exercises on the days in between the heavy slow resistance exercises are performed.
Stage 3- Energy-storage loading: Increase load tolerance and improve power
- When good strength is achieved and the athlete tolerates single-leg loads with around 150% of body weight (for example 4 sets of 8 reps of a single-leg press), this phase can be initiated if no pain beyond NRS 3/10 is seen within the 24 h post-training.
- The initiation can be a bilateral leg press with loads of 3 times body weight (or 1.5 times in case single leg) as this exerts a patellar force corresponding to the forces seen during landing from a vertical jump
- Jump sequences with stop lands, jumping and landing, acceleration and deceleration, cutting and directional changes
- Volume (the number of jumps, contacts) progressed before the intensity (height, speed)
- Perform every third day and continue isometric loading and isotonic loading every second and third day.
Stage 4 – Return to sport
- Graded return to training and competition where initially the training matches the volume and intensity of the stage 3 exercises and progresses to a volume and intensity as required by the sport-specific situation.
- Maintenance of stage 2 exercises at least twice a week and eventually the stage 1 exercises prior to or after training.
Be aware that the whole rehab process can be slow and sometimes take more than 6 months. A study by Bahr et al. (2014) found that only 46% of athletes with patellar tendinopathy were able to return to full training and were pain-free after an eccentric training program for 12 months.
Do you want to learn more about how to treat tendons? Then check out our blog articles:
- 6 Risk factors for tendinopathy You Need to Know (#5 might surprise you!)
- Isometrics – A Wonder Weapon to Decrease Pain?
- 7 Crucial Facts You Didn’t Know about Tendons
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
THE BIG 3 - ADVANCED REHABILITATION OF HAMSTRING, QUADRICEPS, AND CALF MUSCLE- AND TENDON INJURIES


What customers have to say about this course
- Ivo Rigter07/11/25The Big 3 Prima informatieve cursusDavid Norenlind09/02/25Fantastic course on the topic of muscle and tendon injury The course does a great job of summarizing the research in the field and Enda provides clinical expertise along the way. A must-do course for anyone wanting to deepen their knowledge of muscle and tendon injuries.
- Senne Gabriëls25/12/24Worth the investment! This was my first online experience with courses. It was a very comprehensive and complete course. Management of tendon and muscle conditions in the lower limb became very clear in a way that no stone remained unturned.Eric van Bree09/12/24revalidatie onderste exstremiteiten zeer nuttig om je inzicht te vergroten bij revalidatie van sporters met klachten aan de onderste extremiteiten
- Ruben06/12/24Awesome info I really enjoyed the course. Could not recommend it enough!Thessa Budding06/12/24BIG 3 Interessant en meteen toepasbaar in de praktijk!
- Joris Bonarius25/11/24Informative and Efficient A very usefull course as an sportsphysio. Focussing on all important factors in injury risk, prevention, rehab and more!Pete23/11/24Course Summary I thought the course presented great content and was well organized. The format moving from general to injury specific was easy to follow. It could have been helpful to have a few more narrative sections, especially for the Case studies. Being in a High Performance setting, the course also allowed me to get some confirmation bias while at the same time providing the foundational understanding of tissue biology. The exercises and progressions also provided an alternative for the clinician and performance specialist.
- Bas Slieker02/10/24Very detailed course I found the course to be very well structured in logical and clear steps. A nice balance between evidence and practical tools! I think they do a great job throughout the course of making it clear that injuries and recovery are both biomedical and psychosocial. In doing so, they highlight the complexity of the human being and discuss many of the risk factors and pitfalls/points of attention during the rehabilitation of the big 3!Pascal Van de Kamp24/09/24Very structured, thanks Very structured, covering everything from anatomy to injury to rehab and movement patterns. Quizes were a bit annoying after every chapter. Still enjoyed it, refreshing course to stay sharp in my rehab plans.
- Gustav Hübinette30/01/24The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries REVIEW OF THE BIG 3
I experienced the course as very well-structured, maintaining a clear thread throughout the entire program. The content is clearly based on updated evidence, providing numerous valuable tips and tricks for implementing rehabilitation of THE BIG 3.
What I had wished for to be different is to include more recorded lectures, as there is currently a considerable amount of test-based information.Yoran Deleu30/12/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries Well structured course from the theoretical background to clear practical exercises needed for rehabilitation! - Adam Stewart14/11/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries VERY THOROUGH AND EXCELLENT JOB USING EVIDENCE BASED PRACTICE
Enda does a great job with this course and dives into as much detail as you would like throughout. Excellent job of keeping the most up-to-date information in the presentation. Takes time to get through it all, but very worth itOlivier Gouvernet11/10/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries BIG §
The course is very well structured, the anatomical reminders are relevant, each stage of rehabilitation is well detailed and the videos of the exercises make it easy to see and understand what needs to be monitored and done.
In my opinion, the last phases of rehabilitation are the most interesting, as they are rarely covered. This helps to reduce the gap between the load at the end of treatment and the load of a return to sport. - Jeremy Beyer05/09/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries An excellent course on the rehabilitation and management of lower extremity muscle & tendon injuries! Enda covers serious range in this course with lessons on muscle & tendon physiology all the way to late stage rehab and discussions around power & reactive strength development. This course is comprehensive and covers many of the overlooked aspects of muscle and tendon rehab. Enda highlights foundational rehabilitation concepts in an easy to digest manner that is guaranteed to influence the way you practice.Beppeke Molenaar04/05/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries EXCELLENT COURSE, INCREDIBLY KNOWLEDGEABLE
This is a fantastic course, with loads of information that is very applicable to daily practice.
I think this course has offered me the most in terms of learning and professional development out of all the courses I’ve done so far.
The set-up of the course is really well-structured. The videos are clear, the information in the text is evidence-based, very in-depth, and at the end of each unit, you can find further readings for anyone who wants to dive even deeper into the material.
I would highly recommend this course! - Badrinath31/03/23The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries The presentation is quite evidence based and evidence informed. It is presented in a structured manner. The author has put lots of effort. It is an application based course.Frederik Adriaensens30/12/22The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries VERY NICE OVERVIEW OF ALL THE INFLUENCIAL MECHANICS AND REHAB OPTIONS
Thanks for the excellent refresher! - Aemy den Hollander04/05/22The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries AWESOME
the amazing amount of detail Enda gives was a huge Eye opener for me.
Not the regular elearning i was used to. love this!Nicolo16/01/22The Big 3 - Advanced Rehabilitation of Hamstring, Quadriceps, and Calf Muscle- and Tendon Injuries USEFUL AND INSPIRING
This course is really useful and well made.
If you really can learn all the notions , you’ll be a better physiotherapist for sure.




