AC Joint Pain / Acromioclavicular Injury | Diagnosis & Treatment

AC Joint Pain / Acromioclavicular Injury | Diagnosis & Treatment
Introduction & Epidemiology

The clavicle functions in support and mobility of the upper extremity. It serves as a transition point between the shoulder girdle and the trunk of the body, connecting the upper extremity to the axial skeleton. On top of that, it serves to protect the subclavian vessels and brachial plexus (Balcik et al. 2013).
A fibrocartilaginous intra-articular disk of variable size and shape is interposed between the bony articulation, which functions to correct bony incongruities between the concave acromial surface and the convex distal clavicle. Disk degeneration may begin as early as the second decade of life, often resulting in little more than a fibrocartilaginous remnant by early adulthood (Menge et al. 2014).
While injuries are a common precipitating cause of ACJ pain, arthritis is usually the main cause of pain and develops as a consequence of constant stress on the joint, often in people who perform repeated overhead lifting activities (Buss et al. 2003).
During your screening process, it is important to rule out a fracture of the clavicle or severe AC joint separation. Clavicular fractures account for 2,6-5% of all fractures and their mechanism of injury is similar to that of an AC injury (Melenevsky et al. 2011).
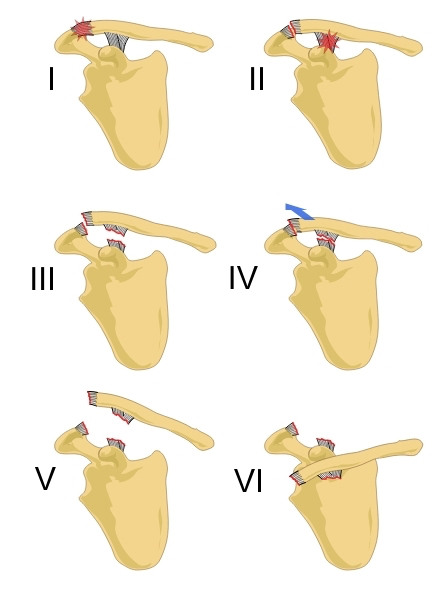
Acromioclavicular joint separations are graded according to severity based on the Rockwood classification:
I: AC ligament stretched
II: Partial rupture of AC ligaments
III: Complete rupture AC ligaments and coracoclavicular (CC) ligaments
IV: Clavicle displaced posteriorly over the acromion
V: Clavicle displaced just under the skin
VI: Clavicle underneath coracoid (very rare!)
There is consensus in the literature that grade I-III (according to the Rockwood classification) is managed conservatively and grades IV-VI are managed surgically (Reid et al. 2012).
The mechanism of injury is reported to be either a fall onto the point of the shoulder or the outstretched arm.
Epidemiology
Van der Windt et al. (1995) found a 1-year prevalence of 4% for acromioclavicular syndrome in a Dutch cohort of 349 patients with shoulder complaints (restriction of horizontal adduction, pain in the area of the AC joint, and/or C4 dermatome).
Östör et al. (2005) evaluated 131 patients with shoulder pain in an English cohort over a period of one year and found a prevalence of 24% for AC Joint pathology.
The differences between these findings might be explained due to different diagnostic criteria that were used, which were more strict in the study of Van der Windt et al. (1995).
So one might assume that the study of Östör et al. (2005) includes a high rate of false-positive results as they classified AC joint pathology based on painful horizontal adduction only.
For AC joint sprains Hibberd et al. (2016) found an incidence rate of 1,72 cases per 10.000 athlete-exposures. The majority of sprains were reported in football (50,4%), followed by ice hockey (34,6%), wrestling, and during competition (66,0%). The male: female ratio was 4.67 with most sprains being caused by player contact (54,7%) followed by surface contact (29,0%).
The Recurrency rate was as high as 9,7% with 1% of all sprains requiring surgery.
Be aware that diagnostic imaging of the AC joint can be misleading. Jordan et al. (2002) have found that the only statistically significant correlation was between the high signal in the distal clavicle and clinically found degenerative changes. Furthermore, they state that a weaker relationship existed between the fluid in the joint and clinical examination and between increasing degenerative changes and advancing age. Otherwise, no material relationship was found between any of the other MRI abnormalities and the clinical picture.
On top of that, Girish et al. (2011) examined 51 asymptomatic shoulders in men (average age 56y, range 40-70y) and found a prevalence of osteoarthritis of the AC joint in 65% of all cases.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
Signs & Symptoms
AC arthritis generally presents with complaints of progressively worsening shoulder pain, although minor trauma or strenuous activity may cause an acute exacerbation of this chronic degenerative condition. The pain is typically located over the anterior aspect of the shoulder in the region of the AC joint or referred to the shoulder and upper arm.
Overhead activities, weight lifting, and cross-body movements using the affected arm often are associated with worsening symptoms.
Pain at night is more common when patients lie on the affected side and difficulty sleeping can be a reason why contact with a health professional is sought in the first place.
Additionally, popping, clicking, grinding, and a catching sensation with movement of the shoulder might be present. A careful history of trauma or injuries can raise suspicion for instability or other associated pathologies (Menge et al. 2014).
Cadogan et al. (2013) have developed a cluster including signs & symptoms and items from physical examination in order to diagnose non-traumatic AC joint.
Examination
The painful arc test can be used in the evaluation of the symptomatic AC joint as well. The only difference compared to the subacromial pain syndrome category is that patients commonly report symptoms at shoulder flexion and abduction end range between 170-180° of movement:
Krill et al. (2018) have performed a systematic review evaluating the most accurate combination of physical tests in order to evaluate the ACJ as the source of nociception. Watch the following video to learn which tests have been included:
Other common orthopedic tests for the AC Joint are:
- AC Shear Test
- Paxinos Sign
- AC Resisted Extension Test
- AC Joint Line Tenderness
- Cluster of Chronopoulos
LEARN TO DISTINGUISH SHOULDER FACTS FROM FICTION

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK