Hip Osteoarthritis: The New 2025 Clinical Practice Guideline for Physiotherapists

Hip osteoarthritis (OA) remains one of the most common sources of lower-limb pain and functional decline encountered in musculoskeletal physiotherapy. Despite its prevalence, practice variation persists, ranging from inconsistent exercise dosing to an overreliance on passive modalities or imaging pathways that offer little clinical value.
The 2025 Clinical Practice Guideline (CPG) by Koc et al., published in the Journal of Orthopaedic & Sports Physical Therapy, provides the first major update since 2017 and synthesizes new high-quality research to guide assessment, conservative management, and outcome tracking for adults with hip OA.
This article summarizes the key updates through a physiotherapist’s lens, highlighting the clinical implications of each recommendation and the shifts from the 2017 guideline.
The 2025 Clinical Practice Guidelineprovides the first major update since 2017 and synthesizes new high-quality research to guide assessment, conservative management, and outcome tracking for adults with hip OA.
Why This Guideline Matters
Developed by a multidisciplinary team representing orthopedic physical therapy practice, manual therapy, movement science, surgery, residency education, outcomes research, and guideline methodology, the 2025 CPG reflects a comprehensive, cross-disciplinary review of current best evidence.
Importantly, the review process also included individuals living with hip osteoarthritis, whose insights contributed to the refinement of recommendations. Additionally, the guideline was posted for public comment through APTA Orthopedics, allowing patients, clinicians, and other stakeholders to provide feedback that was incorporated into the final version before publication.
Evidence Grades Explained
Each recommendation is assigned an evidence grade indicating the strength and certainty of the supporting research:
- Grade A – Strong evidence: Supported by a body of high-quality research such as well-designed randomized trials, prospective studies, or systematic reviews, providing strong confidence in the recommendation.
- Grade B – Moderate evidence: Supported by at least one high-quality randomized trial or multiple moderately rigorous studies, making the recommendation reliable in most clinical situations.
- Grade C – Weak evidence: Supported by a single moderately rigorous study or several lower-quality studies (e.g., retrospective designs or case series), sometimes supplemented by expert consensus.
- Grade D – Conflicting evidence: Higher-quality studies exist but do not agree in their conclusions, requiring clinicians to interpret findings in context.
- Grade E – Theoretical/foundational evidence: Based primarily on basic science, biomechanical, conceptual, or cadaveric research rather than clinical trials.
- Grade F – Expert opinion: Supported mainly by the clinical experience and consensus of the guideline development team when research evidence is lacking.
Online Course
Book your spot now and gain the skills and confidence to manage upper and lower extremity cases with clarity in everyday outpatient practice.

Key Clinical Recommendations
1. Assessment & Diagnosis
Comprehensive Subjective & Physical Examination:
Clinicians should perform a thorough history and physical exam assessing symptom behavior, irritability, gait, ROM, strength, and functional limitations, with provocation tests (e.g., FABER) used judiciously.
Diagnostic Criteria:
Diagnosis is supported by:
- Hip pain in adults >50 years of age
- Morning stiffness <60 minutes
- Painful and restricted passive IR
- IR <24° or ≥15° less than the contralateral side
Imaging :
Follow American College of Radiology criteria:
- First-line: AP pelvis and hip radiographs
- If unclear or extra-articular pathology suspected: diagnostic ultrasound
- MRI/CT only when radiographs + ultrasound are nondiagnostic
Best Practice Examination Set:
To standardize assessment, clinicians should collect:
- One self-report measure: WOMAC, HOOS, or PROMIS
- One performance measure: 6MWT, 30-s chair stand, TUG, or stair test
- Impairments: hip ROM, hip strength (all planes), FABER, NPRS
2. Rehabilitation Principles
Exercise Therapy (Grade A): The primary intervention for hip OA. Prescribe individualized strengthening and mobility programs, 1–5 sessions/week for 5–16 weeks, 30–120 minutes per session. Aquatic therapy is effective for pain, ROM, gait, balance, and function.
Manual Therapy (Grade A): Use hip joint mobilization techniques—including high-force long-axis distraction to improve ROM, low-force distraction to reduce pain, and mobilization-with-movement for quick functional gains.
Dry Needling (Grade A): Recommended for Grades II–III hip OA for short-term improvements in pain, ROM, strength, and function. Target iliopsoas, rectus femoris, TFL, and gluteus medius/minimus using a fast-in fast-out technique.
Patient Education (Grade B): Include guidance on exercise principles, activity modification, joint unloading, and weight-supporting strategies. New evidence supports automated internet-based pain coping skills training as an adjunct.
Functional, Gait & Balance Training (Grade C): Provide impairment-based gait and balance retraining and instruction in assistive devices when indicated.
Weight Loss (Grade B): Collaborate with physicians/dietitians toward a 5–7.5% body-weight reduction for individuals with BMI >25–30 kg/m².
3. Adjunct Modalities
Therapeutic Ultrasound (Downgraded — Grade D):
New RCT evidence shows no added benefit of continuous, pulsed, or combined ultrasound beyond placebo, reversing the 2017 recommendation.
Bracing (Grade F):
Not first-line treatment. May be considered after exercise and manual therapy fail, particularly in bilateral OA requiring pivoting or turning demands.
4. Pharmacological Treatment
The guideline restates 2017 findings on NSAIDs, COX-2 inhibitors, and corticosteroid injections for symptom relief, with caution regarding gastrointestinal side effects and potential (but unconfirmed) OA progression concerns.
5. Progression
Functional progression should be monitored through:
- Improvements in validated outcome measures
- Gradual progression of load based on symptom irritability
- Recovery of hip ROM and strength
- Performance on functional tests such as walking distance, stair climbing, and sit-to-stand
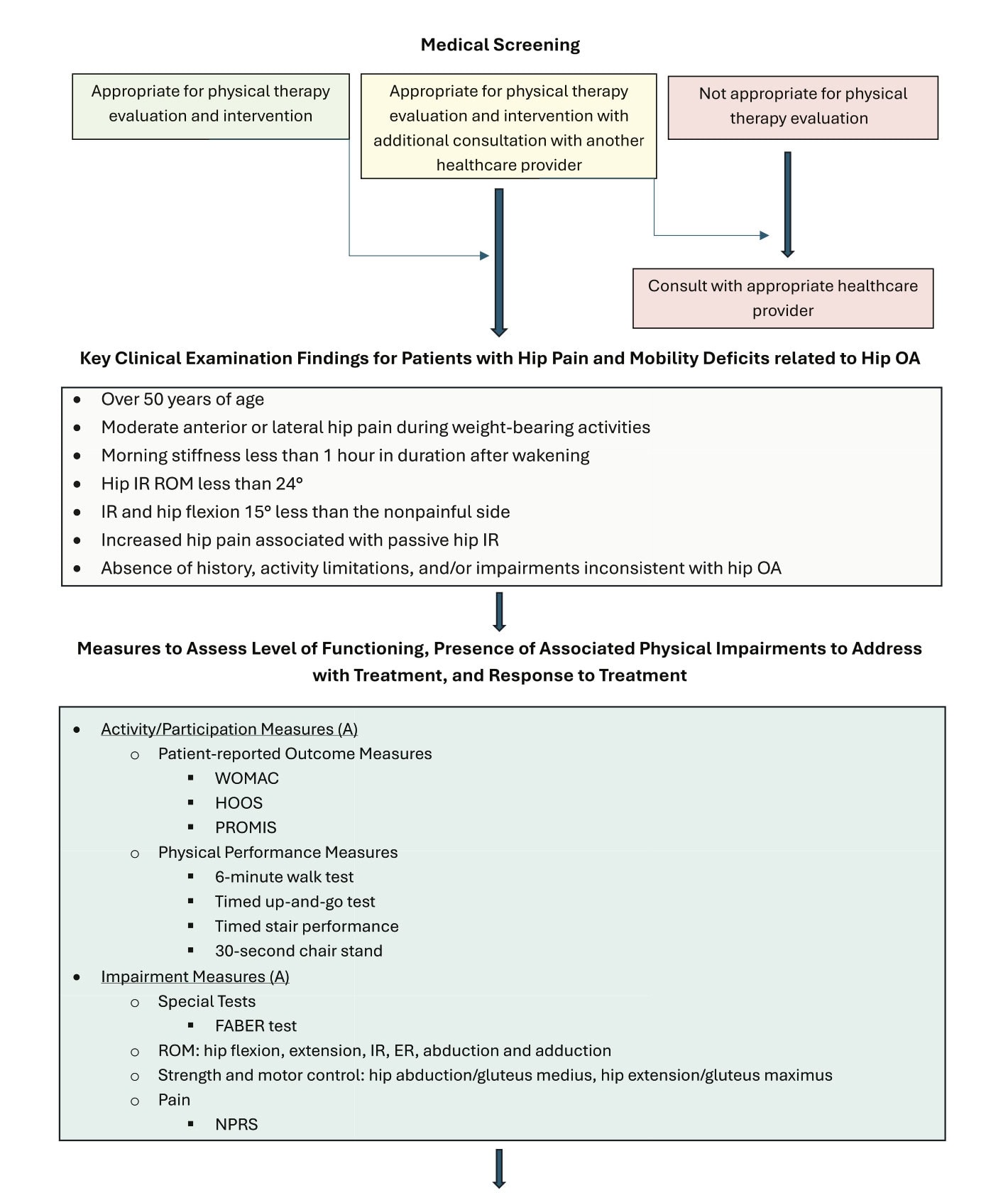
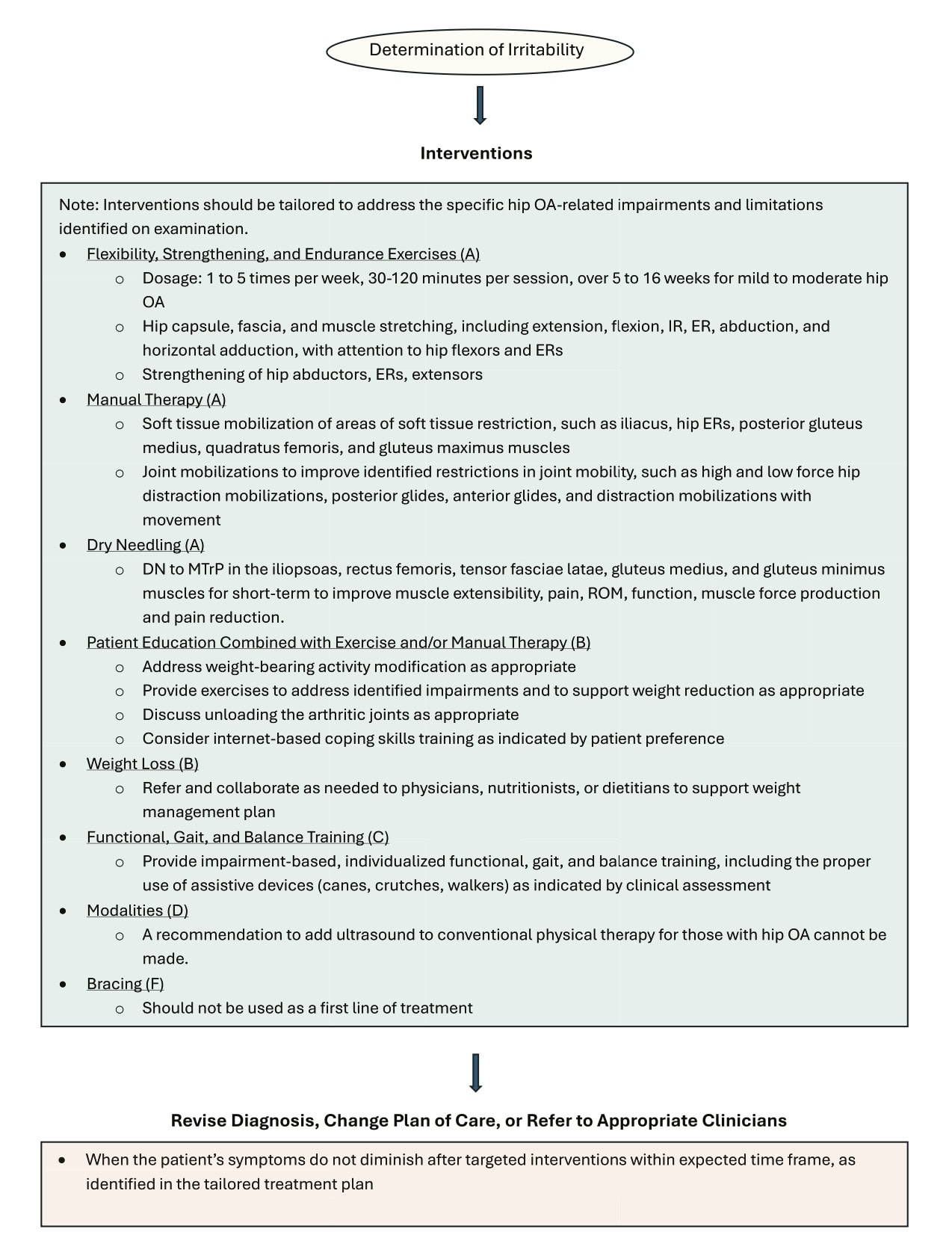
Hip Osteoarthritis Clinical Practice Guideline recommendation diagram.
Summary
The 2025 Hip OA CPG strengthens the emphasis on active rehabilitation, progressive loading, manual therapy, and dry needling while refining diagnostic pathways and standardizing assessment. It integrates new research across multiple domains and clarifies where evidence has evolved since 2017.
Changes from the 2017 guideline:
- Changes from the 2017 Guideline:
- Integration of new evidence (2016–2023): Multiple new RCTs, systematic reviews, and meta-analyses were incorporated across key intervention areas.
- Dry needling added (Grade A): A new strong recommendation supported by high-quality evidence for short-term improvements in pain, ROM, strength, and function.
- Updated imaging pathway: Adoption of ACR criteria for appropriate use of radiographs, diagnostic ultrasound, and MRI/CT.
- Standardized “Best Practice” examination set: Introduction of a core set of outcome measures, physical performance tests, and impairment measures to improve consistency across clinicians.
- Exercise therapy strengthened: New meta-analyses reinforce individualized progressive strengthening and aquatic therapy, with clearer dosing parameters.
- Manual therapy evidence expanded: Recent trials clarify the benefits of high- vs low-force hip distraction and mobilization-with-movement.
- Patient education updated: Now includes evidence for automated internet-based pain-coping skills training alongside exercise and/or manual therapy.
- Therapeutic ultrasound downgraded (now Grade D): A new high-quality RCT demonstrates no added benefit compared with placebo, reversing the previous 2017 short-term recommendation.
Limitations & Conclusion
Despite substantial updates, the 2025 guideline highlights several ongoing limitations. Many intervention areas still lack high-quality trials, especially for functional training, gait retraining, balance interventions, and bracing. Evidence for patient education beyond automated pain-coping skills training remains limited, and therapeutic ultrasound research continues to conflict. Several recommendations remain unchanged from 2017 simply because no new studies have been published.
As emphasized in the guideline’s statement of intent, these recommendations serve as evidence-informed guidance (not prescriptive standards) and must be applied using clinical reasoning, patient goals, and individual presentation. The authors underscore the need for clinicians to document deviations when appropriate and to contribute future outcomes to strengthen the evidence base. The 2025 CPG provides an updated, patient-responsive, and methodologically rigorous framework that reinforces active rehabilitation and supports consistent, evidence-based care for adults with hip osteoarthritis.
Reference
Koc, T. A., Jr, Cibulka, M., Enseki, K. R., Gentile, J. T., MacDonald, C. W., Kollmorgen, R. C., & Martin, R. L. (2025). Hip Pain and Mobility Deficits-Hip Osteoarthritis: Revision 2025. The Journal of orthopaedic and sports physical therapy, 55(11), CPG1–CPG31. https://doi.org/10.2519/jospt.2025.0301

Anibal Vivanco
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.




