Learn
The Shoulder Joint
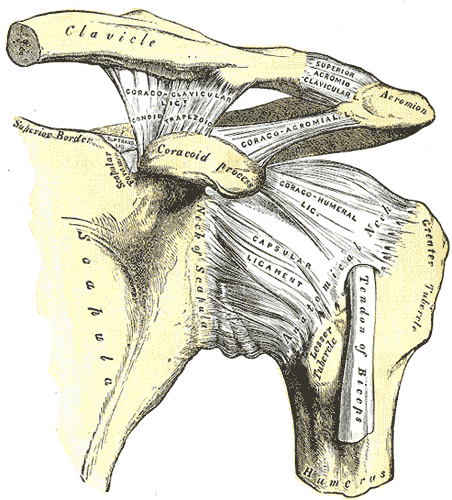
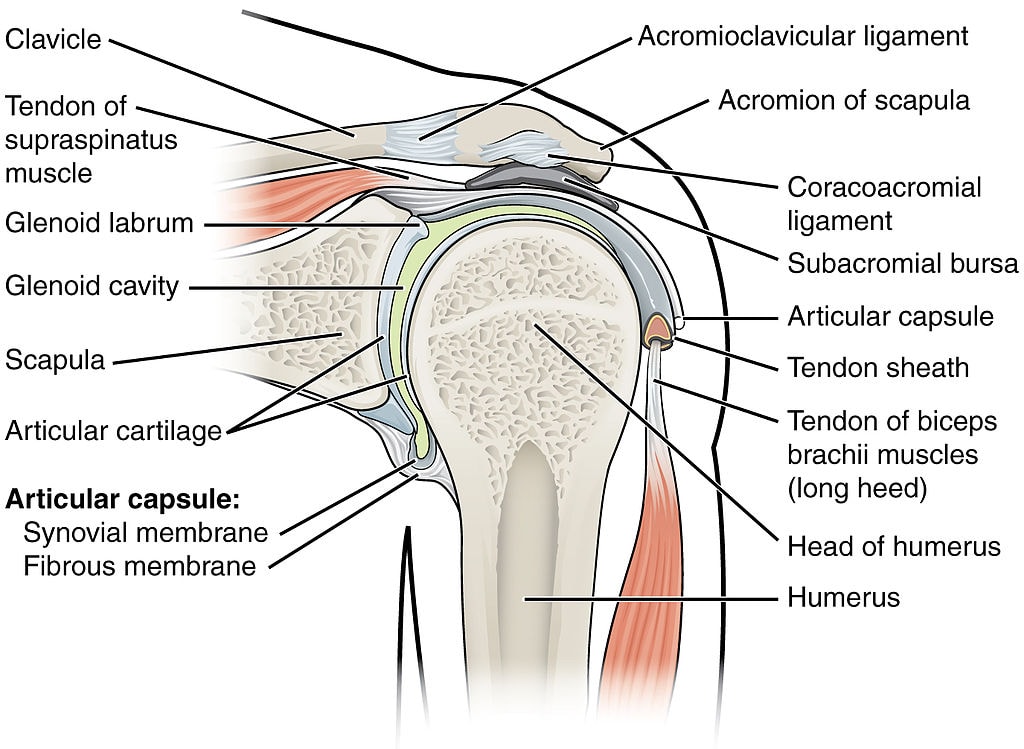
The shoulder joint is one of the most complex joints in the human body. When we refer to the shoulder we usually mean the glenohumeral joint, which is formed by the head of the humerus and the glenoid fossa of the scapula. We shouldn’t forget that for proper shoulder function, coordinated movement of several other joints is necessary. These are:
- The sternoclavicular (SC) joint: Clavicle and Sternum
- The acromioclavicular (AC) joint: Acromion and Sternum
- The scapulothoracic joint: Not a true anatomic joint. Depends on the integrity of the abovementioned joints.
Epidemiology (Luime et al. 2004)
The literature describes the incidence of shoulder pain to be between 0,9 – 2,5%. (31-35y: 0,9%; 42-46y: 2,5%; 56-60y: 1,1%; 70-74y: 1,6%)Shoulder pain is very common with a point prevalence of 6,9 to 26% in the general population. The 1-month prevalence for shoulder pain is described at 18,5-31%, 1-year prevalence ranges from 4,7 – 46,7%, with a lifetime prevalence of 6,7-66,7%. This makes shoulder pain the third most common musculoskeletal complaint after low back and neck pain with cuff-related problems as the most common shoulder injury. In general, the prevalence of shoulder pain is higher in women and increases with age.
Course
Shoulder pain generally has an unfavorable prognosis with only 30% of patients recovering after six weeks and 54% after six months (Kuijpers et al. 2006). Van der Windt et al. (1996) report a median duration of complaints of 21 weeks. Luime et al. (2004) report that 50-70% of all patients still have complaints after six months, and 40-50% still experience complaints after one year. The recurrence of shoulder pain was reported to be 20-50%.
Prognostic factors
Verhagen et al. (2014) describe that the following factors are associated with a negative prognosis for recovery:
- High pain score at baseline
- Long duration of complaints
- Insidious onset of complaints
- Concomitant neck pain
- Impairments in activities of daily living (ADLs)
- Psychological factors without further specification
- Repetitive movements are described as a factor in work-related shoulder pain
Red flags
Next to the general red flags, specific red flags in the shoulder joint can be:
Region-specific red flags
- Tumors in the brain, breast, lung (most often Pancoast tumors), liver, and spine
- Infections: History of surgery, open wound, swelling, redness, heat fever
- Avascular necrosis: Trauma, Cancer, steroid use/abuse (Gruson et al. 2009)
Tract anamnesis
In general, all tissues irritating the diaphragm can create visceral referred pain in the shoulder
- Heart disease/angina: Often sharp stabbing pain in the left shoulder, arm, lateral neck, increasing with exercise; risk factors include: Age>40y, hypertension, diabetes, smoker, high cholesterol, etc.
- Respiratory system: Look for impairments in breathing, shortness of breath, dizziness, etc.
- Liver cirrhosis (right shoulder): excessive alcohol, family history of liver disease, history of Hepatitis B or C, obesity, jaundice, swollen legs, ankles, abdomen (ascites), feet
- Spleen (abscess or rupture can produce left ACJ pain): Kehr Sign –> Pain increases in supine with feet elevated (Söyüncü et al. 2012)
- Gall bladder/Cholecystitis (right scapula): Increase in pain after a fatty meal, fever, nausea, vomiting
- Peptic ulcer (deep dull pain felt mid-thoracic/scapula): Increases after meals, long-term use of NSAIDs
Apart from red flags, shoulder pain has to be distinguished from referred pain from the cervical facet joints in the neck, cervical myelopathy, or cervical radicular syndrome. So if concomitant neck pain is present, further examination of the neck region should be done in order to rule out the above-mentioned pathologies. In order to learn more about these differential diagnoses, we would like to refer you to the “Further reading” section at the bottom of this unit.
TWO MYTHS BUSTED & 3 KNOWLEDGE BOMBS FOR FREE
Basic Assessment
Shoulder pain can be roughly divided into three main groups:
- Shoulder pain with limited passive range of motion (PROM) and shoulder pain directly related to the glenohumeral joint (Frozen Shoulder or Osteoarthritis)
- Shoulder pain without limited PROM, but a painful abduction component (painful arc), usually indicating Subacromial Pain Syndrome (including rotator cuff pathology with or without tendinopathy of the biceps and bursitis)
- Other shoulder complaints without limited PROM and without a painful arc (Shoulder Instability, AC or SC Joint Pathology)
In order to divide your patient’s shoulder pain into one of those 3 categories, a basic assessment should be performed. It’s best to start with an Active Range of Motion Assessment:
Standard values for the range of motion in different directions are as follows:
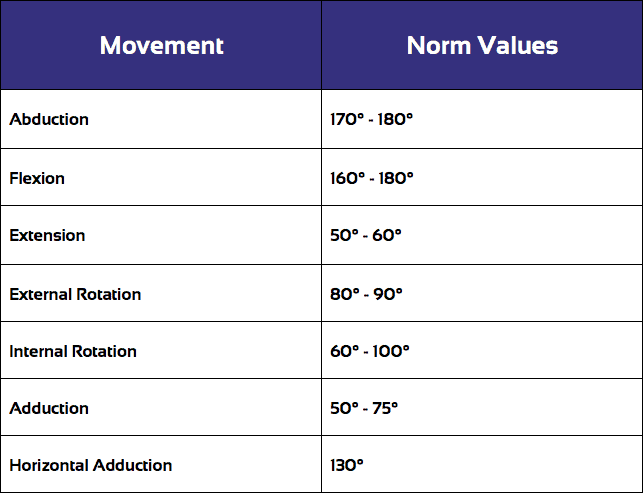
As described in the basic categorization above, it is important to look for a painful arc.
AROM assessment is then typically followed by Passive Range of Motion Assessment (PROM) which you can watch by a click on the following video:
During PROM assessment, it’s important to compare the range of motion as well as the end-feel of the affected shoulder with the unaffected side. After AROM and PROM assessment you should be able to categorize the patient into one of the three basic categories for shoulder pain.
Stenvers et al. (1977) have come up with 5 different quick tests in order to assess the mobility of the shoulder girdle.
Specific Pathologies in the Shoulder
There are several pathologies that are commonly seen in the shoulder area. For more information, click on the respective pathology (content will be added in the near future):
- Rotator Cuff Tear
- Full-Thickness Rotator Cuff Tears
- Scapular Dyskinesis
- Subacromial Pain Syndrome
- Internal Shoulder Impingement
- Shoulder Instability
- SLAP (Superior Labrum Tear from Anterior to Posterior) lesion/Biceps Tendinopathy
- Acromioclavicular Joint Pathology
- Frozen Shoulder
References
Like what you’re learning?
BUY THE FULL PHYSIOTUTORS ASSESSMENT BOOK
- 600+ Pages e-Book
- Interactive Content (Direct Video Demonstration, PubMed articles)
- Statistical Values for all Special Tests from the latest research
- Available in 🇬🇧 🇩🇪 🇫🇷 🇪🇸 🇮🇹 🇵🇹 🇹🇷
- And much more!