The relationship between stress and physical activity: how to aid our patients on a psychosocial level during physiotherapy consultation
The idea that the body and mind are two separate entities is already long overdue. While it was once believed that emotions and bodily functions were unrelated, over the past century, the prevailing view has shifted. Today, it is widely accepted that the body’s organs operate as an interconnected system, continuously influencing one another. When one part is affected, the rest respond in kind—similar to how pulling one end of a web stretches the other (Walker, 1956).
Background
In community-based practice, patients frequently present themselves with a wide range of symptoms of which 25 to 50% remain medically unexplained (Burton, 2003; Escobar et al., 2010; Olde Hartman et al., 2009). The link between medically unexplained symptoms and psychosocial factors, such as distress, anxiety, or depression, is clearly outlined in both the ICD-10 (World Health Organization [WHO], 2019) and DSM-5 (American Psychiatric Association [APA], 2013). As a result, international physiotherapy guidelines for managing conditions like lower back pain recommend screening and assessing psychosocial factors (Delitto et al., 2012), noting that:
‘’Psychosocial factors appear to play a larger prognostic role than physical factors in low back pain. There are some reviews that question if changes in behavioural variables and reductions of disability that facilitate an improvement in function, may be more important than physical performance factors for successful treatment of chronic low back pain’’
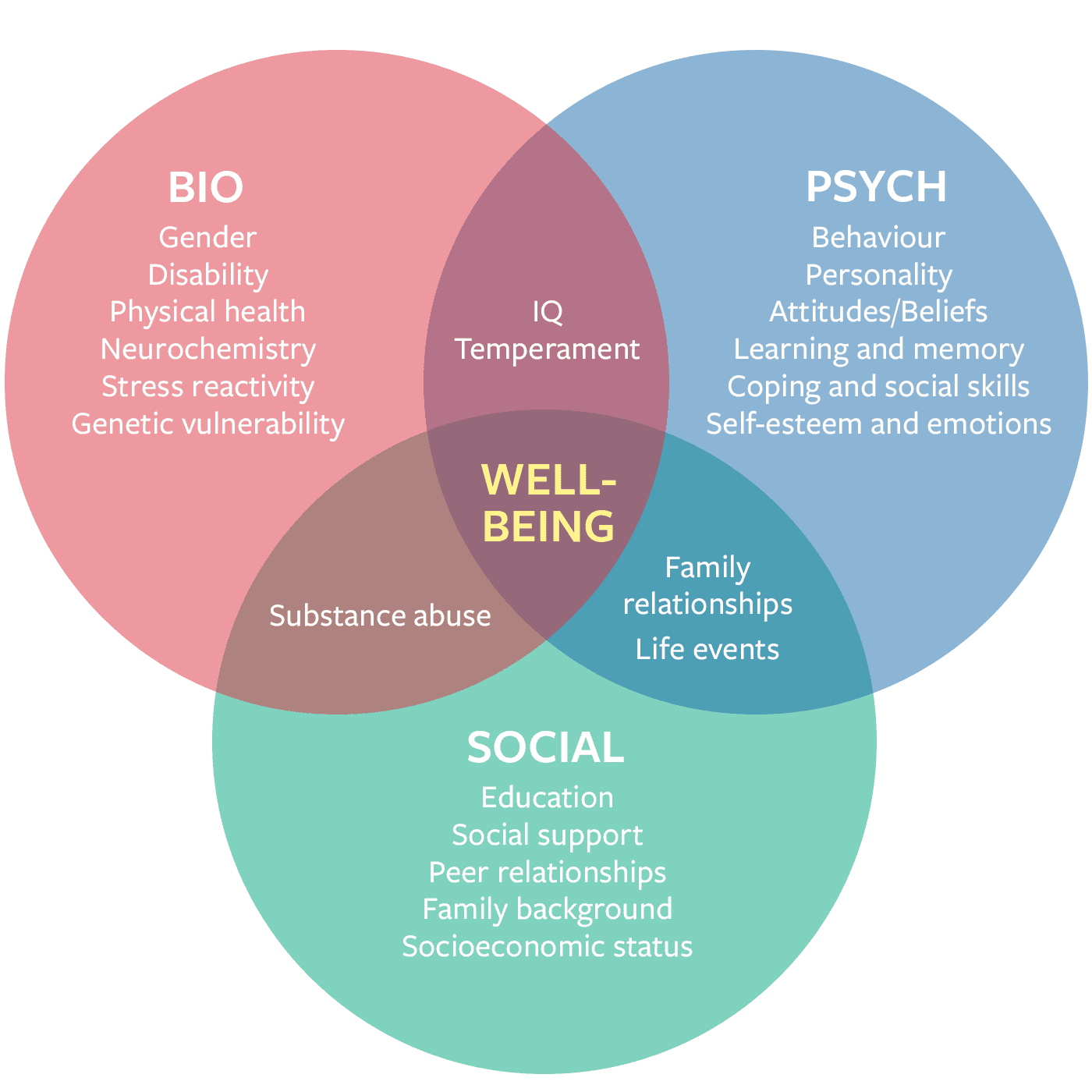
Figure 1: the biopsychosocial model, displaying the interaction between different factors for well-being (https://www.hgi.org.uk/news/latest-news/alarming-hijacking-biopsychosocial-model)
Most modern physiotherapy guidelines adopt a biopsychosocial model, emphasizing the continuous interaction between biological factors (such as genetics), psychological factors (such as distress), and social factors (such as social support). While the importance of psychosocial factors in the recovery process is well-documented, there are still no specific recommendations for clinicians on how to effectively address these aspects in treatment. So, what role can physiotherapists play in the management of psychosocial complaints?
Physical activity and psychosocial factors
Previous research has demonstrated the significant benefits of physical activity on distress, anxiety, and depression (Rebar et al., 2015; Schuch et al., 2019). Some studies even suggest that the benefits of physical activity interventions are comparable to those of psychotherapy and pharmacotherapy, with additional advantages in terms of cost, side effects, and other health benefits.
The mental health benefits of physical activity can rival those of psychotherapy or medication—without the side effects
An overview of reviews by Singh et al. (2023), which combined data from 1,039 trials and 128,119 participants, examined the impact of physical activity interventions on distress, anxiety (Figure 2), and depression (Figure 3). The findings revealed that physical activity interventions were effective in managing psychosocial factors across diverse populations, including healthy individuals, people with mental health disorders, cancer patients, and those with multiple sclerosis, among others. The interventions included strength training, endurance training, yoga, stretching, and mixed modalities. All of these interventions were found to be effective, though resistance exercise had the most significant impact on depression, while yoga and other mind-body exercises were most effective for reducing anxiety. Overall, moderate- and high-intensity training proved to be more beneficial than low-intensity training.
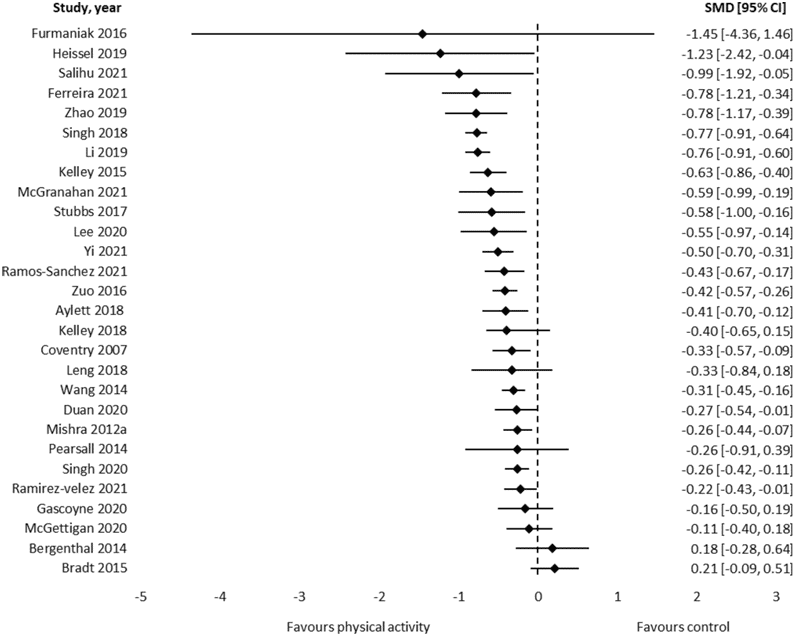
Figure 2: results of the meta-analysis that assessed symptoms of anxiety using standardized mean differences
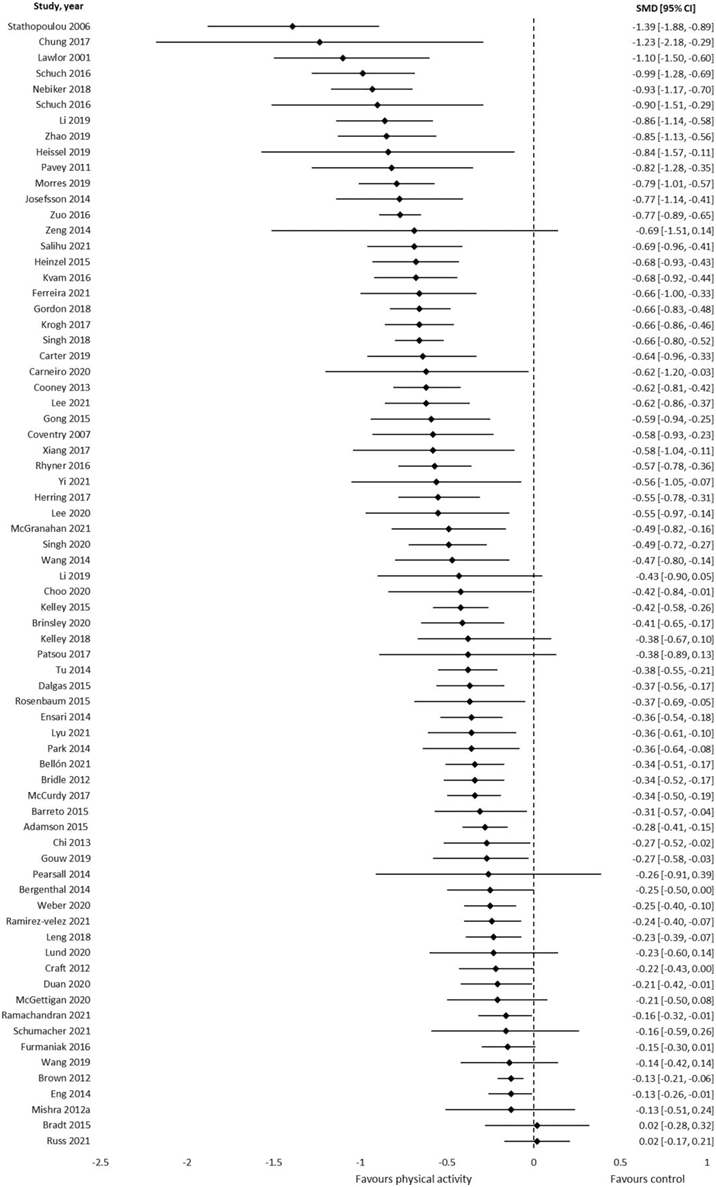
Figure 3: results of the meta-analysis that assessed symptoms of anxiety using standardized mean differences
One of the key features of these interventions is that they are often conducted in group settings. In an era where loneliness is a growing societal challenge, particularly among the elderly population, social engagement has become increasingly important (Pels et al., 2016). Research has shown that social isolation can have significant negative effects on both mental and physical health, making the role of social activities even more vital. Psychological studies have demonstrated that group exercise can be an effective intervention for alleviating loneliness, with some research indicating that it can be just as effective as psychological group therapy in reducing feelings of isolation and improving emotional well-being (Savikko et al., 2010).
Movement is medicine—and community is part of the dose.
Moreover, group exercise not only provides the physical benefits of movement but also fosters a sense of community and belonging (Golaszewski et al., 2023). These social interactions can boost self-esteem, improve mood, and create a support system that contributes to better overall mental health. For individuals experiencing chronic conditions, such as mental health disorders or physical disabilities, the additional social support offered through group settings can enhance motivation, adherence to treatment, and recovery outcomes. As such, integrating social elements into physical activity interventions can significantly improve their effectiveness in promoting both physical and mental well-being.
Sign up for this online course
Join our online course Central Sensitization: From the Lab to the Clinic with Prof. Dr. Jo Nijs and learn to provide the best-evidence based care for patients with chronic pain

Practical implications
Physical therapists are uniquely positioned to support patients not only in their physical recovery but also in enhancing psychosocial well-being. While movement remains our primary tool, integrating psychosocial considerations into everyday practice does not require a radical change in scope—rather, it involves small, meaningful shifts in our approach to patient interaction and intervention planning.
Clinicians can start by creating a safe, validating environment where patients feel comfortable discussing emotional or psychosocial distress. Simple communication strategies such as active listening, open-ended questioning, and empathetic reflection can build rapport and trust. For example, asking, “How are you coping with your symptoms day-to-day?” or “What concerns you most about your condition?” may uncover emotional or social stressors contributing to the patient’s experience of pain or disability. It is important to openly communicate with the patient regarding this topic to make sure that they are comfortable with sharing their thoughts and feelings.
In addition, motivational interviewing techniques can be used to encourage behavioural change by exploring the patient’s own values and goals. Rather than prescribing generic exercises, you might ask: “What kind of physical activity have you enjoyed in the past?” or “What would being more active allow you to do that you miss now?”—helping patients reconnect with personally meaningful goals. Finally, for complex cases involving severe distress or social dysfunction, physiotherapists can play an important role in a multidisciplinary team. Timely referrals to psychological or social services can ensure a patient receives well-rounded, holistic support.
5 Practical tips for managing biopsychosocial factors in practise
- Use open-ended questions to explore psychosocial challenges (e.g., “What do you find most difficult about your condition?”). Open communication regarding stressors can be very meaningful; however, do not try to replace a psychologist by going to much into detail, background, or psychological trauma.
- Collaborate with other professionals when psychosocial issues fall outside your scope—referrals are not a sign of failure, but of patient-centred care.
- Encourage patients to meet the World Health Organization’s physical activity guidelines (150 minutes of moderate or 75 minutes of vigorous activity per week), emphasizing the mental as well as physical health benefits. Where possible, tailor activity types to symptoms: recommend strength training for depression-related complaints and yoga or other mind-body exercises for anxiety and distress.
- Encourage participation in group classes or community-based activities for motivation, adherence and social support.
- Use metaphors to explain the stress-pain connection if that hinders the patient from being physical active (‘’Your nervous system is like an overly sensitive smoke alarm—it goes off at the slightest hint of steam, not just real fire.”)
By applying these strategies, physiotherapists can move beyond the biomechanical model and become agents of change in both the physical and mental health of their patients.
Conclusive thoughts
While international physiotherapy guidelines advocate for a biopsychosocial approach to understanding the body, specific treatment recommendations for addressing psychosocial factors remain limited. Although psychosomatic physiotherapists frequently utilize interventions such as breathing techniques and relaxation exercises, the average physical therapist may also play a significant role in managing these factors.
The field of physiotherapy has undergone a shift over the past few decades, transitioning from predominantly hands-on treatment to a focus on exercise therapy and education. While guidelines have formally moved from a purely body-focused approach to incorporating the biopsychosocial model, there is still considerable room for improvement in how we educate and support patients in managing both their physical and psychosocial well-being. If we believe in the existence of the biopsychosocial model to explain the body’s processes, perhaps we should act accordingly.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
Burton, C. (2003). Beyond somatisation: A review of the understanding and treatment of medically unexplained physical symptoms (MUPS). British Journal of General Practice, 53(488), 231–239. https://doi.org/10.3399/09601640320016696
Delitto, A., George, S. Z., Van Dillen, L., Whitman, J. M., Sowa, G., Shekelle, P., Denninger, T. R., & Godges, J. J. (2012). Low back pain. Journal of Orthopaedic & Sports Physical Therapy, 42(4), A1–A57. https://doi.org/10.2519/jospt.2012.42.4.A1
Escobar, J. I., Cook, B., Chen, C. N., Gara, M. A., Alegría, M., Interian, A., & Diaz, E. (2010). Whether medically unexplained or not, three or more concurrent somatic symptoms predict psychopathology and service use in community populations. Journal of Psychosomatic Research, 69(1), 1–8. https://doi.org/10.1016/j.jpsychores.2009.12.001
Golaszewski, N. M., LaCroix, A. Z., Hooker, S. P., & Bartholomew, J. B. (2022). Group exercise membership is associated with forms of social support, exercise identity, and amount of physical activity. International Journal of Sport and Exercise Psychology, 20(2), 630–643. https://doi.org/10.1080/1612197X.2021.1891121
Olde Hartman, T. C., Borghuis, M. S., Lucassen, P. L., van de Laar, F. A., Speckens, A. E., & van Weel, C. (2009). Medically unexplained symptoms, somatisation disorder and hypochondriasis: Course and prognosis. A systematic review. Journal of Psychosomatic Research, 66(5), 363–377. https://doi.org/10.1016/j.jpsychores.2008.10.003
Pels, F., & Kleinert, J. (2016). Loneliness and physical activity: A systematic review. International Review of Sport and Exercise Psychology, 9(1), 231–260. https://doi.org/10.1080/1750984X.2015.1061057
Rebar, A. L., Stanton, R., Geard, D., et al. (2015). A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychology Review, 9, 366–378. https://doi.org/10.1080/17437199.2015.1072149
Savikko, N., Routasalo, P., Tilvis, R., & Pitkälä, K. (2010). Psychosocial group rehabilitation for lonely older people: Favourable processes and mediating factors of the intervention leading to alleviated loneliness. International Journal of Older People Nursing, 5(1), 16–24. https://doi.org/10.1111/j.1748-3743.2009.00202.x
Schuch, F. B., Stubbs, B., Meyer, J., et al. (2019). Physical activity protects from incident anxiety: A meta-analysis of prospective cohort studies. Depression and Anxiety, 36, 846–858. https://doi.org/10.1002/da.22915
Singh, B., Olds, T., Curtis, R., et al. (2023). Effectiveness of physical activity interventions for improving depression, anxiety, and distress: An overview of systematic reviews. British Journal of Sports Medicine, 57, 1203–1209. https://doi.org/10.1136/bjsports-2022-106300
Walker, N. (1956). The definition of psychosomatic disorder. The British Journal for the Philosophy of Science, 6(24), 265–299. https://doi.org/10.1093/bjps/VI.24.265
World Health Organization. (2019). International classification of diseases and related health problems (10th ed.). World Health Organization.

Guus Rothuizen
Physiotherapist, Researcher & Journalist
NEW BLOG ARTICLES IN YOUR INBOX
Subscribe now and receive a notification once the latest blog article is published.





