The Impact of Stress on Chronic Pain - Understanding the Stress-Pain Connection

Introduction
Chronic pain patients often feel left out in the cold since the management of their pain is often not fully successful. They can develop depressive feelings over time, or they have difficulties coping with their pain and get anxious and stressed, all human reactions, but it is in turn counterproductive and only pushes them further in a vicious cycle. When discussing the role of stress and depressive feelings in chronic pain, clinicians should be aware that their explanations may be perceived by some patients as dismissive, potentially causing anger or offense. Most of the time, they feel misunderstood, although the communication of the clinician assumes good intentions, it can be difficult to understand what drives pain to become chronic, and that also accounts for us as clinicians. Therefore, this publication by Fülöp et al. (2025) aimed to broaden our knowledge on the stress-pain connection and how psychosocial distress can induce chronic pain.
Methods
This article is written as a “short review” summarizing recent literature. It is important to know that it is not a systematic review. Instead, the authors synthesized existing research to introduce their research perspective on the interactions between chronic pain, stress, and co-morbid mood disorders. The review focuses on fibromyalgia as part of chronic primary pain, defined by the International Association for the Study of Pain (Nicholas et al. 2019).

Data was obtained from a literature review of:
- Clinical studies related to chronic pain, stress, and mood disorders, including functional magnetic imaging (fMRI) outcomes and postmortem brain tissue examination.
- Animal experiments of translational relevance, specifically focusing on rodent models of chronic primary pain, particularly those that use chronic stress paradigms as an etiological factor.
With a specific focus on fibromyalgia, the authors categorized and presented findings related to:
- Clinical data on the stress-pain connection interactions in fibromyalgia.
- Preclinical models used to investigate chronic primary pain and stress-related pain mechanisms, with a summary of various rodent models (e.g., repeated swim stress, intermittent cold stress, repeated sound stress, chronic restraint stress, reserpine-induced, and acid saline-induced models) and their observed behavioral (pain and mood) and molecular alterations (neuroinflammation and inflammatory mechanisms).
- The relationship between mood disorders (anxiety, depression) and chronic pain.
- The role of neuroinflammation and neuroplasticity changes as common mechanisms, integrating both clinical and preclinical findings.
- Potential mechanisms and novel therapeutic targets
They aimed to provide a comprehensive overview of the current understanding in the field to highlight the need for novel therapeutic approaches and explore the stress-pain connection.
Results
The review found evidence supporting a complex interplay between chronic psychosocial distress, neuroinflammation, neuroplasticity changes, and chronic primary pain, especially in fibromyalgia.
Chronic psychosocial distress as an etiological and aggravating factor of chronic primary pain
Clinical data found positive correlations between baseline stress levels and pain intensity scores in fibromyalgia and other chronic widespread pain conditions in a longitudinal study. Both stress and pain catastrophizing showed strong positive correlations with pain severity and the co-occurrence of multiple painful diseases. Psychosocial stressors influence the pathogenesis of low back pain, with inflammatory cytokine IL-6, norepinephrine, and resting heart rate suggested as predictive values. The impact of chronic pain on stress levels, anxiety, and depression is confirmed, and psychopathological profiles, stress, and coping mechanisms are associated with fibromyalgia symptoms and pain threshold decrease. The Trier Social Stress Test (an acute psychosocial stress task) decreased thermo- and mechanonociceptive thresholds, resulting in hyperalgesia (increased pain sensitivity) and allodynia (pain from non-painful stimuli) in fibromyalgia patients.
Mood disorders are common comorbidities
Clinical data indicate that higher percentages of mood disorders (depression and anxiety) are present in fibromyalgia patients compared to the healthy population. Depression as a comorbidity is suspected to worsen treatment outcomes in fibromyalgia patients. Pain severity and catastrophizing in women were associated with higher depression and anxiety levels. Personality traits like neuroticism, conscientiousness, and extraversion are associated with fibromyalgia symptoms including pain, depression, anxiety, and stress level
Neuroinflammation and neuroplasticity changes as common mechanisms of chronic primary pain
Clinical studies showed increased glial activation (microglia and astrocytes) in the brains of fibromyalgia patients, which correlated with fatigue and pain. Preclinical studies confirmed that chronic stress induces microglia and astrocyte activation, and various inflammatory parameters are elevated in animal models of FM. Inflammatory cytokines (like IL-6, IL-2, IL-1, TNFα) and neuropeptides (Substance P, Hemokinin-1) are implicated in both clinical and preclinical settings, with some showing positive correlations with pain intensity and psychological distress.
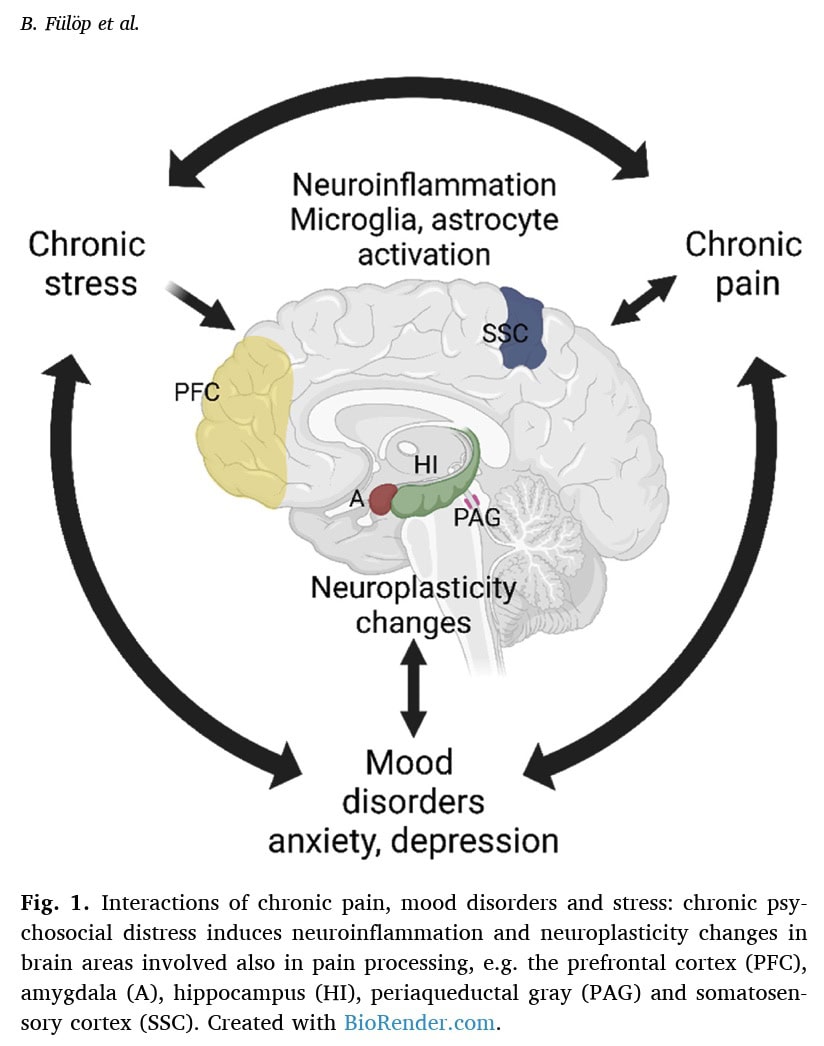
Alterations in brain networks and synaptic links are observed. In fibromyalgia patients, functional connectivity within salience and default mode networks is increased, correlating with pain intensity and catastrophizing. Animal models also show deteriorated salience network connectivity and altered default mode network activation in response to chronic stress.
- Shared mechanisms: Both chronic pain and depression are suggested to induce neuroinflammation via glia-neuron interactions and neuroplasticity alterations, making treatment more challenging. This further emphasizes the stress-pain connection.
Potential Therapeutic Targets: The review points to several areas for future drug development, including:
- Autoimmunity: Autoantibodies from fibromyalgia patients were shown to induce pain symptoms in mice.
- Neurotrophic Factors: While NGF levels were lower and BDNF higher in fibromyalgia patients, blocking BDNF signaling prevented hyperalgesia in some animal models, suggesting a complex role.
- Inflammatory Mediators: Targeting cytokines like IL-1 and the fractalkine receptor (CX3CR1) pathway, which mediates IL-1 release from microglia, shows promise in animal models.
In essence, the paper concludes that stress, pain, and mood disorders form a vicious circle, sharing common brain structures, mechanisms, and mediators, with neuroinflammation and neuroplasticity being key players in the stress-pain connection.
Questions and thoughts
This review provides a valuable overview, but as physiotherapists, several questions and critical thoughts come to mind regarding the stress-pain connection.
The paper strongly states that “Chronic psychosocial distress is known to be the only etiological and/or aggravating factor” for chronic primary pain”. While positive correlations are found between stress levels and pain, and stress-induced tasks decrease pain thresholds, the clinical data presented here are largely correlational. It would be more accurate to say it’s a major contributing factor. The word “only” might be an overstatement without a systematic review of all other potential contributing factors and a demonstration that they play no etiological role. This kind of definitive statement in a review should ideally be supported by an exhaustive literature search and critical evaluation of all relevant literature, not just the studies that support this particular perspective on the stress-pain connection.
Animal models do show stress-induced pain, which strengthens the causal link, but how well does this translate to the complex human experience where multiple factors often converge? Stress is a multifactorial and multidimensional experience that may not be exactly similar between humans and animals, and not even between humans.
The review mentions various chronic stressors in animal models (swim, cold, sound, restraint). While these induce hyperalgesia, are all types of stress equally relevant or impactful for chronic pain, especially fibromyalgia? The paper notes that “chronic variable mild stress… is not suitable to investigate stress-induced pain mechanisms,” which is an important nuance. What specific aspects of psychosocial distress are most relevant in humans? Is it the type of stress, its duration, or the individual’s coping capacity that matters most?
The authors acknowledge that “no animal models are suitable for reflecting all aspects of the complex symptomatology of human diseases.” This is a crucial point. While animal models provide insights into cellular and molecular processes, the subjective experience of chronic pain, pain catastrophizing, and the impact on daily function in humans are difficult to replicate. How can findings from animal models, especially regarding specific molecular targets, be most effectively translated into clinical practice for complex conditions like FM? This highlights challenges in understanding the stress-pain connection across species.
The paper mentions psychotherapy might be effective “on a long-term after months, but these treatments usually start together with medications at the earlier stages; further suggesting the complex treatment paradigm: targeting the psychosocial component of these diseases.” While the paper focuses on molecular mechanisms, this phrasing might downplay the significant and often immediate impact of psychosocial interventions on coping, pain perception, and quality of life. Is the “minor effect” statement based purely on pain reduction, or does it consider broader patient-centered outcomes?
Talk nerdy to me
While this publication answers several questions, we must acknowledge that it is not a systematic review and that it may be biased. For example, psychosocial distress was named by the researchers as the “only etiological and/or aggravating factor for chronic primary pain conditions” like fibromyalgia. They highlight the importance of the stress-pain connection, and they reference 3 articles to endorse this statement. While psychosocial distress plays an important role in chronic pain, none of the three referenced studies indicates psychosocial distress as the sole factor contributing to the pain experienced.
- In fact, the reference of Barke et al. 2019 is a citation not leading to a peer-reviewed paper.
- The reference of Nicholas et al. 2019 emphasizes the biopsychosocial model in explaining chronic pain and acknowledges psychosocial factors like distress, but also mentions neurobiological and behavioral factors to be at play.
- The Scholz et al. (2019) reference reinforces the multidimensional nature of chronic pain and lists various potential contributors: nervous system dysfunction, emotional distress, social context, but again, does not isolate chronic psychosocial distress as the only cause. Even more, this reference is about chronic neuropathic pain, and not about chronic widespread pain such as fibromyalgia.
Thus, there is no indication that psychosocial distress is the sole factor, although the current paper says so. This may indicate that the authors oversimplified the role of psychosocial distress to align with their own research and hypotheses, which is called framing.
As this article was intended to be a short review article, it relies on the quality and robustness of the primary research it summarizes. But you must be aware that no systematic search for literature was held. The study itself also doesn’t present new data. Therefore, its conclusions are as strong as the evidence base it draws from, but the non-systematic way the authors searched for literature raises the risk of biases. While the authors have done a good job of citing a wide range of studies, individual study limitations (e.g., sample size, specific animal models chosen, methodology of stress induction, outcome measures) influence the overall conclusions, and as no rating of the evidence took place, the certainty of the synthesized evidence remains questionable and low.
Take-home messages
Chronic psychosocial distress is not just a secondary issue; it’s a fundamental factor in the development and perpetuation of chronic primary pain. Always explore and acknowledge the role of stress, anxiety, and depression in your patients’ pain experience. Your assessment should go beyond purely physical factors. Incorporate questions about stress levels, coping mechanisms, mood, and social support. This provides a more complete picture of the patient’s condition and the stress-pain connection.
Educate your patients about the brain-body connection and how stress can influence pain through mechanisms like neuroinflammation and changes in brain wiring (neuroplasticity). This can empower them to understand their pain better and engage in self-management strategies.
While the review focuses on molecular targets, remember the value of psychosocial interventions. Techniques like mindfulness, relaxation exercises, and cognitive behavioral approaches (which can be integrated into physiotherapy) can directly address the psychosocial distress contributing to pain. Exercise is a cornerstone of physiotherapy for chronic pain. While this review doesn’t detail the mechanisms, exercise is known to have anti-inflammatory effects and can influence neuroplasticity. Encourage regular, graded exercise, explaining its potential benefits in counteracting the negative effects of stress.
A multidisciplinary approach is often necessary to address all facets of the patient’s condition effectively, especially when dealing with the stress-pain connection. Recognize that each patient’s experience of chronic pain and psychosocial distress is unique. Tailor your interventions to the individual’s specific needs, stressors, and coping abilities.
Reference
How Nutrition Can Be a Crucial Factor for Central Sensitisation - Video Lecture
Watch this FREE video lecture on Nutrition & Central Sensitisation by Europe’s #1 chronic pain researcher Jo Nijs. Which food patients should avoid will probably surprise you!

