Assessing Sensorimotor Dysfunction Following ACL Injury

Introduction
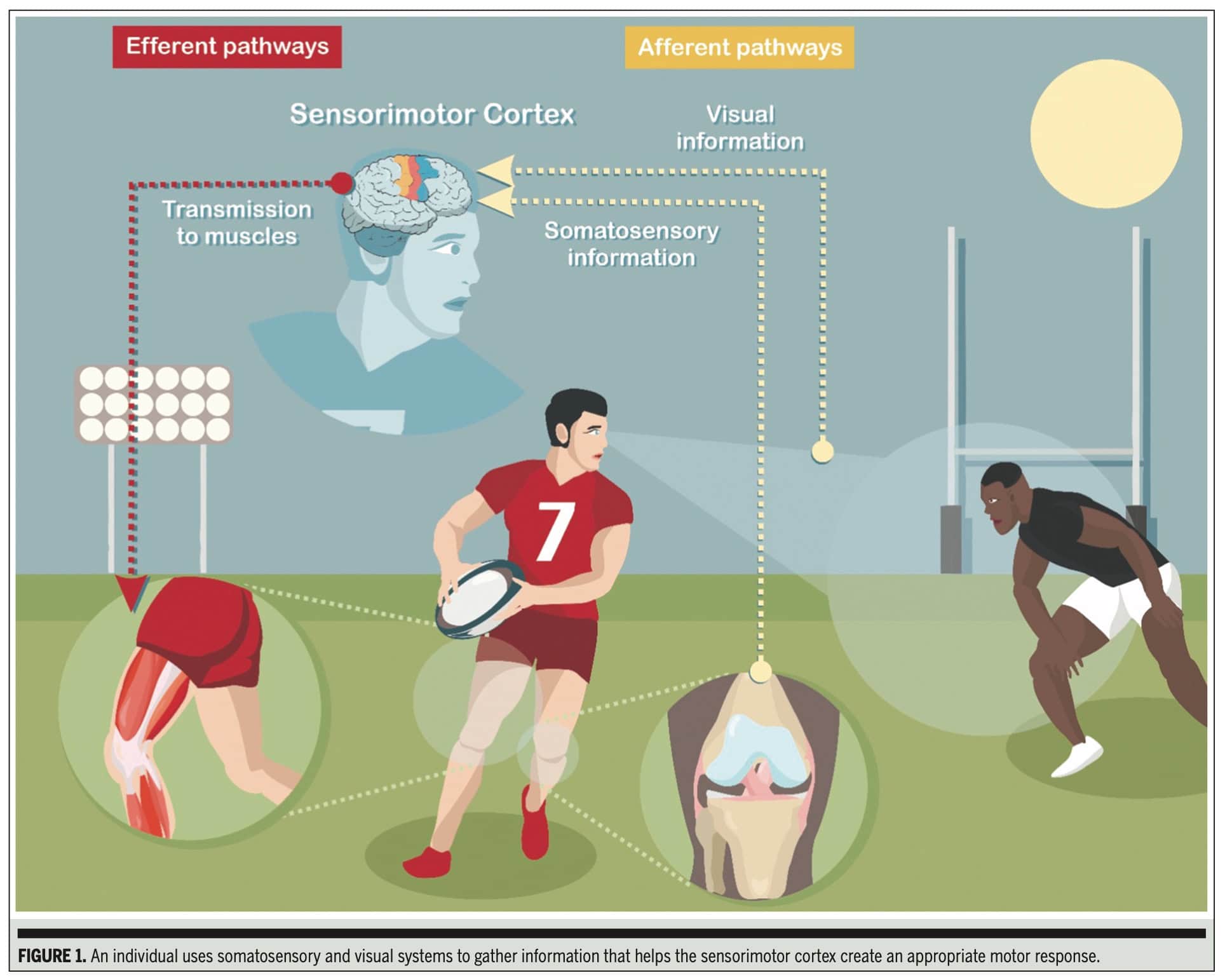
Injuries to the musculoskeletal system lead to disturbances in the sensorimotor system. The sensorimotor system integrates afferent information from the periphery, which is then processed in the sensorimotor cortex, whereafter an efferent (motor) action is executed. People sustaining injuries to the anterior cruciate ligament (ACL) are primarily affected in the knee stability domain, as the torn ACL is a crucial restraint against excessive tibial anterior translation, internal rotation, and knee valgus. What becomes more clear is the important sensory function of the ACL. Afferent information is sent from the ACL to the sensorimotor cortex, where it is integrated with other stimuli from sensory systems, such as the visual and vestibular systems. This integration enables the planning and execution of a motor action. One of the major frustrations in ACL research and rehabilitation is the high re-injury risk. More and more effort is put into finding the hows and whys of this high risk. This research review outlines a clinical commentary written by Vitharana et al. (2025), aiming to increase knowledge about sensorimotor dysfunction following ACL injury.
Methods
This paper is written as a clinical commentary that includes a systematic approach to reviewing the literature to inform clinical practice. It is, however, not a formal systematic review with a meta-analysis of primary studies, which adheres to more rigorous statistical and methodological criteria.
The authors aim to answer two key questions:
- What dysfunction occurs within the sensorimotor system following ACL injury?
- How can clinicians assess it?
They aimed to examine the changes that occur across the afferent (sensory input), efferent (motor output), and central processing pathways after an ACL injury. A key focus of their examination was identifying assessment methods that are practically accessible to clinicians, recognizing the limitations of specialized equipment in typical clinical settings.
Their review specifically delved into:
- Somatosensory system changes: Examining alterations in proprioception, pain, and effusion following ACL injury.
- Visual system changes: Investigating how visual-motor reliance and processing ability are affected.
- Efferent system changes: Exploring the impact on muscle strength and voluntary activation, particularly in the quadriceps.
By reviewing studies related to these areas, the authors sought to synthesize the current understanding of sensorimotor dysfunction and identify practical, evidence-based ways for clinicians to assess these deficits.
Results
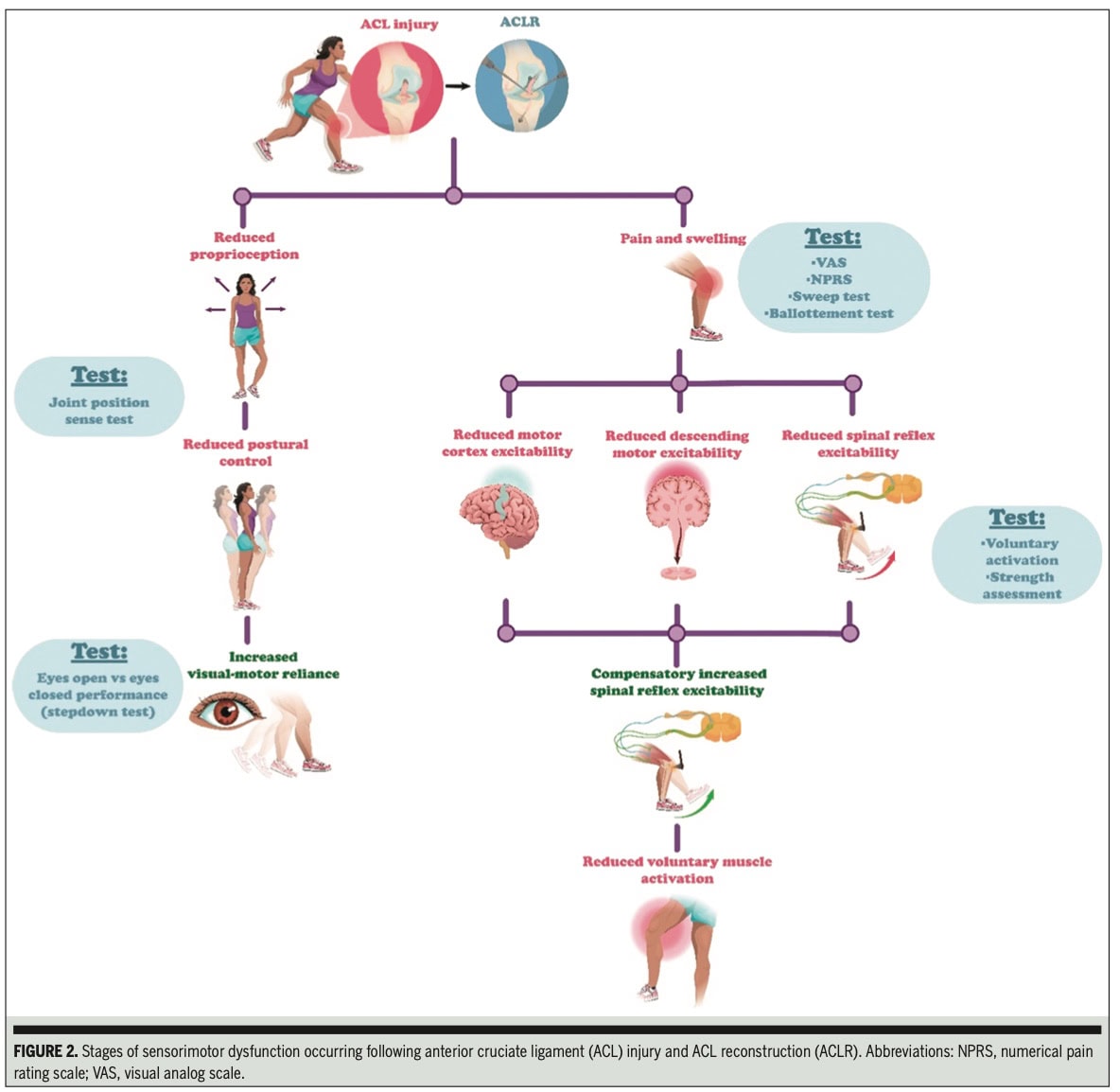
The paper confirms that following an ACL injury, dysfunction is widespread across the sensorimotor system, impacting afferent pathways (somatosensory and visual systems), efferent pathways, and central processing.
Specifically:
- Afferent Pathway Dysfunction:
- Somatosensory System: The authors’ review of the literature indicated increased pain and swelling, increased central cortical processing (though this is difficult to assess practically), and a consistent finding of reduced proprioception, particularly in knee Joint Position Sense (JPS). This leads to a greater error in body position awareness.
- Visual System: The authors found evidence of increased visual-motor reliance and central cortical processing. This suggests that individuals with ACL injuries may rely more heavily on vision for movement, potentially increasing cognitive demand and reducing reaction time.
- Efferent Pathway Dysfunction: The authors pointed to reduced excitability of the motor cortex and descending motor pathways, as well as altered spinal reflexive excitability. These changes manifest as reduced muscle activation, impaired coordination, and persistent muscle weakness, especially in the quadriceps.
The authors’ review of the literature led them to conclude that assessing proprioception, pain, swelling, visual-motor reliance, visual-motor processing ability, muscle strength, and voluntary activation are key practical ways to objectify the extent of sensorimotor dysfunction following ACL injury.
The clinical commentary then outlines the details of how to perform these assessments:
Afferent Pathway Dysfunction Assessment
For somatosensory assessment, the paper emphasizes proprioception, pain, and effusion.
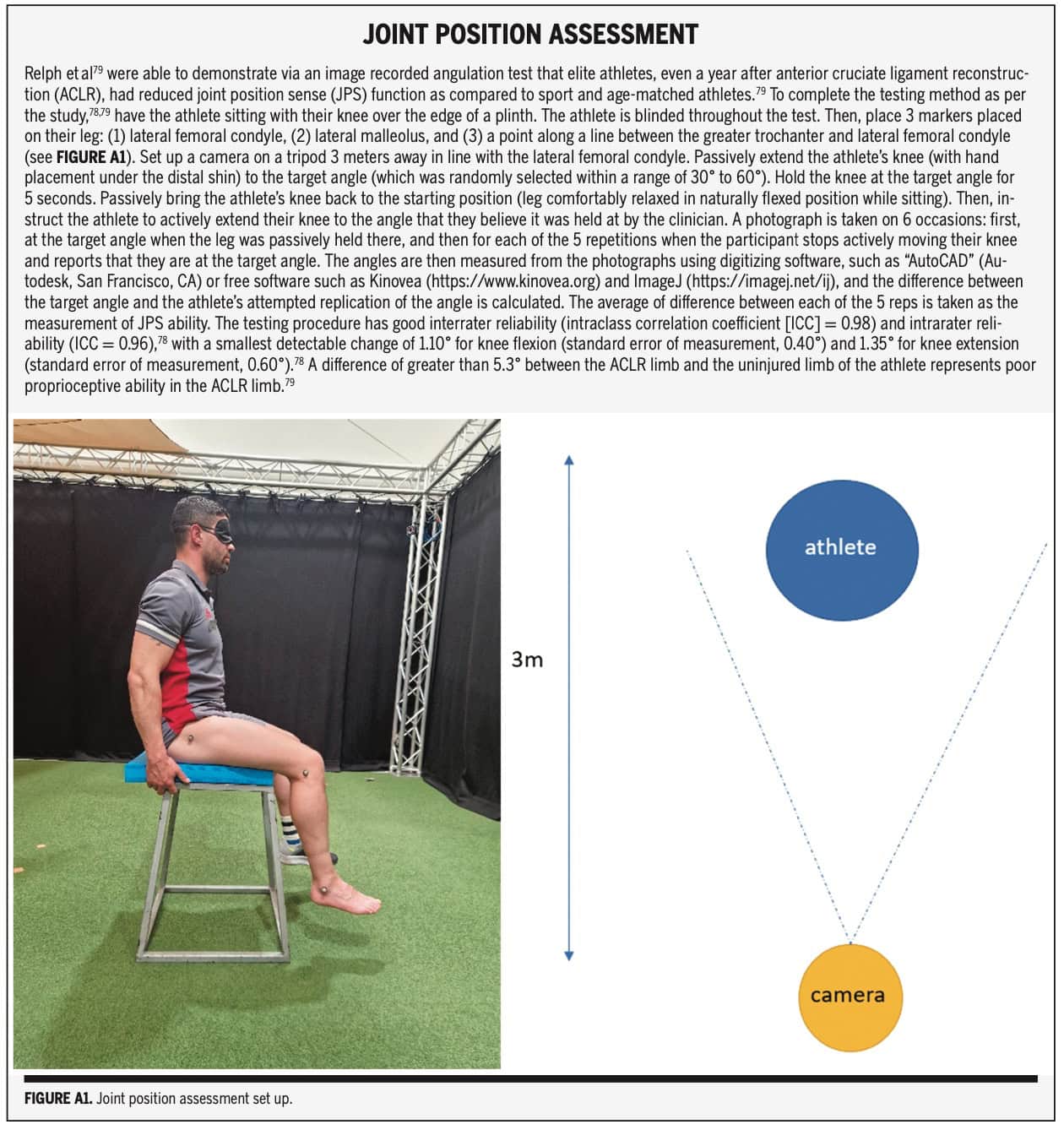
Proprioception encompasses joint position sense, kinesthesia, sense of movement velocity, and sense of force. As the latter three require specialized equipment, the clinical commentary recommends the Joint Position Sense Test to use in clinical practice.
- Procedure: The athlete sits with their knee over the edge of a plinth, blinded. Three markers are placed: on the lateral femoral condyle, lateral malleolus, and a point along the line between the greater trochanter and lateral femoral condyle. A camera is set up 3 meters away, in line with the lateral femoral condyle. The clinician passively extends the knee to a random target angle (30-60 degrees), holds for 5 seconds, and then returns the leg to a relaxed position. The athlete then actively extends their knee to replicate the perceived target angle.
- Data Collection: A photograph is taken at the target angle for each of 5 active replication attempts, or a goniometer can be attached to the lower leg to control the angles. Angles are measured from photos using digitizing software (e.g., Kinovea, ImageJ). The average difference between the target and replicated angles quantifies the proprioceptive ability.
- Interpretation: A difference greater than 5.3° between the ACLR limb and the uninjured limb indicates poor proprioceptive ability in the injured limb, but this was derived from a study including only 10 athletes following ACL reconstruction. The authors recommend reassessing every 4-6 weeks during rehabilitation.
Pain
The authors recommend using the Numerical Pain Rating Scale (NPRS) or Visual Analog Scale (VAS). Changes from 1.4 cm to 2 cm are suggested for musculoskeletal and chronic pain. It is recommended to assess pain every session until it is resolved.
Effusion
The Sweep test and Ballottement test are to be performed for assessing the quantity of effusion around the knee joint. The authors pointed out that effusion should be assessed, like pain, every session until resolved.
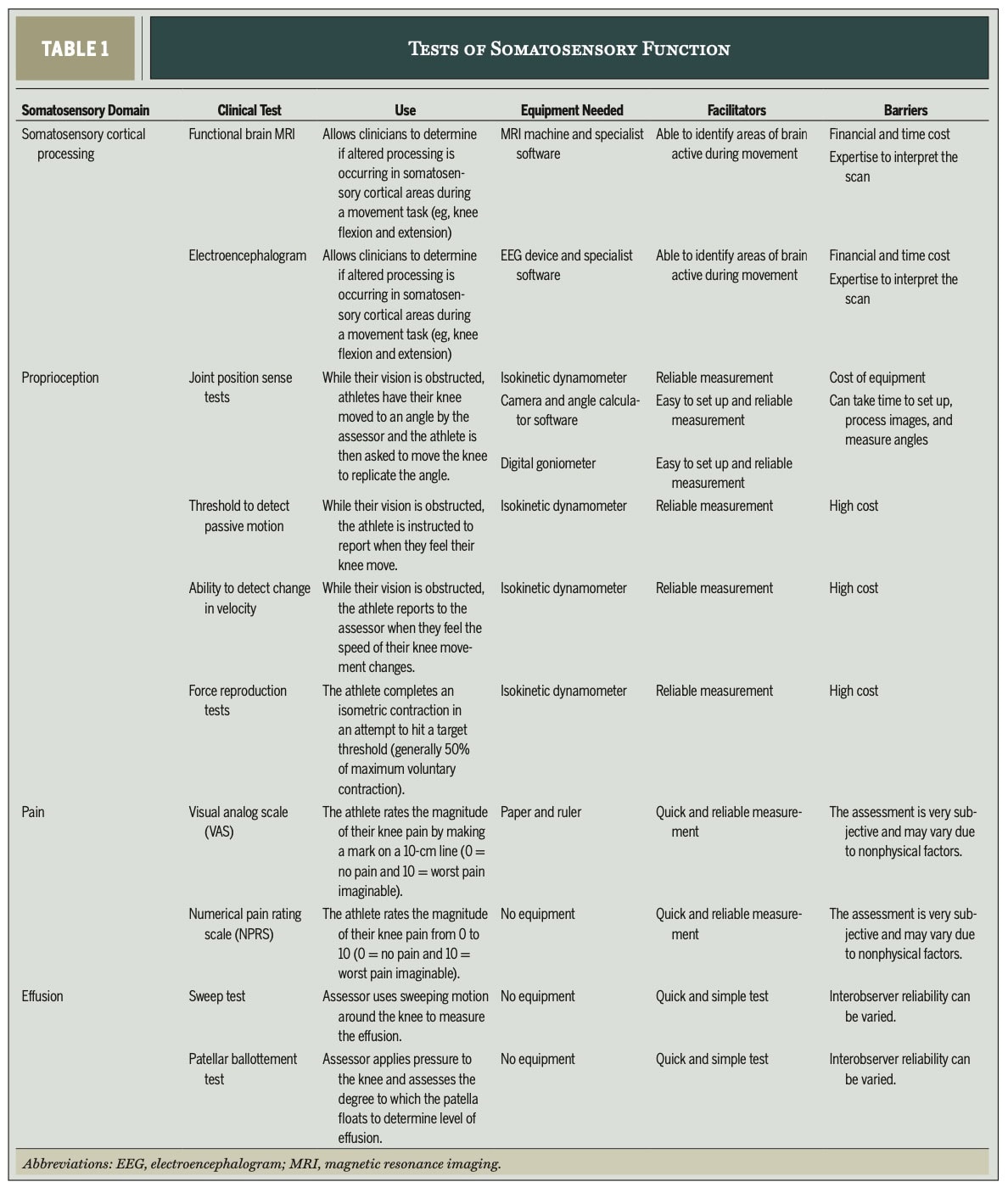
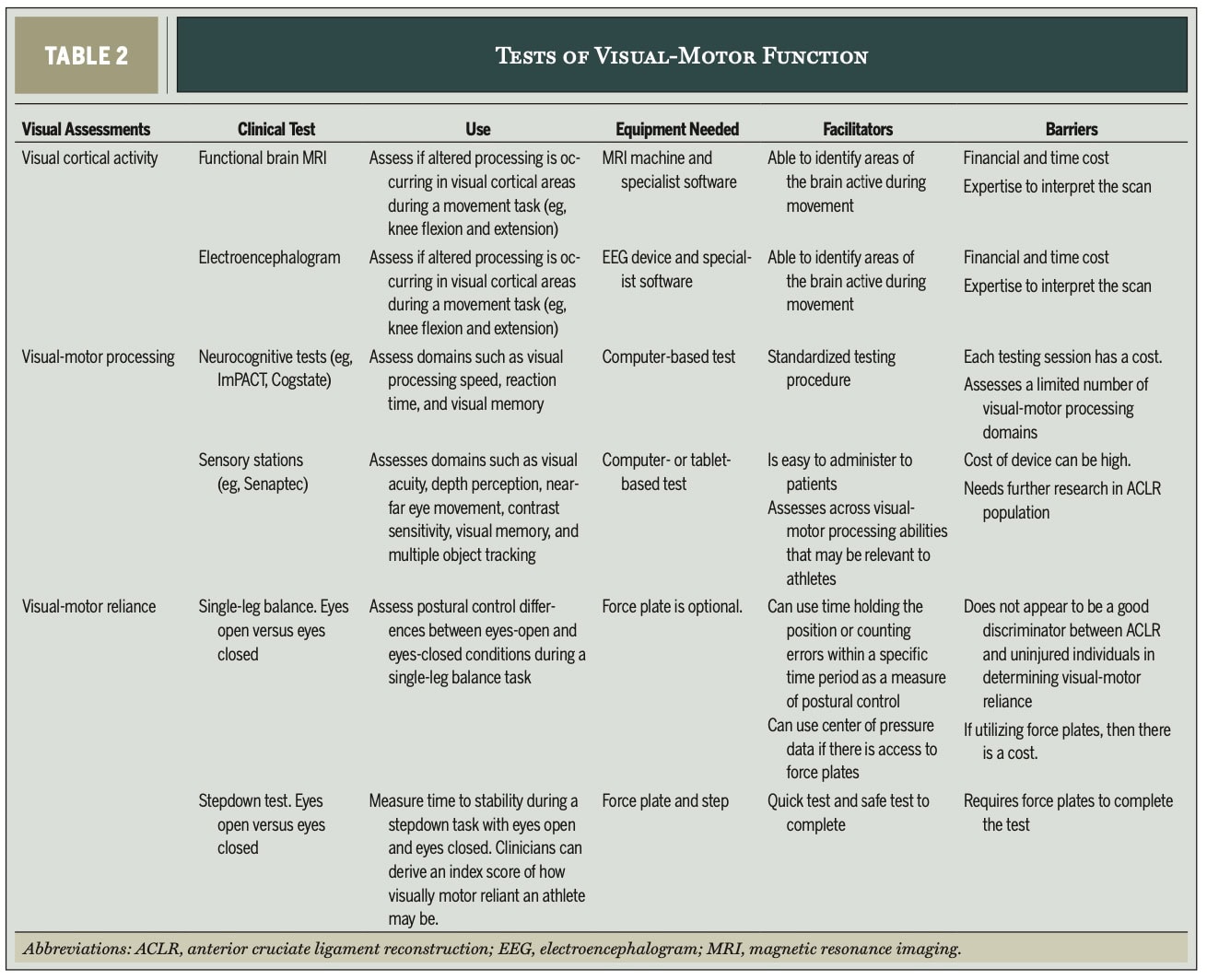
For visual system assessment, the focus is on visual-motor reliance and processing ability:
Visual-Motor Reliance (via Balance Tests)
The paper adapts a 20-cm Stepdown Test with eyes open vs. eyes closed. With the athlete barefoot and standing on a 20-cm step with his hands on his hips, he steps onto a force plate with one leg, aiming for quick stability and maintaining landing posture for 20 seconds. Three trials are done for each leg, both with eyes open and then repeated with a blindfold or with the eyes closed.
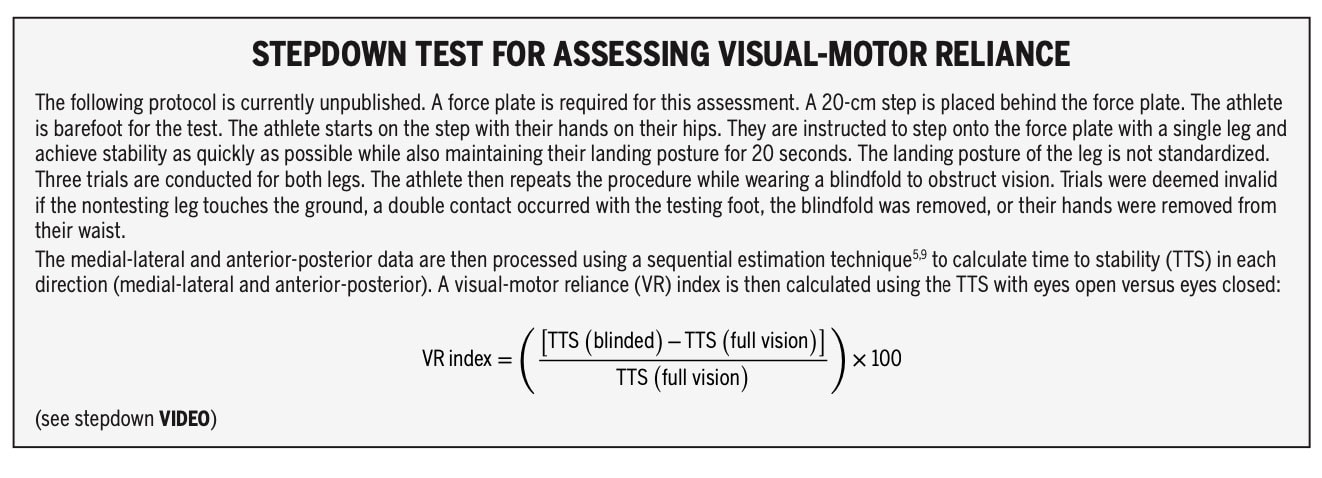
- The time to stability (TTS) is calculated for medial-lateral and anterior-posterior directions.
- A Visual-Motor Reliance (VR) index is calculated by using the formula depicted above. It was shown that healthy athletes improve TTS by 17% with eyes closed. If an athlete’s TTS worsens with eyes closed, it indicates visual reliance.
- Subjective assessment of postural control can be used if force plates are unavailable. In the subjective assessment, you look for frontal plane control, trunk sway, hip movement, knee adduction and foot pronation and supination. It is important to reassess every 6 weeks.
Visual-Motor Processing Ability
The authors recommend the use of computer-based neurocognitive tests (e.g., ImPACT, Cogstate) or “Sensory Stations” (e.g., Senaptec). These assess domains like visual processing speed, reaction time, visual memory, visual acuity, depth perception, near-far eye movement, contrast sensitivity, and multiple object tracking.
- Practicality: Computer-based tests are relatively low-cost and easy to administer. Sensory stations offer varied tasks and immediate percentile scores.
- Caution: Reliability in ACLR populations and normative values are still areas needing more research. Baseline information is crucial, but often unavailable since the athlete will likely see you after the injury has already happened and not preventively.
Efferent System Assessment
For assessing the efferent system, muscle strength and voluntary activation of the quadriceps are recommended. Other domains, such as motor cortical activity, descending motor pathways, and spinal reflexes, are also part of the efferent motor pathway, but require specialized equipment frequently unavailable to the clinician.
Muscle Strength
The use of repetition maximum testing (using 1, 3, or 5 RM), handheld dynamometry, or isokinetic dynamometry is recommended.
- Isokinetic Dynamometry is considered the gold standard, but requires specialized equipment not always available. With the athlete in a seated position with torso and limb fixed, three sets of five concentric knee flexion/extension repetitions are performed, with the first set being submaximal, and a one-minute rest between sets. The range of motion is from 0 to 100° at 60°/s. The peak torque for the quadriceps and hamstrings is measured, with target values of 240-270% body mass for quadriceps and 150-160% body mass for hamstrings.
- Handheld Dynamometry offers a cost-effective alternative for assessing isometric quadriceps strength using nonelastic straps, though it cannot identify range-specific deficits.
- Strength assessments using these methods should be completed every 6-8 weeks.
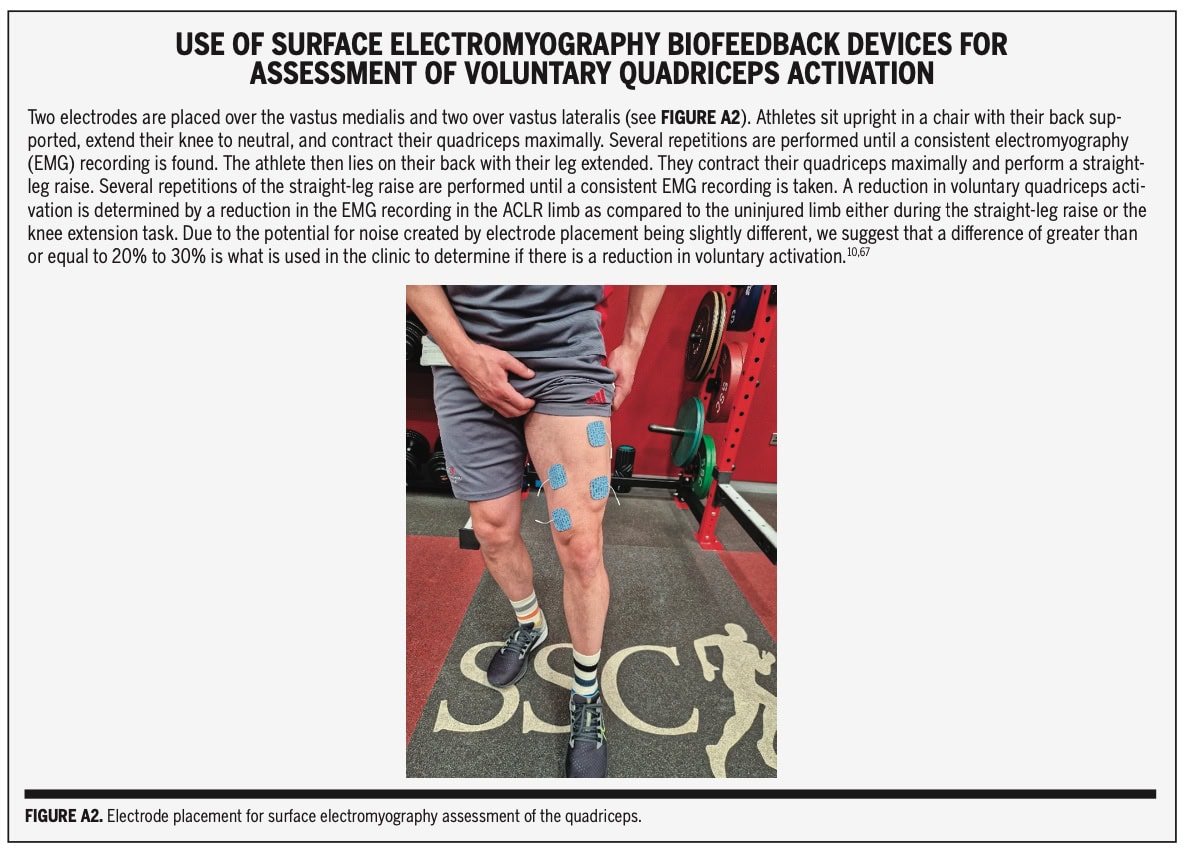
Voluntary Activation of the Quadriceps
The use of surface electromyography (EMG) biofeedback devices is advocated
For assessing voluntary activation of the quadriceps, two electrodes are placed over the vastus medialis and two over the vastus lateralis. The athlete sits upright with the knee extended to neutral and performs a maximal quadriceps contraction, repeating until consistent EMG is recorded. Subsequently, lying on their back with the leg extended, they perform a maximal quadriceps contraction with a straight-leg raise, also repeated until consistent EMG is recorded. A reduction in EMG recording of 20-30% or more in the ACLR limb compared to the uninjured limb is interpreted as indicating reduced voluntary activation. This assessment should be performed every two weeks until no significant difference is observed.
Questions and thoughts
While the authors emphasize practical tools, the limitations of those tools compared to the “gold standard” equipment (like isokinetic dynamometers for strength or MRI for cortical activity) are acknowledged. How much sensitivity are we losing with the more practical tests? And at what point does the practical test become too insensitive to reliably detect meaningful dysfunction? For example, is a subjective assessment of postural control truly sufficient if force plates aren’t available, or does it miss subtle but important deficits? Video recordings in slow motion may help the examiner to note more subtle differences, but can be prone to misinterpretation.
The paper notes that more research is needed for visual-motor reliance and processing tests to identify normative values and determine if they are related to reinjury. This is a crucial gap. Without clear normative data for an ACL-injured population and a demonstrated link to reinjury, how confident can we be in using these assessments to guide return-to-sport decisions? It seems like we’re still in the early stages for some of these visual assessments.
The paper focuses on ACL injury and its impact on the sensorimotor system, primarily around the knee. However, sensorimotor dysfunction often manifests more globally and can affect more than just the knee joint. While the paper highlights changes in central processing, it doesn’t delve into how these might impact other joints or global movement patterns.
Talk nerdy to me
Although the researchers have put tremendous effort into writing a clinically applicable statement, you should be aware that this information was not derived from a systematic review. Rather, it serves as an expert opinion publication, which is, however, very informative to the reader as it is written for easy implementation into clinical practice. As a clinical commentary, the paper itself is a lower level of evidence. Its strength lies in synthesizing existing research and providing clinical applications.
Reliability of the assessments
The paper cites ICCs of 0.96-0.98 for inter- and intra-rater reliability of the image-recorded angulation Joint Position Sense test. These are excellent reliability values, indicating high consistency. The smallest detectable change (SDC) of 1.10° for knee flexion and 1.35° for knee extension is also provided, which is crucial for interpreting real change versus measurement error. The interpretation of a >5.3° difference between limbs as “poor proprioceptive ability” is based on a specific study of 10 elite athletes. While this provides a benchmark, the generalizability to a broader ACLR population might be limited due to the small sample size and elite athlete focus of the original study.
The paper notes “good interobserver agreement” for the Sweep and Ballottement tests. While this is positive, it lacks specific statistical measures (e.g., Kappa coefficients, specific ICCs) that would provide a more precise quantification of agreement. This is a common limitation for clinical examination tests.
The authors report “good reliability (ICCs=0.71-0.96)” for their adapted stepdown task. This is a broad range, and specific ICCs for the VR index would be more informative. The interpretation that “healthy athletes improved their time to stability time by 17% with eyes closed” and the subsequent implication of visual reliance if an athlete’s TTS worsens with eyes closed, sets a clear benchmark. However, the data for healthy athletes is “unpublished,” which is a methodological weakness, as it hasn’t undergone peer review.
Visual-Motor Processing Ability (Neurocognitive Tests, Sensory Stations): Reliability is stated as “good” for uninjured athletes, but a critical caveat is made: “no study has examined their reliability in the ACLR population”. This is a significant limitation for using these tests specifically in ACLR rehabilitation, as reliability can differ in injured populations. The lack of normative values and established links to reinjury risk are also highlighted as areas needing more research.
Isokinetic Dynamometry: Described as the “gold standard” with “high reliability (ICC=0.74-0.93)” [1, p. 9]. This range is generally considered good. The target values (quadriceps 240-270% body mass, hamstrings 150-160% body mass) are provided.
Handheld Dynamometry: Stated as “reliable and valid in measuring isometric quadriceps strength when using nonelastic straps”. This provides confidence in its use as a practical alternative.
Voluntary Activation (Surface EMG): The paper suggests a “difference of greater than or equal to 20% to 30%” as clinically relevant based on their references. This provides a practical threshold for interpreting EMG findings.
Risk of Bias
As a clinical commentary, a formal risk of bias assessment doesn’t apply to the paper itself. However, the authors’ selection of assessment methods is driven by their clinical practice, which introduces potential for selection bias. While they aim for evidence-based methods, the depth of evidence for each suggested test varies, as noted above.
The strength of this clinical commentary lies in its focus on practical clinical application. The authors have done a commendable job of synthesizing research to provide actionable assessment strategies. However, it’s important for the reader to recognize that this practical focus sometimes comes at the expense of the rigorous statistical analysis and adherence to strict evidence-based hierarchies found in systematic reviews or large-scale primary studies. The commentary serves as a valuable bridge between research and practice, but it also highlights the ongoing need for more high-quality research, particularly on the reliability and validity of practical tests in the ACLR population and their direct link to meaningful outcomes like reinjury risk.
Take-home messages
It has long been understood that ACL injuries impact knee stability, but what’s become increasingly clear is the broader effect on the sensorimotor system, influencing movement planning and execution.
Sensorimotor dysfunction following ACL injury is multifaceted. It affects not just the knee joint, but the entire afferent (somatosensory, visual) and efferent systems, including central processing. We need to look beyond just strength and stability. This paper outlines the recommended assessments for clinical practice. While specialized equipment exists, clinicians can still assess key aspects of sensorimotor dysfunction using readily available tools like the Joint Position Sense test, pain/effusion scales, adapted step-down tests for visual reliance, and handheld dynamometry or repetition maximum testing for strength.
This paper lays the groundwork for understanding what and how to assess. Stay tuned for Part 2 to learn how to rehabilitate these dysfunctions!
Reference
WHAT TO LOOK FOR TO PREVENT HAMSTRING, CALF & QUADRICEPS INJURIES
Whether you’re working with high-level or amateur athletes you don’t want to miss these risk factors which could expose them to higher risk of injury. This webinar will enable you to spot those risk factors to work on them during rehab!

