Rehabilitation Interventions for CRPS: Investigating the Effectiveness on Pain and Disability

Introduction
Complex regional pain syndrome, abbreviated CRPS, is a painful, chronic, and debilitating condition where the autonomic nervous system and neuro-inflammatory pathways get overly activated. It mostly arises after surgery or after sustaining a traumatic event such as a wrist fracture. CRPS can be subclassified into two types: CRPS-1 and CRPS-2, where the latter shows signs of (discrete) nerve lesions. In both cases, the signs and symptoms are way out of proportion to the underlying injury or inciting event.
Many rehabilitation interventions for CRPS have been proposed, but their effectiveness remains unclear, since existing systematic reviews have either focused too narrowly on specific modalities or have not provided a recent, in-depth critical appraisal and quantitative synthesis of rehabilitation-focused randomized controlled trials (RCTs). Recognizing this need, Shafiee et al. (2023) conducted this systematic review and meta-analysis to consolidate and evaluate the current body of evidence on rehabilitation interventions for CRPS, offering a crucial resource for clinicians.
Methods
To conduct this systematic review and meta-analysis, the researchers performed a thorough literature search across multiple databases, including Embase, Medline, CINAHL, Google Scholar, PEDro, and PsycINFO, from their inception up to November 2021.
Two independent reviewers screened titles and abstracts to identify potentially relevant manuscripts. Subsequently, the full text of these studies was reviewed against specific eligibility criteria. Any disagreements between the reviewers were resolved through discussion with a third author.
Studies were eligible for inclusion when they were randomized controlled trials (RCTs), including adults (18 years or older) who were diagnosed with CRPS-1 or CRPS-2 or Shoulder-Hand Syndrome (SHS), resulting from trauma or neurological conditions like stroke. Interventions in the RCTs could be any non-invasive intervention, but they had to be delivered by a rehabilitation professional (occupational therapist, physiotherapist, or psychologist). The articles had to measure pain severity and/or function/disability outcomes, using recognized and accepted patient-reported outcome measurements.
Studies about pharmacological and surgical interventions, studies on CRPS in children, and non-randomized clinical trials or conference abstracts were excluded.
Two independent researchers extracted data using a standardized form. This included details such as author, year, type of CRPS, number of participants, mean age, intervention and comparison groups, intervention characteristics (e.g., duration, frequency), study results, and main conclusions. Discrepancies were resolved through consultation with a third author.
Qualitative synthesis was used to summarize findings (e.g., mean age, sex, participant numbers, intervention details, and overall RoB). For the meta-analysis, standardized mean differences (SMD) based on Hedges’ g were calculated as a measure of effect size when sufficient numerical data were available. These effect sizes were pooled, and heterogeneity across the RCTs was reported using I-squared values (0-25% low, 26-50% medium, >50% high). A random-effects model was used for high heterogeneity. Hedges’ g benchmarks were used to interpret the magnitude of the effect sizes as trivial (<0.2), small (0.2), medium (0.5), and large (>0.8). A subgroup analysis based on sex was planned if sufficient data existed.
Results
A total of 33 studies were included in the systematic review, published between 1995 and 2021. Not a single study focused on CRPS-2; eight studies were about poststroke CRPS, 16 studies were about upper limb CRPS-1, and nine studies included a mixed etiology of CRPS in either the upper or lower limbs.
The following rehabilitation interventions for CRPS were studied:
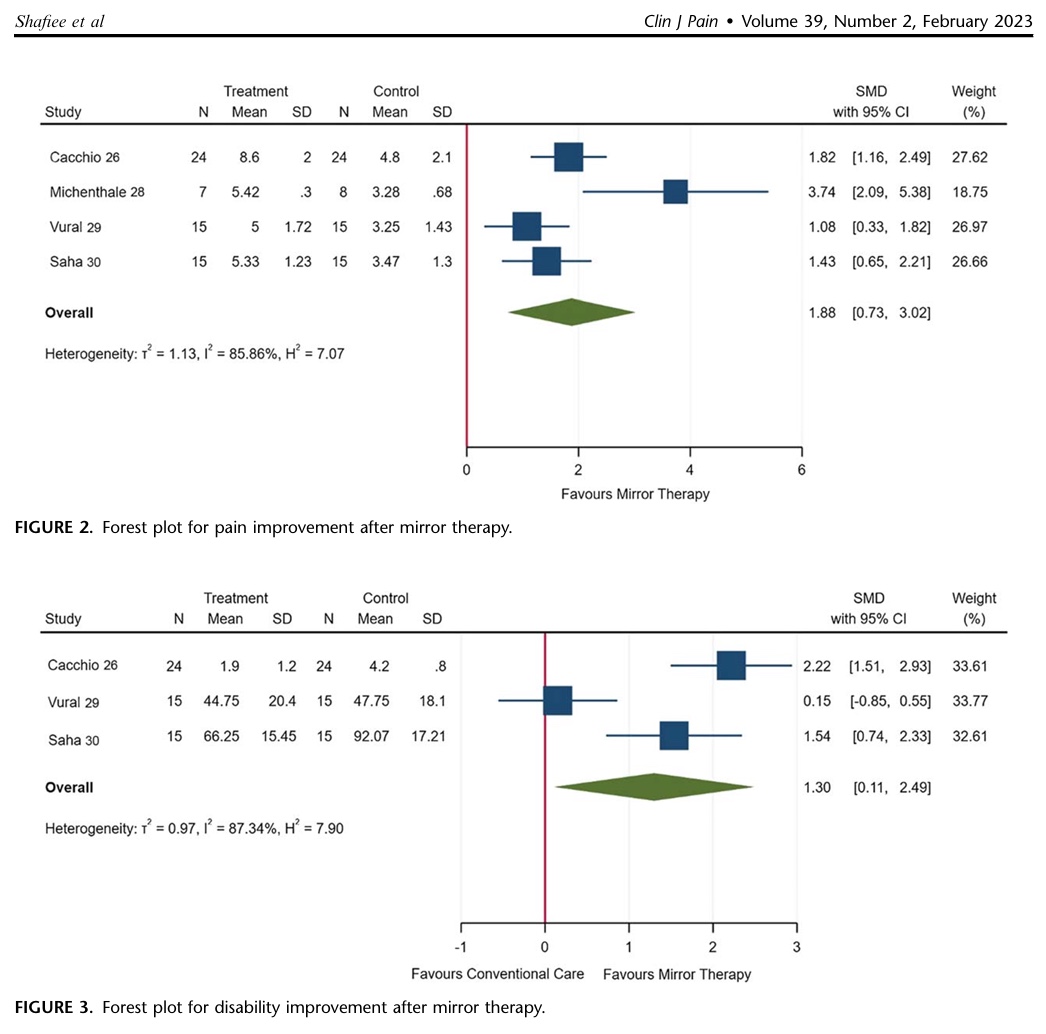
Mirror therapy
Two studies with unclear and two studies with high risk of bias were included in the meta-analysis. These studies evaluated the effectiveness of mirror therapy compared with routine rehabilitation interventions on pain and disability improvement in a total of 155 poststroke and mixed etiology CRPS-1 patients
Pooled Estimates (Meta-analysis):
- Pain: Standardized Mean Difference (SMD) = 1.88 (95% CI: 0.73 to 3.02)
- Disability: SMD = 1.30 (95% CI: 0.11 to 2.49)
The pooled estimate of the SMD for pain and disability improvement when following mirror therapy was 1.88 and 1.30, respectively, indicating large effects. The GRADE analysis initially ranked the RCT evidence as high-quality, but it was downgraded once for sample size, once for inconsistency, and once for methodological limitations and upgraded once for a large effect size. The evidence for mirror therapy was thus concluded to be of low quality, suggesting that mirror therapy as an addition to conventional stroke rehabilitation interventions may result in a large improvement in pain and disability up to 6 months in poststroke CRPS-1 patients.
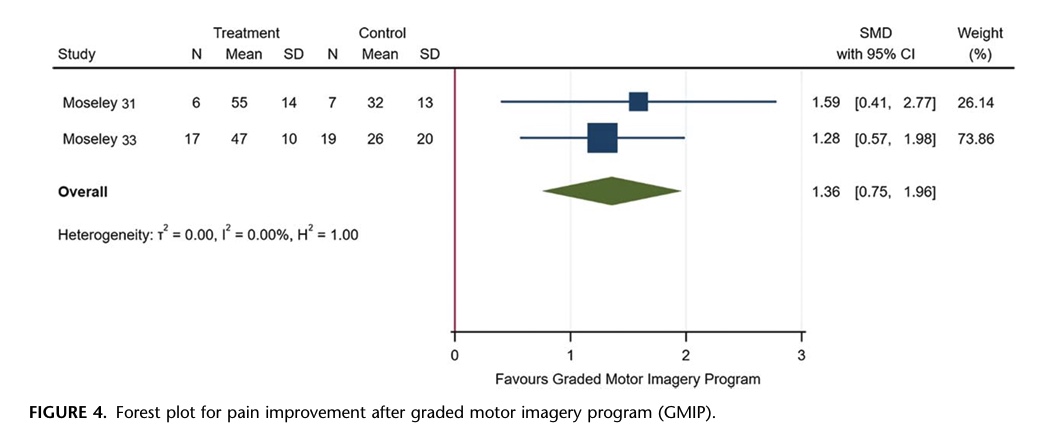
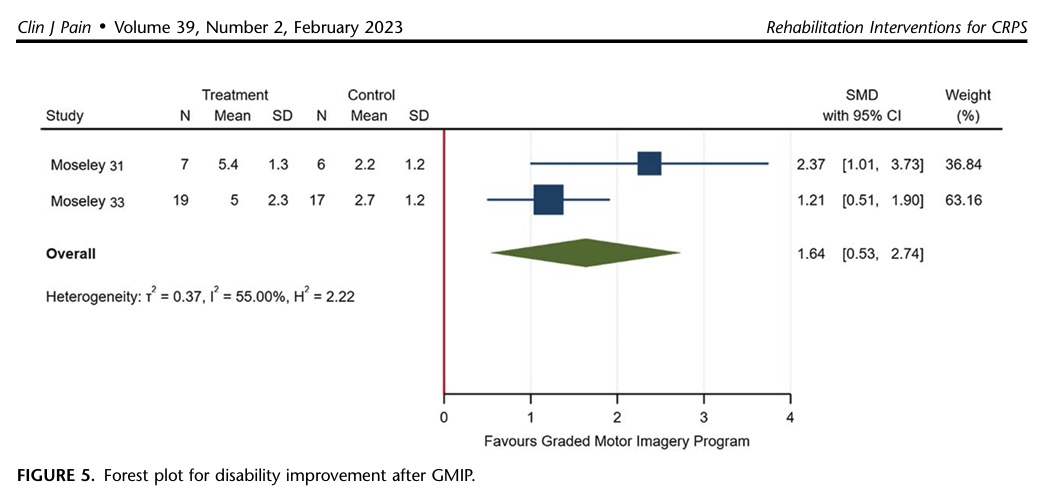
Graded motor imagery
Four studies with risk of bias studies were included in the systematic review, but only 2 were included in the meta-analyses. These studies examined the effectiveness of rehabilitation interventions of graded motor imagery on pain improvement.
Pooled Estimates (Meta-analysis):
- Pain: SMD = 1.36 (95% CI: 0.75 to 1.96)
- Disability: SMD = 1.64 (95% CI: 0.53 to 2.74)
The pooled estimate of the SMD for pain and disability improvement after following a graded motor imagery program was 1.36 and 1.64, respectively, indicating large effects.
The GRADE analysis initially ranked the RCT evidence as high-quality, but it was downgraded twice for sample size, once for inconsistency, and once for methodological limitations and upgraded once for a large effect size. The evidence for mirror therapy was thus concluded to be of low quality, suggesting that mirror therapy as an addition to conventional stroke rehabilitation interventions may result in a large improvement in pain and disability up to 6 months in patients with chronic CRPS following non-complicated wrist fractures and upper limb CRPS-1.
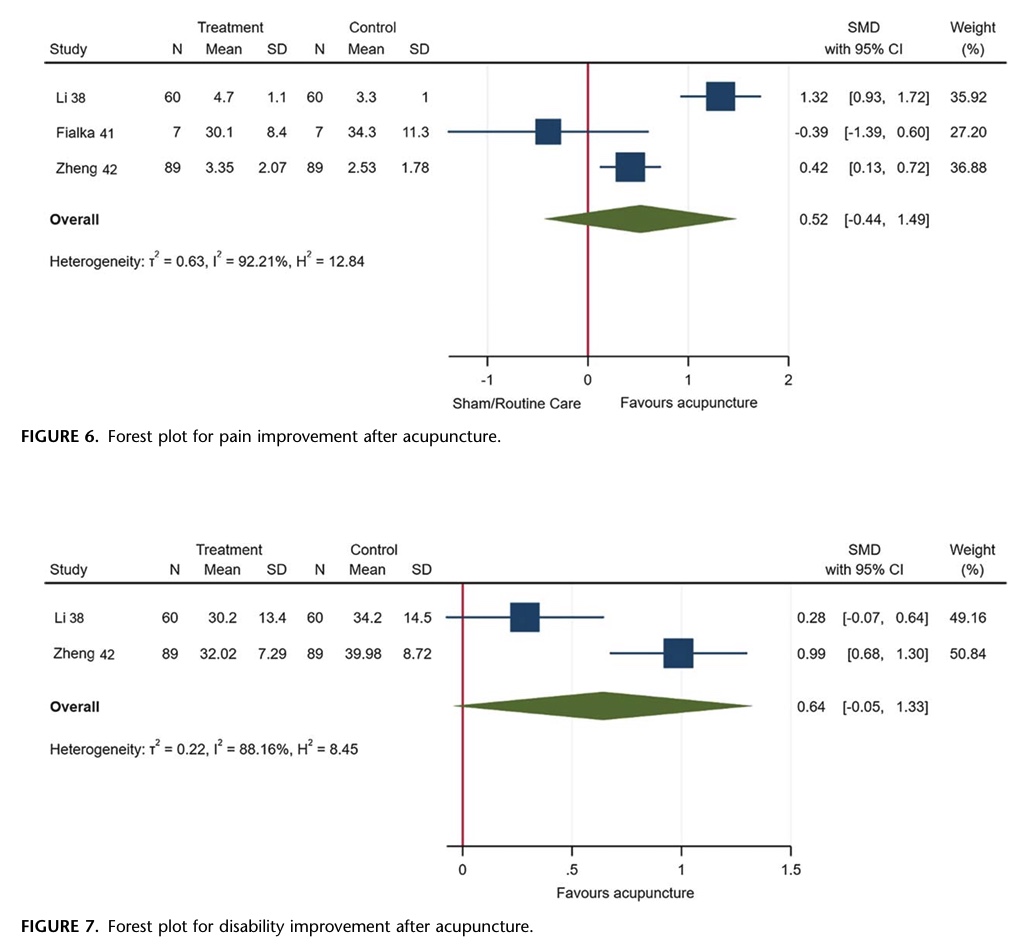
Acupuncture
Four studies, all with high risk of bias, evaluated the effectiveness of acupuncture in pain and disability improvement in 354 CRPS-1 patients. Three studies were included in the meta-analysis for the effect on the outcome pain, while 2 studies were included in the meta-analysis to study the effect on disability improvement.
Pooled Estimates (Meta-analysis):
- Pain: SMD = 0.52 (95% CI: -0.44 to 1.49)
- Disability: SMD = 0.64 (95% CI: -0.05 to 1.33)
The GRADE analysis initially ranked the RCT evidence as high, but downgraded the evidence once for methodological limitations, once for imprecision, and once for inconsistency, resulting in very uncertain effectiveness of acupuncture compared with sham treatment or routine rehabilitation interventions on pain and disability. Further, the confidence intervals indicate the effects crossed 0, and are thus not significant.
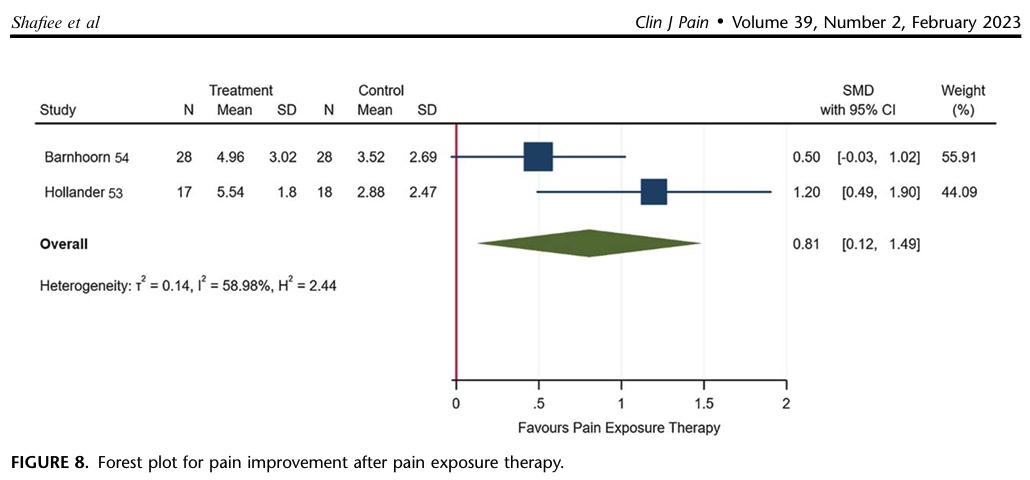
Pain exposure
Two studies, with low and high risk of bias, evaluated the effectiveness of pain exposure in 102 patients with upper and lower limb CRPS-1.
Pooled Estimates (Meta-analysis):
- Pain: SMD = 0.81 (95% CI: 0.12 to 1.49)
- Disability: SMD = 0.59 (95% CI: -0.56 to 1.75)
The GRADE analysis downgraded the high RCT evidence once for sample size, once for methodological limitations, once for imprecision, and once for inconsistency. This resulted in low-quality evidence suggesting that pain exposure treatment may result in a large improvement in pain up to 6-month follow-up. Regarding disability, the evidence is very uncertain about the effect of pain exposure treatment.
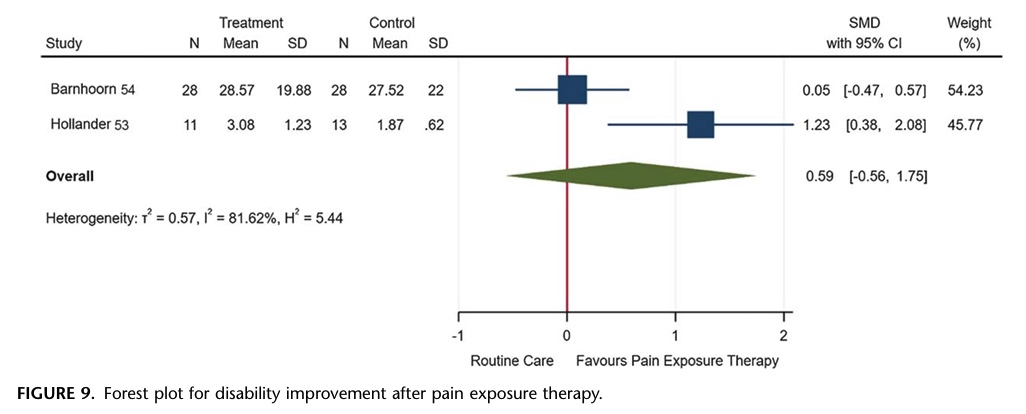
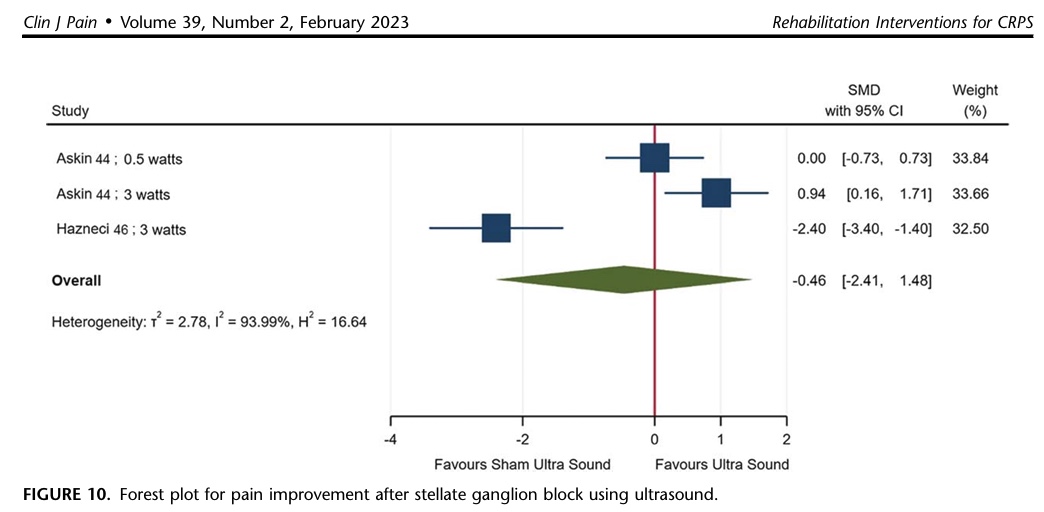
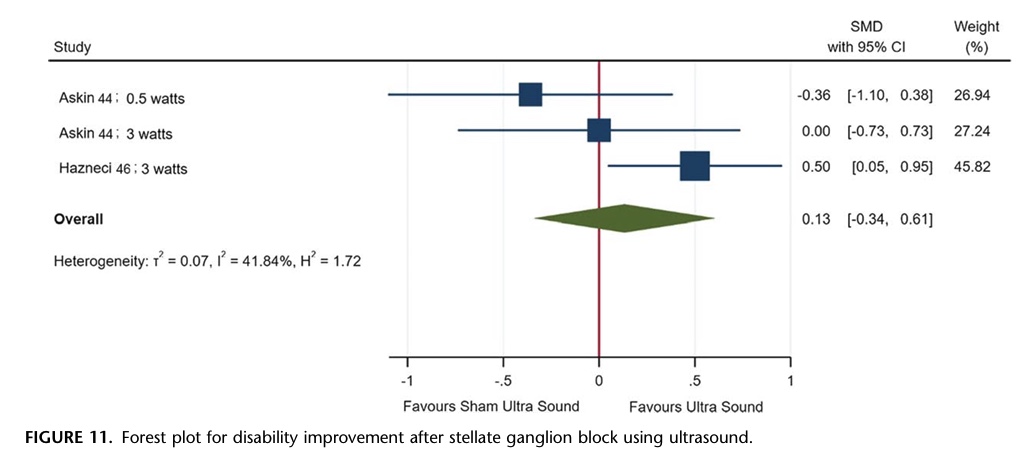
Ultrasound targeting the stellate ganglion
This intervention was studied in 3 RCTs, one with high and two with unclear risk of bias. A total sample of 100 participants with upper limb CRPS-1 were studied by these RCTs.
Pooled Estimates (Meta-analysis):
- Pain: SMD = 0.46 (95% CI: -2.41 to 1.48)
- Disability: SMD = 0.13 (95% CI: -2.41 to 1.48)
The high RCT evidence was downgraded once for methodological limitations, once for imprecision, and once for inconsistency. This resulted in the evidence being very uncertain about the effect of ultrasound of the stellate ganglion compared with placebo or TENS on pain and disability.
The effectiveness of fluidotherapy and Transcutaneous Electrical Nerve Stimulation (TENS) could not be investigated by a meta-analysis due to too much heterogeneity between the studies in terms of dosage differences. Other included studies investigated the following rehabilitation interventions for CRPS as an addition to conventional physiotherapy, but could not be meta-analysed due to insufficient data available for pooling:
- Manual therapy
- Occupational therapy
- Physiotherapy added to conventional occupational therapy
- Aerobic exercise
- Psychological interventions
- Graded exposure
- Laser therapy
Questions and thoughts
Since the included studies covered a wide date range, from 1995 to 2021, various diagnostic criteria were used to define CRPS. The diagnostic criteria for CRPS itself have also shifted throughout the years. Over the years, more and more research around CRPS emerged, and this led to changing definitions and diagnostic criteria. It evolved from an unknown condition that was observed during the American Civil War and described as causalgia in the 19th Century. In the 20th Century, the term reflex sympathetic dystrophy was used to describe similar cases as observed earlier. Then, in the late 20th Century, the International Association for the Study of Pain (IASP) named this condition as we know it today. But as the diagnostic criteria for CRPS, as proposed by the IASP, were of low specificity, in 2010, a new set of criteria, known as the Budapest Criteria, was proposed and validated.
As diagnostic labels have shifted from reflex sympathetic dystrophy, Sudeck atrophy, causalgia, reflex neurovascular dystrophy, algodystrophy, or algoneurodystrophy, to complex regional pain syndrome (CRPS), this leads to heterogeneity across studies over the years. New information and research become available, leading to changes in the way clinicians diagnose and treat these conditions. While this is common and part of evidence-based practice, it can lead to problems when studies examining the same topic are analyzed together, as is done in systematic reviews and meta-analyses. Some studies might include patients diagnosed using older criteria, while others have a more modern understanding of the pathology itself. This leads to variations in patient characteristics, symptom severity, and possibly response to treatment. There are ways to overcome this issue, as the authors have tried to analyze subgroups of CRPS and include the I-squared statistic to measure statistical heterogeneity. Yet, we must remain cautious about the conclusions, especially those with high heterogeneity, established by this systematic review.
As expected, statistical heterogeneity was observed in the meta-analysis of the effectiveness of mirror therapy, graded motor imagery (for disability improvement), acupuncture, pain exposure therapy, and ultrasound stellate ganglion block (medium heterogeneity for disability improvement, high heterogeneity for pain improvement for the latter). This will make comparisons difficult, so there is a need for RCTs using the same criteria and treatment protocols to be established, as it will help improve the low sample sizes and ultimately, it will help increase the possibility of conducting subgroup analyses.
The heterogeneity for the analysis of the effectiveness of graded motor imagery on pain improvement was low, due to the meta-analysis including 2 studies by the same authors, likely using the same definitions across their studies. But for disability improvement, the heterogeneity was high. As such, it would be better to highlight the findings of the effectiveness of graded motor imagery for pain improvement, since it was the only rehabilitation intervention for CRPS I that showed low heterogeneity, a large effect size (with the 95% confidence interval ranging from a medium to large effect size). Yet the evidence level got downgraded for sample size issues and methodological limitations. If these issues could be addressed in the future, I suppose that the certainty of the evidence for graded motor imagery will increase, and new knowledge will emerge to help people affected by CRPS I.
One very important rehabilitation intervention for CRPS, yet not mentioned by this study, is patient education and communication! Despite being often overlooked by reviews and RCTs, it should be the most important aspect of your approach! You can give the best exercises, including mirror therapy and graded motor imagery, as backed by this systematic review’s effectiveness findings, but if you don’t take time to explain what is going on in your patient’s body and how to manage the symptoms, they’ll probably give up when they don’t see improvements right away. Inform them about the long duration and stubborn, fluctuating symptomatology. Explain that flare-ups do not necessarily mean that they’ve done too much; rather, their body overreacts. The last thing you would want to create is fear avoidance, where the patient gets trapped in a vicious cycle where they avoid loading the affected tissues.
New for me was the intervention targeted at the stellate ganglion. A quick search got me to understand that blocking this ganglion (using a nerve block) can help reduce the sympathetic output. As a nerve block is considered a surgical approach, this was excluded by the eligibility criteria of the current paper. Apparently, some RCTs looking at the effectiveness of so-called therapeutic ultrasound for blocking the stellate ganglion were included, which is then categorized as a conservative approach, as no needles are to be inserted. This gave no evidence of effectiveness, probably because the stellate ganglion lies deep in the neck, and because ultrasound waves are likely unable to influence a structure at that depth. Moreover, by 2001, no evidence for the therapeutic use of ultrasound had been found in a review.
Talk nerdy to me
A critical strength of this review is its systematic assessment of the methodological quality and risk of bias (RoB) of the included RCTs using a modified Cochrane tool. The tool was used by two independent raters to assess each manuscript’s methodological quality and risk of bias, across 9 critical domains: random sequence generation, allocation concealment, blinding of study participants and personnel, blinding of outcome assessment (both self-reported and investigator-administered), completeness of outcome data (attrition bias and method of analysis), selective reporting, and other biases (sample size and follow-up duration). Each domain was rated as low, unclear, or high RoB, and an overall RoB rating was assigned.
The assessment of risk of bias rated 23 out of 33 studies as high (70%), 8 as unclear, and 2 studies a low risk of bias. This means that a large proportion of the evidence base is susceptible to bias, which can either overestimate or underestimate the true effects of the interventions. While the study noted that most studies had a low risk of bias in aspects like random sequence generation and allocation concealment, these strengths were often overshadowed by the limitations of small sample sizes and short follow-up periods. However, it’s important to consider that as more research is conducted and published over time, the number of studies available for future systematic reviews and meta-analyses will likely increase. This growth in the body of evidence should lead to studies with larger sample sizes and potentially longer follow-up periods. If these limitations become less common in future research, the overall risk of bias in systematic reviews of CRPS rehabilitation interventions will likely decrease. This evolution in the quality and quantity of research will ultimately contribute to a more robust and clearer understanding of effective treatments for CRPS.
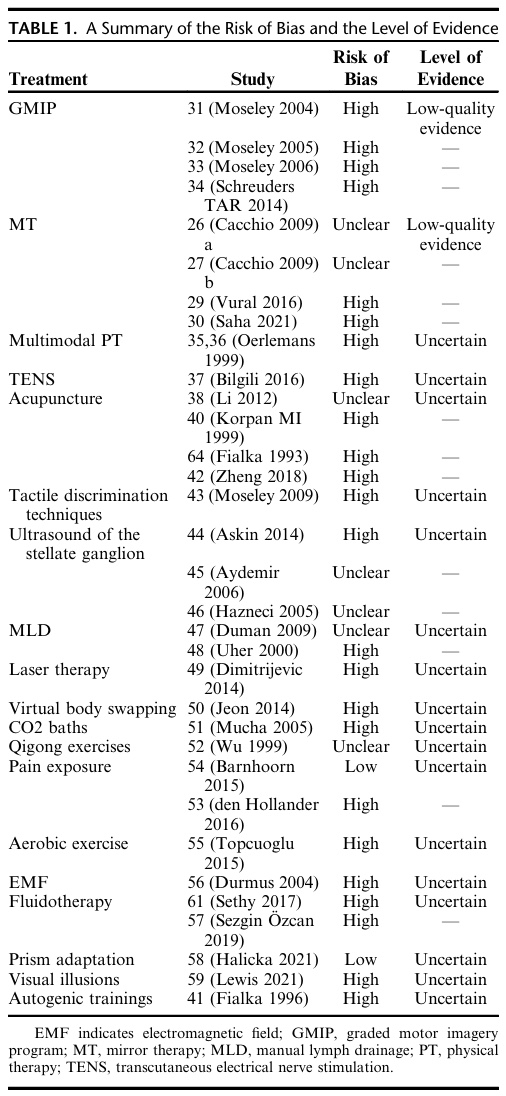
The lack of evidence coming from RCTs of CRPS-2 is a critical gap in the literature. Therefore, these conclusions can not be translated into CRPS-2, where signs of nerve lesions become apparent. Further, no assessment of publication bias could be conducted since too few studies were included per rehabilitation intervention for CRPS, indicating that the available evidence may be skewed. Also, there is only limited evidence on how commonly used psychological and occupation-based interventions might be effectively implemented for CRPS. This highlights areas where more research is desperately needed and suggests that for certain patient populations or intervention types, we are working with very limited specific evidence.
Take-home messages
This systematic review and meta-analysis looked at various non-invasive treatments that physiotherapists and other rehabilitation professionals use for CRPS. The goal was to see how effective these treatments are in reducing pain and improving function or reducing disability.
What the review found is that while some interventions, like Mirror Therapy, Graded Motor Imagery, and Pain Exposure Therapy, may show promise in improving pain and disability in CRPS-1 patients, the overall evidence is not very strong or certain. Think of it like this: the studies available suggest these treatments might work, and in some cases show a large potential improvement, but we can’t be highly confident in these findings yet.
Other interventions, such as Acupuncture, Ultrasound Targeting the Stellate Ganglion, Fluidotherapy, and TENS, have even less certain evidence, with the review concluding it’s “very uncertain about the effect” of these compared to other treatments or placebos.
Essentially, while we have some indications that certain rehabilitation interventions for CRPS could be beneficial, the current body of research doesn’t provide a definitive “this works for sure” answer for most interventions.
A Potential Threatening Limitation:
One of the biggest red flags in this review, and a limitation that seriously endangers the conclusions and validity of the findings, is the poor quality of many of the original studies. A large majority of the included studies had a high or unclear risk of bias, but mostly this came from sample size limitations and short periods of follow-up. Two key aspects that’ll likely improve with future studies becoming available.
Reference
Learn more
Watch two 100% Free Webinars on Shoulder Pain and Ulna-Side Wrist Pain
Improve your Clinical Reasoning for Exercise Prescription in the Active Person with Shoulder pain with Andrew Cuff and Navigate Clinical Diagnosis & Management featuring a Case Study of Golfer with Thomas Mitchell