Why Physiotherapy for Substance Use Disorder Deserves a Place in Multidisciplinary Care

Introduction
Substance use disorder (SUD) is a treatable neurobehavioral condition characterized by the inability to control the use of drugs, alcohol, or medications1. In the U.S., opioid overprescription for chronic pain has fueled a devastating SUD epidemic—yet physiotherapy, a discipline uniquely equipped to address pain through movement and neuroscience, remains underutilized in this population.
With specialized expertise in functional rehabilitation and advancing knowledge in pain science, physiotherapists are uniquely positioned to interrupt this harmful cycle. Patients with SUD often present with reduced cardiovascular fitness, muscle weakness, and mobility impairments—all areas within physiotherapy scope.
While this article focuses on opioid-related cases (reflecting the U.S. crisis), its findings demonstrate how physiotherapy for substance use disorder can transform broader psychiatric care. We challenge traditional practice boundaries by:
- Addressing pain without reliance on opioids through evidence-based, non-pharmacological strategies.
- Restoring physical function to combat SUD-related deconditioning.
- Expanding physiotherapists role in multidisciplinary SUD teams, bridging gaps in holistic care.
Methods
Participants
Participants were recruited from two residential Addiction Recovery Care (ARC) centers within the same U.S. healthcare system. The cohort consisted exclusively of women undergoing medically managed outpatient or intensive outpatient treatment for substance use disorder (SUD), all of whom met the following criteria: (1) presence of musculoskeletal pain, (2) minimum 5 days post-detoxification from alcohol or drugs, and (3) current enrollment in medication-assisted detoxification therapy.
Recruitment and Procedures
Eligible patients were referred by nursing staff and offered free physiotherapy for substance use disorder during a dedicated consultation. During this session, participants completed baseline questionnaires, with follow-up assessments administered after 30 days.
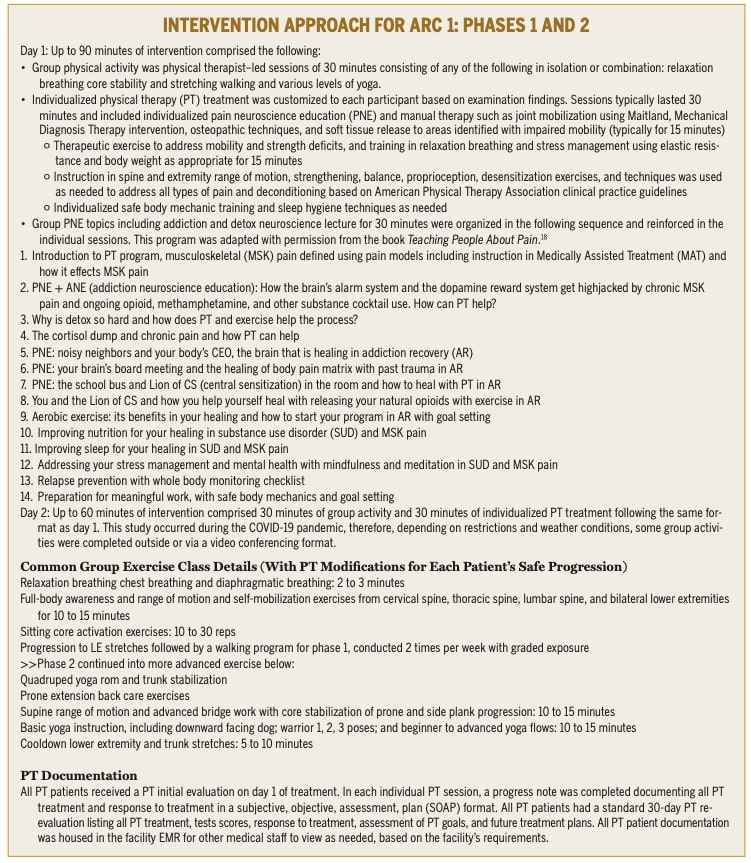
- ARC1 (Intervention Group): Received physiotherapy twice weekly for 30 days, including:
- Group sessions: Yoga, mindfulness breathing, and guided walking.
- Weekly 30-minute lectures: Pain neuroscience education (PNE) and SUD-related content.
- ARC2 (Control Group): Received standard care (medical management, counseling, walking sessions) without physiotherapy or PNE.
Both centers provided identical services except for physiotherapy/PNE, minimizing performance bias. Questionnaires were administered in person by the study’s lead physiotherapist to ensure comprehension and address participant questions.
Clinical Assessments
All participants underwent a comprehensive physiotherapy evaluation, including:
- Subjective history: Illness trajectory, mental health, pain characteristics, substance use patterns, trauma exposure (e.g., Adverse Childhood Experiences).
- Objective measures: Active range of motion, strength, mobility, and sensory testing (hypoalgesia/allodynia via palpation).
Outcome Measures
The study utilized two primary outcome measures to evaluate participants’ progress.
Central Sensitization Inventory (CSI)
served as the first measure, assessing pain centralization through a 100-point scale. Scores were categorized into five severity levels: extreme (60-100), severe (50-59), moderate (40-49), mild (30-39), and subclinical (0-29).
The Recovery Exercise Program Index (REP Index) is a 70-point composite tool developed by two physiotherapists specialized in substance use disorders. It combines items from multiple validated questionnaires to assess self-efficacy, sleep, physical activity, and pain coping strategies. This self-reported questionnaire produces scores ranging from 4 to 70, with lower values indicating greater recovery potential. While showing moderate reliability (Cronbach’s α ≥0.70) in non-SUD populations, further validation is needed for SUD cohorts.
Statistical analysis
Baseline comparisons used independent t-tests (continuous data) and chi-square tests (categorical data). Normality of CSI and REP Index scores was confirmed via Shapiro-Wilk. Primary analysis employed 2×2 repeated-measures ANOVA (between-factor: group [Physiotherapy+PNE vs control]; within-factor: time [pre/post]) with Bonferroni-corrected post-hoc tests (α=0.05). Effect sizes were calculated using Cohen’s d (small<0.20; moderate≥0.50; large≥0.80). NNT analysis identified clinically meaningful improvement (CSI reduction ≥10 points + severity category downgrade in patients with baseline CSI>29). Analyses conducted in SPSS v28 (except Cohen’s d via online calculator). For detailed statistical explanations, see the “Talk Nerdy to Me” section.
Results
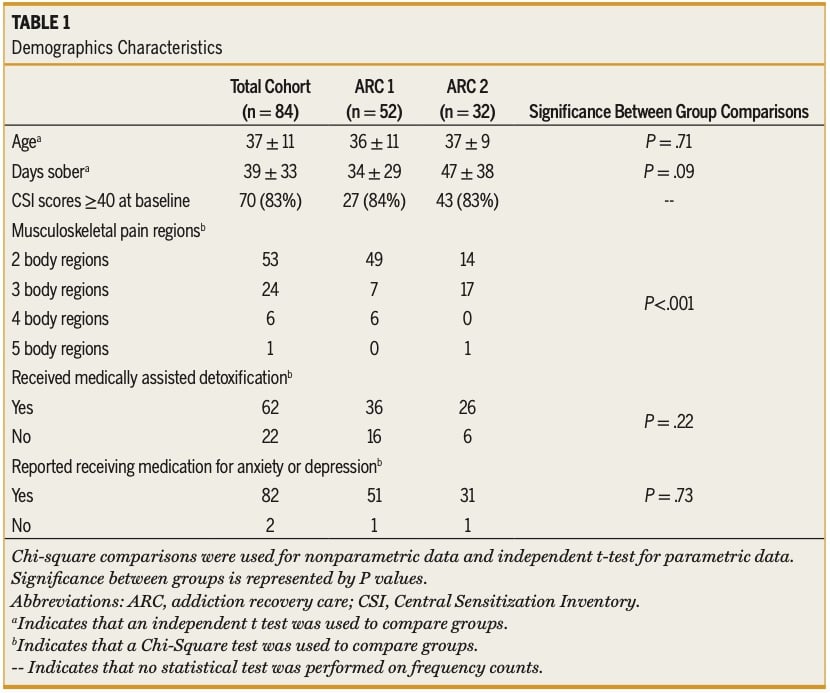
Participant Characteristics
The study included 84 women across both ARC1 (Physiotherapy+PNE) and ARC2 (control) groups. Demographic data were comparable between groups (Figure 1), with the exception of pain distribution: ARC2 participants reported more widespread pain (71% had ≥3 affected body regions) compared to ARC1 (74% had 2 affected regions). Notably, nearly all participants in both groups were prescribed medications for anxiety/depression and detoxification.
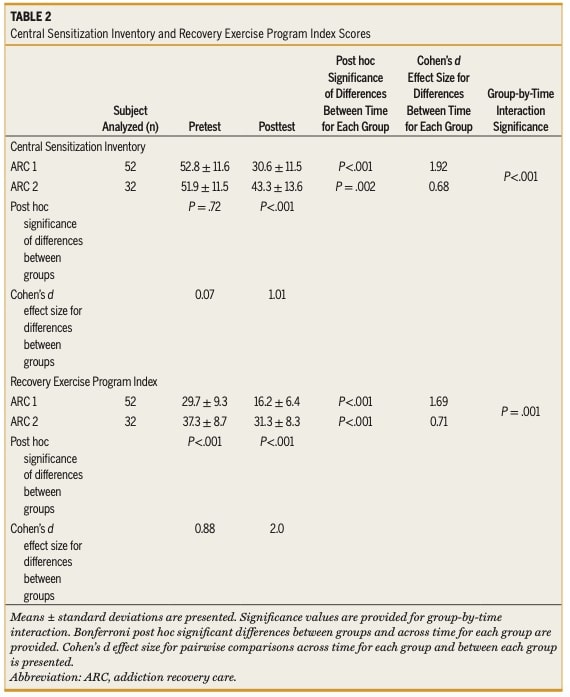
Central Sensitization Inventory (CSI) Outcomes
Repeated-measures ANOVA revealed significant time × group interactions for CSI scores:
- ARC1 (Physiotherapy+PNE): Large effect size improvement (*d* > 0.80)
- ARC2 (control): Moderate effect size improvement (*d* > 0.50)
Both groups showed improvement over time, but the Physiotherapy+PNE group demonstrated significantly better clinical outcomes. Initial severe symptom levels (CSI >40) were comparable between groups (ARC1: 81% vs ARC2: 84%). After treatment, 77% of Physiotherapy+PNE patients achieved clinically meaningful improvement (≥10-point CSI reduction plus severity category improvement), nearly double the rate of controls (44%). This superior effectiveness is reflected in the NNT of 3, meaning only three patients need to be treated with Physiotherapy +PNE for one additional patient to benefit meaningfully compared to standard care.
Recovery Exercise Program Index (REP Index)
Pretest REP Index scores differed significantly between groups (*p* < 0.05), potentially attributable to the one-time pain neuroscience education session ARC1 received before the study. Post-hoc analysis with Bonferroni correction confirmed:
- ARC1: Large effect size (*d* > 0.80)
- ARC2: Moderate effect size (*d* > 0.50)
Question and thoughts
While the study demonstrates promising outcomes using Physiotherapy+PNE in SUD recovery through physiotherapy for substance use disorder, several methodological factors warrant discussion. The absence of a standardized protocol and sham intervention introduces potential confounding from placebo effects (improvement due to treatment expectations), contextual factors (non-specific elements like therapeutic environment or clinician attention), and suggestion bias (outcome influence from researcher communication). The Hawthorne effect (behavioral changes from observation awareness) may have been particularly relevant, as ARC1 participants had more frequent interactions with the researching physiotherapist Furthermore, the exclusive female sample and short 30-day timeframe limit generalizability.
Notably, both groups showed CSI improvement, potentially reflecting uncontrolled medication effects (detox/psychotropic drugs), natural recovery trajectories, or non-specific therapeutic factors. The authors addressed these limitations through the Number Needed to Treat (NNT) statistical tool. We will further examine the statistical methods in the Talk Nerdy to Me section to clarify how these tools shape the study’s conclusions. As detailed below, the NNT of 3—calculated using strict clinical improvement criteria (≥10-point CSI reduction + severity downgrade)— provide compelling evidence for the efficacy of physiotherapy for substance use disorder through combined Physiotherapy+PNE interventions. This finding aligns with established literature on PNE’s effectiveness in chronic pain populations without SUD (refer to this link for the systematic review).
Talk nerdy to me
The study compared participant characteristics across centers using independent *t*-tests for continuous variables (e.g., age, baseline scores) and chi-square tests for categorical variables (e.g., gender). These tests ensured the groups were statistically similar before interventions, reducing confounding effects.
The Shapiro-Wilk test assessed whether the outcome measures (CSI and REP Index) followed a normal distribution (a symmetric, bell-shaped curve where most data points cluster around the mean, with predictable probabilities for values further away). Both variables met this criterion, justifying parametric tests like ANOVA. Non-normal data would require non-parametric alternatives (e.g., Wilcoxon tests).
Treatment effects were analyzed using repeated-measures ANOVA, assessing both between-group differences (Physiotherapy+PNE vs. standard care) and within-group changes over time (pre- to post-treatment). The Bonferroni correction was applied to post-hoc comparisons to control for Type I error (false positives: concluding an effect exists when it does not). By adjusting the significance threshold (e.g., from *p* ≤ 0.05 to *p* ≤ 0.025 for two tests), this method ensures more conservative and reliable results.
Cohen’s *d* quantified the magnitude of differences between groups or time points. Values were interpreted as small (*d* < 0.20), moderate (*d* ≥ 0.50), or large (*d* ≥ 0.80). This complements *p*-values by showing whether differences are clinically meaningful, not just statistically significant.
The study used the “Number Needed to Treat” (NNT) to measure the treatment’s real-world impact. Here, the NNT was 3, meaning for every 3 patients treated with Physiotherapy+PNE (versus no treatment), 1 additional patient achieved meaningful improvement – defined as both a ≥10-point pain score reduction and moving down one symptom severity level. An NNT of 3 is considered very effective. For context: a lower NNT (like 2) means the treatment helps more people (better), while a higher NNT (like 10+) suggests the treatment has limited benefit. However, the NNT cannot fully isolate PNE’s unique contribution from exercise effects due to uncontrolled medications and study design limitations (e.g., lack of sham group).
Take home messages
Despite methodological limitations (e.g., potential placebo effects, uncontrolled contextual factors), this study on physiotherapy for substance use disorder highlights two critical insights for clinical practice:
Physiotherapist’s Emerging Role in SUD/Psychiatric Care
- Demonstrated clinically meaningful improvements (NNT=3) with Physiotherapy+PNE in women with SUD, even amid complex biopsychosocial factors.
- Aligns with growing evidence that movement and pain neuroscience education can address both physical and behavioral health.
Advocating for Physiotherapy Expertise
- Reinforces Physiotherapists’ value in multidisciplinary SUD teams, particularly for:
- Managing opioid-alternative pain strategies
- Addressing SUD-related deconditioning
- Breaking the pain-substance use cycle
- Calls for higher-quality trials to isolate specific Physiotherapists’ effects while leveraging these preliminary real-world findings.
These findings may help inform discussions about integrating physiotherapy for substance use disorder into treatment programs, while acknowledging the study’s limitations as part of a balanced evidence-based approach.
If you want to learn how physiotherapy can reduce opioid prescriptions for low back pain, see Friedman et al. (2020) for evidence supporting this non-pharmacological alternative.
Reference
100% Free Headache Home Exercise Program
Download this FREE home exercise program for your patients suffering from headaches. Just print it out and hand it to them for them to perform these exercises at home