The Prevalence of Neuropathic-Like Symptoms in Tendinopathy and Overuse Injuries

Introduction
The International Association for the Study of Pain (IASP) defined pain to be categorized as nociceptive, neuropathic, and nociplastic pain. These three phenotypes can guide clinicians to select the most appropriate treatment for each condition. While tendinopathy is thought to be mostly nociceptive in origin, reports have speculated that altered pain processing can be present. Because not much is known about altered pain processing in tendinopathy, this systematic review and meta-analysis examined the prevalence of neuropathic-like symptoms in tendinopathy and overuse injuries of the upper and lower extremities.
Methods
This systematic review with meta-analysis included adults aged 18 years and older with painful tendinopathy of the upper or lower extremities. They did not have any condition that could lead to altered nociceptive pain processing, such as fibromyalgia or rheumatoid arthritis.
Diagnosis of tendinopathy was established and could be supplemented with positive imaging, however, this was not required. The included people with tendinopathy had to be compared against a group of pain-free individuals who had no musculoskeletal pain condition.
The primary outcome was the prevalence of neuropathic-like symptoms in tendinopathy and or overuse injuries, assessed using any patient-reported outcome measure (PROM). Eligible studies were cross-sectional or prospective case-control or cohort studies. Clinical trials could be included as well, but in that case only baseline data was used for anaysis. Studies examining experimentally-induced tendon pain were excluded.
Results
Out of 1285 records, 8 studies were included in the review and meta-analysis. Five were cohort studies, one was a case-control study, and two were clinical trials. Lateral epicondylalgia was examined in two articles, three studies looked into patellar or quadriceps tendinopathy, two studies were about plantar heel pain/plantar fasciitis, greater trochanteric pain syndrome was assessed in two studies and five elaborated on Achilles tendinopathy. One study did not mention the tendinopathy investigated.
By including these eight studies, a patient sample of 920 people with painful tendinopathy were included. On average half was female, and the mean age was 51 years (SD: 12.5 years). The average pain duration was 30 months (SD: 28.5 months).
The studies assessed the presence of neuropathic-like symptoms in tendinopathy using the painDETECT questionnaire in 5 studies, the Self-Report Leeds Assessment of Neuropathic Symptoms (S-LANSS) in 2 studies, and the Douleur Neuropathique-4 (DN-4) in one study.
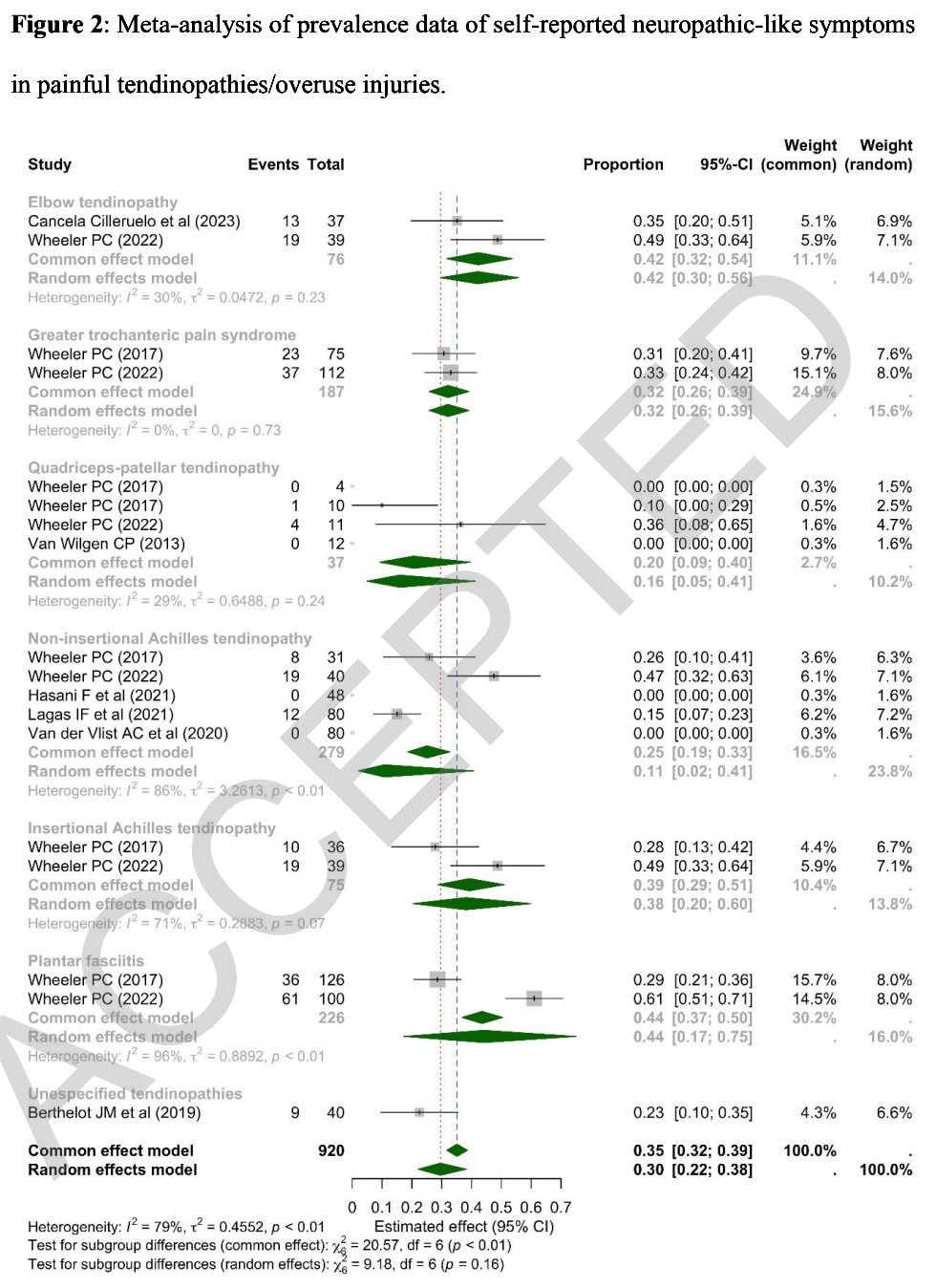
An overal presence of neuropathic-like symptoms in tendinopathy of 30% (95% CI 22% to 38%) was found, with high heterogeneity (I2 = 79%). A lot of variation was observed in the presence of neuropathic-like symptoms across the different body regions. Plantar heel pain and lateral epicondylalgia were most commonly accompanied by neuropathic-like symptoms, with prevalences of 44% and 42% respectively reported. Greater trochanteric pain syndrome had a reported prevalence of neuropathic-like symptoms of 32%. The prevalence of neuropathic-like symptoms in Achilles tendinopathy differed between non-insertional and insertional tendinopathies, with 38% prevalence reported in insertional, while only 11% for non-insertional was found. Finally, 16% prevalence was reported in quadriceps/patellar tendinopathy.
Questions and thoughts
An overall prevalence of neuropathic-like symptoms of 30% is quite remarkable and shouldn’t be neglected. The prevalence varied by condition, with a higher prevalence reported in plantar heel pain compared to non-insertional tendinopathy.
Especially in differential diagnosis, these mixed pain phenotypes can make clinical reasoning more tricky. It was not specified how the tendinopathy diagnosis was established in the individual included studies, so we’re not entirely sure that patients with true tendinopathy were included only.
Although the IASP defined 3 distinct pain phenotypes, there is debate on the validity of categorizing pain. From the study of Kosek et al., (2021), this scheme can help differentiate pain phenotypes.
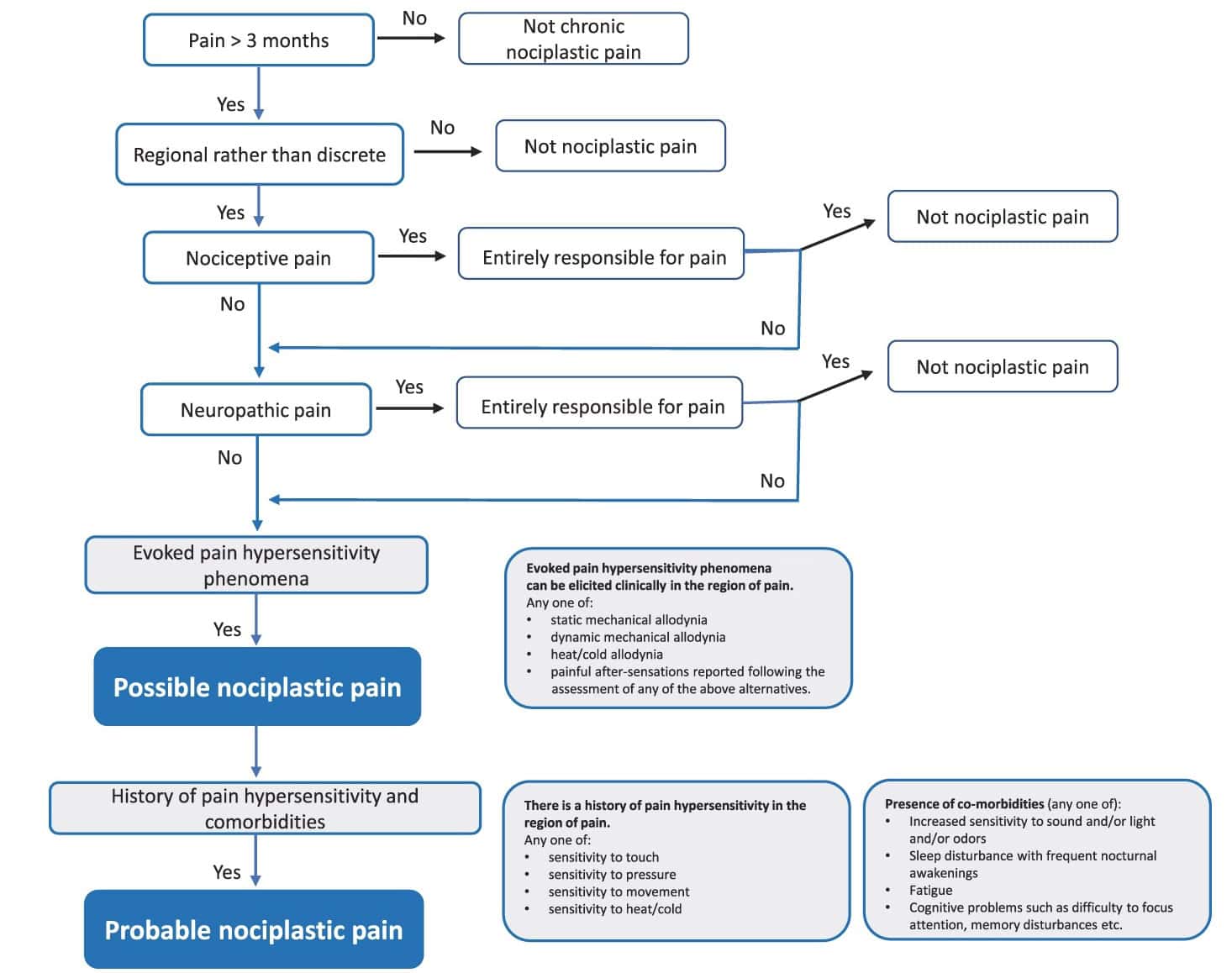
The average pain duration was 30 months, which may be a cause for concern. Did these people had prior treatments or not? Of course, a heterogeneous population was included with different locations of tendinopathy. When someone experiences pain for a prolonged period, this can cause many detrimental effects to occur. Where the initial pain driver was maybe predominantly nociceptive in origin, changes in the pain matrix of the brain can develop, leading to contributing nociplastic pain. But other than that, deconditioning may weaken the muscle and tendon-units, leading to decreased force production and endurance. This altogether can lead to various problems with activities of daily living and interfere with sleep and social interaction which may be underlying drivers of the chronic pain reported.
Talk nerdy to me
The prevalences of neuropathic-like symptoms in tendinopathy and overuse injuries were recorded using self-report PROMs. While these symptoms are sensory in origin, measurements to objectify neuropathic-involvemend exist, like quantitative sensory testing. The authors concluded that a clinical diagnosis of tendinopathy was sufficient.
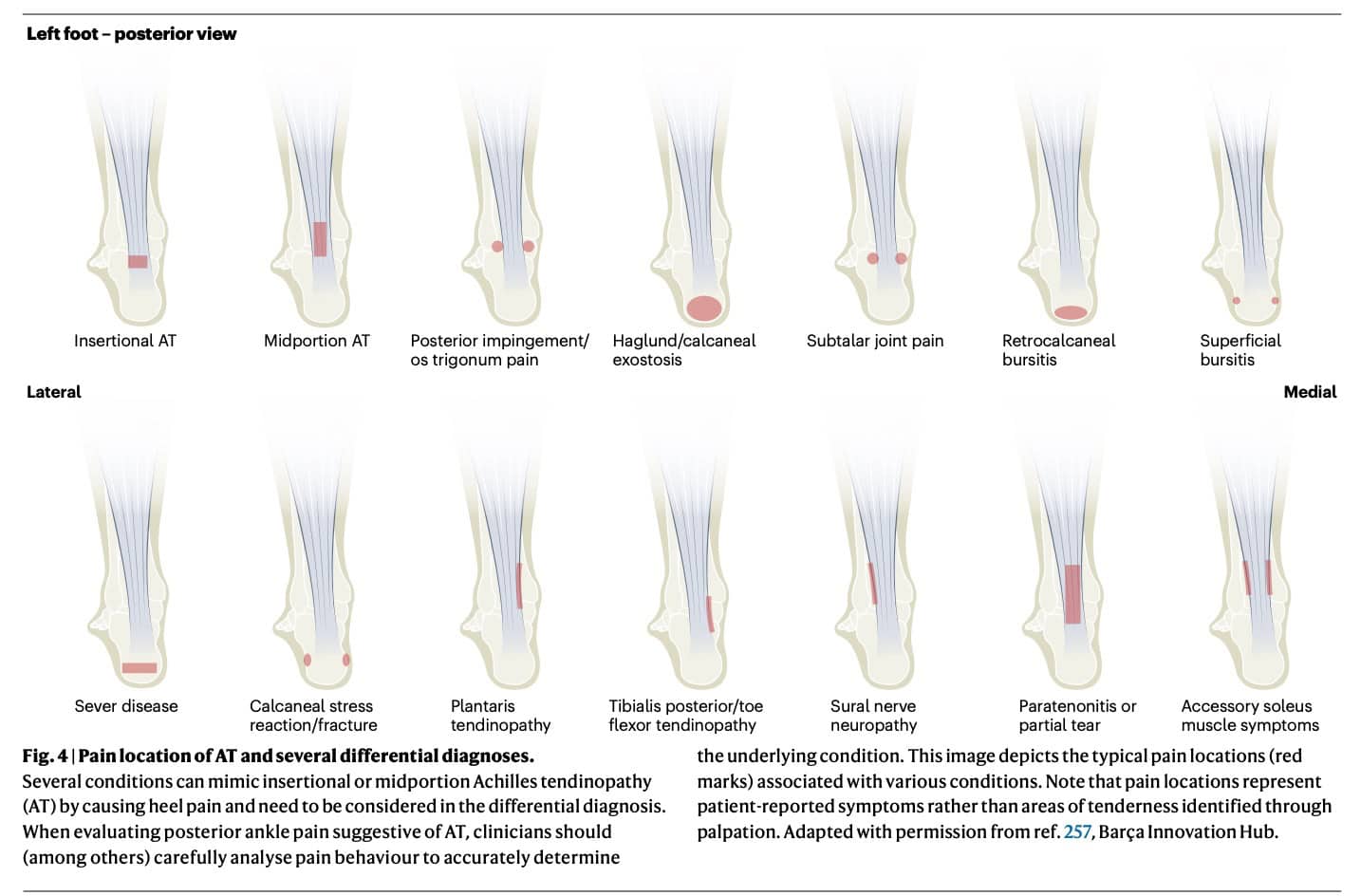
Diagnoses of tendinopathy in the included studies were mainly clinically established in most, without confirmation of tendon changes by imaging analyses. Yet, imaging is not needed for a diagnosis of painful tendinopathy, which we showed already in our review covering posterior tibialis tendinopathy. However, we did not get any information on how differential diagnoses were considered, which makes it difficult to be really confident that only 100% pure tendinopathies were included. The study by Traweger et al. (2025) makes it clear that a lot of differential diagnoses exist in the location of the Achilles tendon, as can be seen in the picture under. When a sural nerve pathology is misdiagnosed as a midportion Achilles tendinopathy, the presence of more neuropathic-like symptoms would be evident. Not exactly knowing how the tendinopathy diagnosis was established is a limitation of this study.
Overall quality of the included studies was moderate to good, but due to the high heterogeneity of the pooled results, one should carefully consider the observed results. Only for greater trochanteric pain syndrome low heterogeneity was found, while lateral epicondylalgia and patellar/quadriceps tendinopathy had moderate heterogeneity in the results. But, even when looking at the different anatomical regions, the low number of included studies per body region may also warrant caution.
As there was a large variation between studies, evidenced by wide confidence intervals, the generalizability of the results is limited. This variation could be due to different diagnostic criteria, patient populations, or duration of symptomatology in the individual studies.
Take-home messages
The presence of neuropathic-like symptoms in tendinopathy and overuse injuries suggests that tendinopathies may not always be purely nociceptive. Instead, they can have a mixed pain profile, involving both nociceptive and neuropathic mechanisms. High heterogeneity warrants careful interpretation of the results, since there was much variation between the studies (for example in duration of the tendinopathy ranging from 13.5 months to 43.2 months. Nevertheless, you should consider the presence of neuropathic-like symptoms to better understand the pain phenotypes driving your patient’s complaints.
Reference
How Nutrition Can Be a Crucial Factor for Central Sensitisation - Video Lecture
Watch this FREE video lecture on Nutrition & Central Sensitisation by Europe’s #1 chronic pain researcher Jo Nijs. Which food patients should avoid will probably surprise you!

