Cervical Radicular Syndrome: To Operate or To Educate?

Introduction
Cervical radicular syndrome is an umbrella term covering cervical radicular pain and cervical radiculopathy. The latter is a condition predominantly caused by a herniated cervical disc, bringing along sensory and motor deficits. Cervical radicular pain manifests as radiating pain along the arm, often severe enough to disrupt daily life. While symptoms often improve within six months, surgical intervention, typically anterior discectomy, is considered when conservative measures fail. Despite reported success rates of 80-95% based on functional and pain outcomes, only two-thirds of patients express satisfaction with the overall relief of their related complaints. This highlights the ongoing need for research to optimize treatment strategies. This CASINO trial was initiated to address the scarcity of knowledge regarding the long-term differences in outcomes between surgical and conservative management for patients with cervical radicular syndrome due to intervertebral disc herniation.
Methods
This prospective cohort study was conducted in the Netherlands over the years 2012 to 2021. Eligible participants were adults from 18 to 75 years who had cervical radicular syndrome, defined as disabling pain or tingling sensations for at least two months. A neurologist or neurosurgeon confirmed the diagnosis, and an MRI scan confirmed the presence of a herniated disc with root compression.
In case of cervical myelopathy (objectified through MRI) or arm paresis, defined as an MRC < 4, participants were excluded.
A surgical and conservative group was created following the consultation with the neurosurgeon. Both options were discussed and balanced with the participant, and in agreement, a decision was made whether to opt for the surgery or the conservative management. No randomization took place.
The participants who chose the surgical intervention underwent a standard anterior discectomy under general anesthesia, where the posterior longitudinal ligament was opened to decompress the nerve root and dura. A PEEK cage was placed in the intervertebral space. Following the procedure, the participants were hospitalized for one to two days, but no physiotherapy took place following the procedure.
For the conservative management group, according to the protocol, the neurologist or the general practitioner was in charge. Participants in this group were informed about the condition and favourable prognosis of cervical radiculopathy. They were encouraged to resume their daily activities. A stepwise approach to pain management with paracetamol, NSAIDs, or tramadol was included if necessary. They were not routinely prescribed physiotherapy or a soft neck collar; however, it was permitted to initiate these treatments if deemed necessary by the patient. They received a schedule targeting graded activity. The participants in this group were safety-netted, meaning that in case of progressive neurological deficits arose or pain became intolerable, patients were referred back to the neurosurgeon to explore potential surgical options.
The primary outcomes were the VAS scale for arm pain and the Neck Disability Index. These measurements were obtained at baseline, 6, 12, 26, 38, 52, and 104 weeks after enrolment. The Neck Disability Index was converted to a 100-point scale, with higher scores representing worse outcomes. The minimal clinically important difference (MCID) was set as a 30% reduction in VAS arm pain and 20 points on the 100-point Neck Disability Index.
Secondary outcomes included the VAS scale for neck pain and the EuroQol VAS (EQ-VAS), which assesses overall health from 0 (worst imaginable health) to 100 (best imaginable health).
Participants’ data were dichotomized to report the distribution of successful and unsuccessful outcomes. The following cut-off values were considered as a good outcome:
- VAS arm pain ≤ 25
- Neck Disability Index ≤ 24
- VAS neck pain ≤ 35
- EQ-VAS ≥ 69
Results
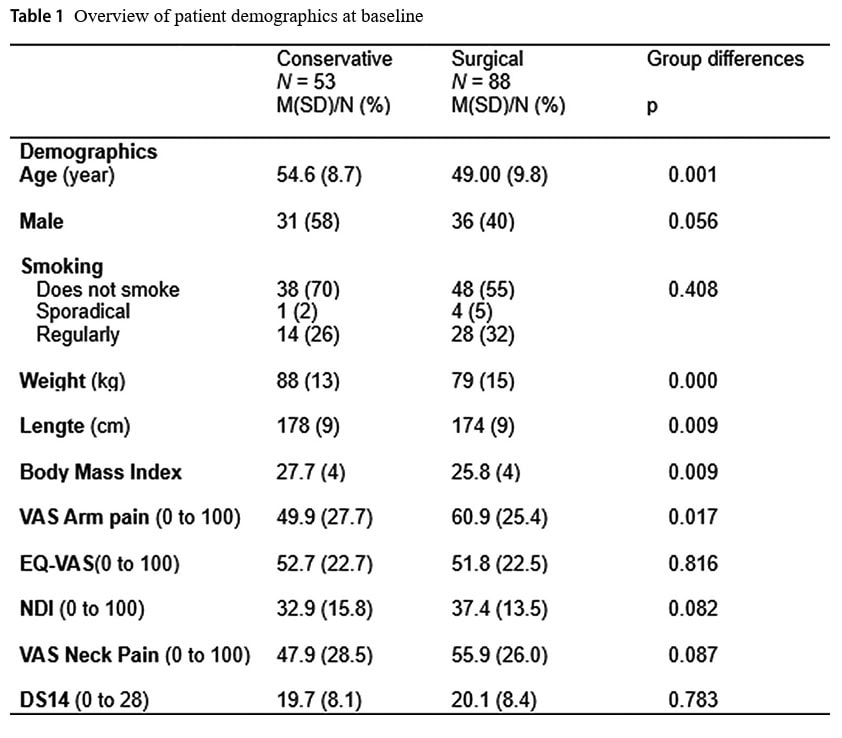
A total of 141 participants were included in the study, 53 of whom were treated conservatively and 88 who opted for surgical anterior decompression.
People in the conservative group were on average 54.6 years old, versus those in the surgical group who were 49 years old. This age difference was statistically significant. In the conservative group, 58% were male, while only 40% were in the surgical group. This gender difference was, however, not statistically significant. The mean body mass index (BMI) in the conservative group was 27.7 kg/m2 compared to 25.8 kg/m2 in the surgery group, leading to a significant difference at baseline. Mean VAS arm pain in the conservative group was 49.9/100 compared to 60.9/100 in the conservative group, also producing a significant baseline difference between the groups.
In the first year, VAS arm pain decreased with an average of 36.9mm in the conservative group compared to 43.9mm in the surgical group. This did not produce a significant between-group difference (p = 0.858).
The Neck Disability Index at one year decreased on average by 13.3 points in the conservative group and by 20.1 points in the surgical group, leading to no significant difference (p=0.329).
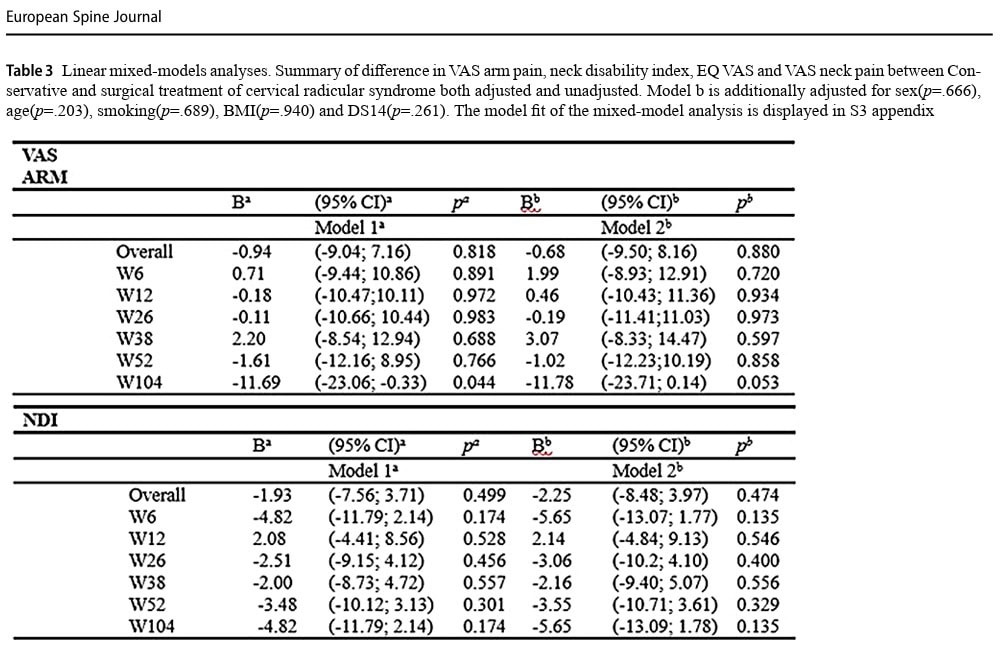
When data were compared at 2 years (104 weeks), the VAS arm pain decreased by 27.1mm in the conservative group and by 41.9mm in the surgical group. This produced no significant between-group difference (p=0.053), although the authors labeled this falsely as a clinically relevant within-group difference since the reduction exceeded the prespecified successful decline of 30%.
The Neck Disability Index at 2 years showed a mean reduction of 12.5 points in the conservative group and 20.6 in the surgical group. This was not statistically significant (p=0.135).
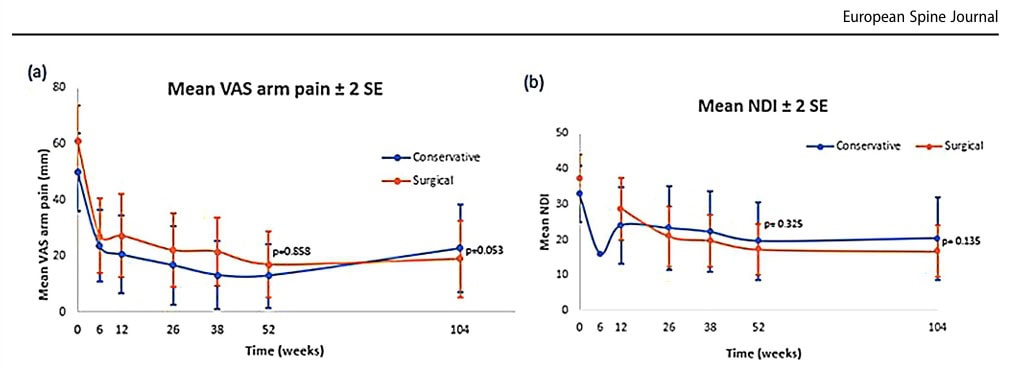
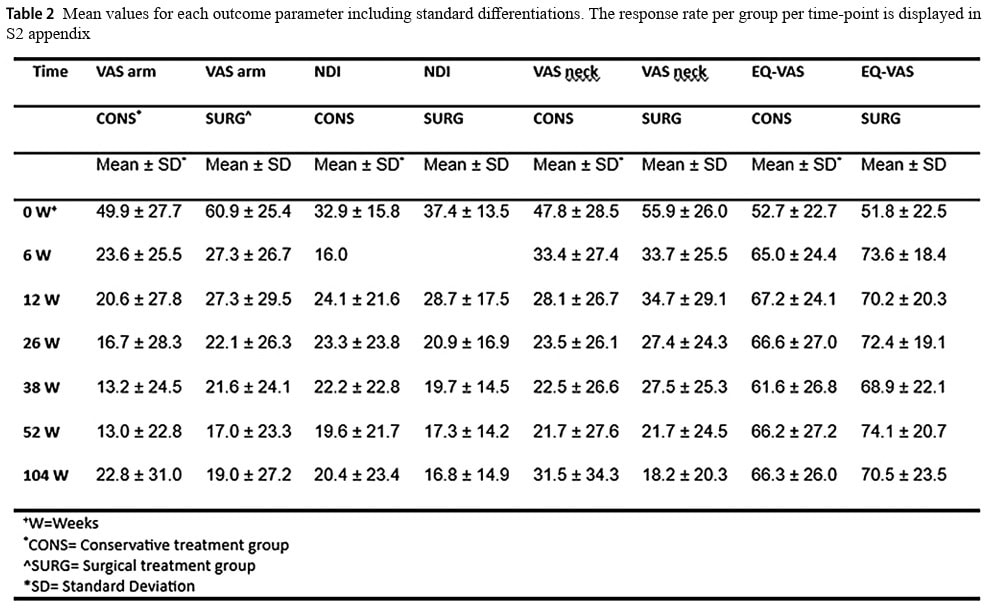
When the VAS arm pain data were dichotomized, 87% of participants in the conservative group and 70% in the surgical group reported a good outcome. This changed to 70% and 74% at 2 years, for the conservative and surgical groups, respectively.
Dichotomizing the Neck Disability Index outcome at 1 year revealed that 76% of the conservative group and 74% of the surgically treated group had a good outcome. At 2 years, this changed to 71% of the conservative group and 80% of the surgical group.
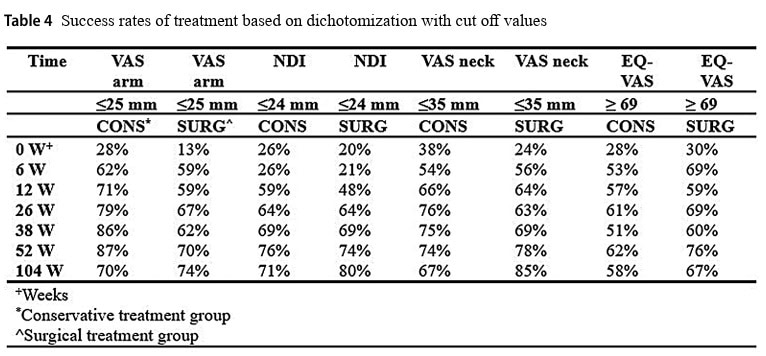
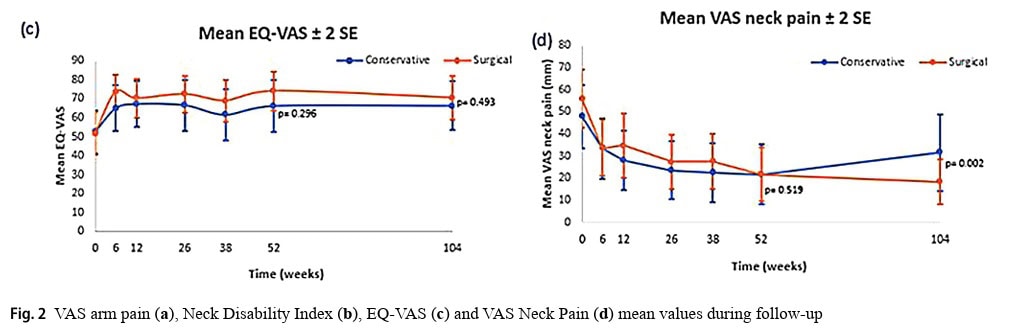
The analysis of secondary outcomes revealed no significant differences (p=0.493) between the groups at 1 or 2 years for the EQ-VAS, although both groups improved over the years. The VAS for neck pain decreased equally over time, but after 2 years, a significant difference was found, favoring the surgical group (p=0.002).
Questions and thoughts
First things first. Something that struck my eye was the inconsistent use of terminology. In the paper, as well as in the protocol, the authors use the terms “cervical radiculopathy” and “cervical radicular syndrome” interchangeably. Although looking similar, these terms are not synonyms, although many times in the literature, the terminology is overlapping and inconsistently used. To be clear, cervical radicular syndrome is an umbrella term under which cervical radicular pain and cervical radiculopathy fall. Where cervical radicular pain is pointing to a painful condition, caused by a compression or irritation of a cervical nerve root, cervical radiculopathy refers to a loss of nerve function. This loss may be motor or sensory in origin, but it can also lead to a loss of reflexes. A combination of pain and loss of nerve function can be referred to as a painful radiculopathy.
Now that that is clear, it is important to know which patient population is studied in this publication. The title points to cervical radiculopathy, implying the condition is characterized by a loss of nerve function. The abstract states cervical radicular syndrome. In the eligibility criteria, “disabling symptoms OR tingling” were specified. This is too broad to be clear. Someone with excruciating pain from cervical radicular pain can have disabling symptoms. Likewise, someone with a loss of motor function originating from cervical radiculopathy can be affected by disabling symptoms. Further, no details about the diagnosis were shared, making it hard to be conclusive which exact patient population was included. Throughout the text, the focus is on pain rather than on loss of neurological function, assuming cervical radicular pain was within the scope. This remains an assumption, however. The lack of clarity in defining the study population limits the interpretability of the results and the applicability to specific clinical subgroups. It is crucial to get the terminology right!
The methodology was changed from an RCT to an observational cohort design. I certainly understand why the authors chose to change the RCT into a cohort study, especially since they encountered problems with recruiting participants. The study ran for nine years, a lot of time, during which the medical field keeps advancing and innovating. Sticking to the original plan to conduct an RCT would have led to wasted resources and recruiting a small sample, with procedures that may be outdated when the publication finally gets submitted, ultimately not contributing to the evidence pile. Yet, an observational study is suboptimal, since it is prone to biases. It was not specifically mentioned where the participants were recruited, but I assume that it was in a tertiary care hospital setting, since the neurologist and neurosurgeon could establish a diagnosis, and the neurosurgeon was involved in making the treatment decision along with the patient. Since these people were already consulting the neurosurgeon, it raises the chances that these people were already seeking more advanced care, implying that they had a bias toward surgery. Indeed, of the 141 eligible candidates, nearly two-thirds opted for surgical care. This may imply that the study was influenced by selection bias and treatment bias. Clinical equipoise, therefore, remains, which would justify an RCT in the future. Since the spaghetti plots indicated substantial heterogeneity, even within the groups, subgroup analyses to further refine responders and non-responding participants would be meaningful.
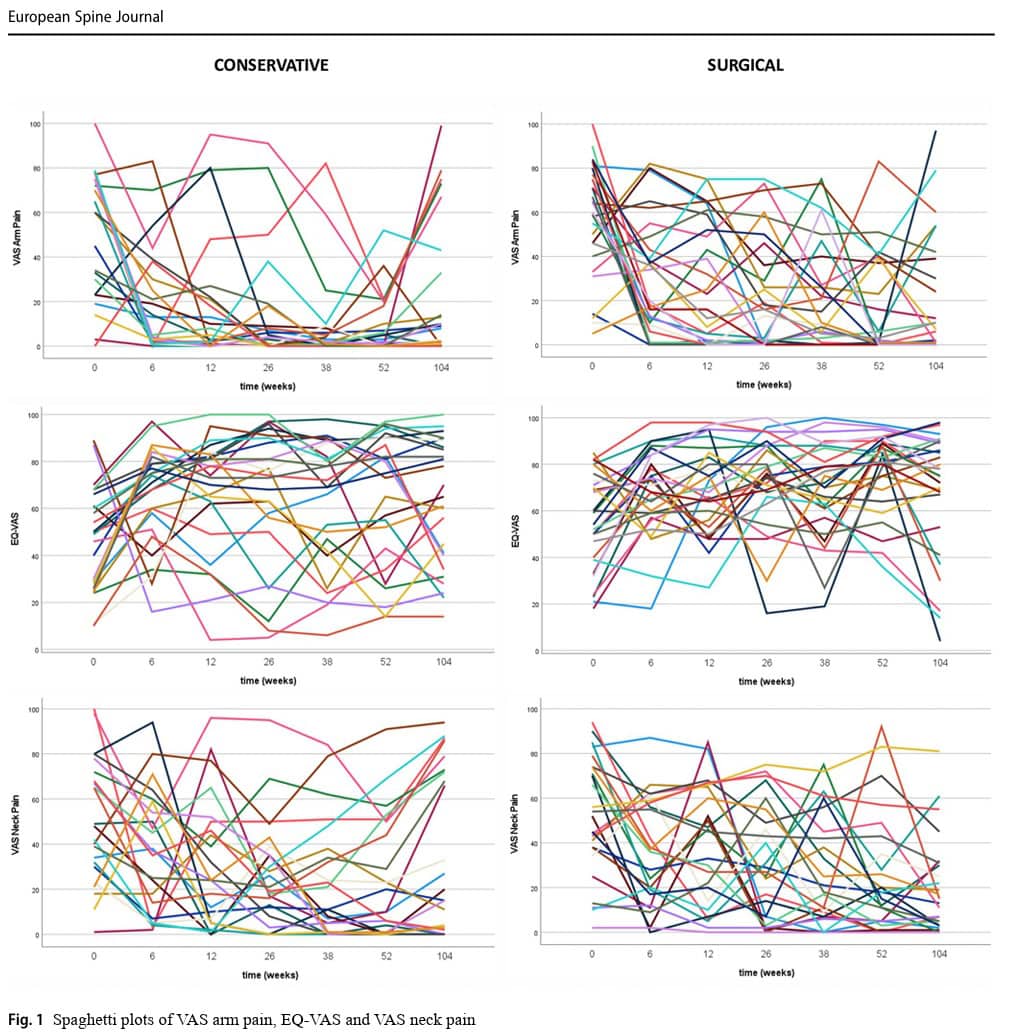
When examining the individual data from the spaghetti plots, much inter-individual variability in the outcomes can be observed. This implies that the study population had significant heterogeneity, which is also reflected in the wide standard deviations. Already at baseline, several factors differed, but interestingly, these differences were not significant as covariates in the analyses. The analyses found no significant confounding effects for the baseline differences, meaning that although the groups were not equal at baseline, these differences are not influencing or predicting the outcomes over time. For example, a significant difference in BMI does not imply that someone with a lower BMI will automatically have a better treatment effect compared to someone with a higher BMI.
The authors confused patient satisfaction with good outcomes. Before analyzing the data, several cut-offs were determined to indicate a good outcome. In the text, when achieving one of the cut-offs, the authors sometimes refer to it as a significant outcome, indicating patient satisfaction. For example, Table 4 depicts that at 2 years, 70% of conservatively treated participants had a VAS arm pain below 25mm/100. The authors label this as a successful outcome, which is comprehensible. Although good outcomes and patient satisfaction may be linked, when someone proposes a certain cut-off score, this does not necessarily mean that the patient sees exceeding this cut-off as a satisfactory outcome. I can imagine that someone with a VAS arm pain below 25, who still has a high Neck Disability Index score, would not be overly satisfied, though the authors label the patient as someone showing a successful outcome. Rather, patients should be involved in the design of a study to indicate what outcomes would indicate success and bring satisfaction to them.
Talk nerdy to me
The study was originally designed to be a randomized controlled trial (RCT), but was transformed into an observational cohort study along the way. The authors explained that this protocol deviation was necessary since inclusion appeared to be challenging. Twelve participants were included in the RCT format before changing to the cohort study format. The protocol deviation was transparently explained in the paper.
Prespecified sample size calculations required 100 participants per group to be included, assuming alpha = 0.05, 90% power, and a 15mm reduction in VAS arm pain as a clinically relevant effect, with a worst-case scenario standard deviation of 30, and taking into account 10% loss to follow-up.
Here are three aspects to discuss:
- The Neck Disability Index was specified as a secondary outcome in the protocol, but was used as a primary outcome measure in the final publication. This post hoc change introduces a risk of outcome reporting bias and raises concerns about selective reporting.
- The MCID was set at a 30% reduction in VAS arm pain, but for the power analysis, a reduction of 15mm was used as being clinically relevant. That is working with double standards.
- While 200 participants were required, the study was halted after 141 participants were enrolled, nine years after the start of enrollment. The authors thus ignored their original sample size calculation, and fewer participants than originally planned were included. This limits the power of the study and can lead to false negative findings.
The results were described according to the MCID, with the caveat regarding the way the authors interpreted this. Let’s take a closer look at what was said.
- For the outcome VAS arm pain, the conservative group showed a reduction in pain from 49.9/100 to 13.0 at 1 year. On the VAS scale, this means a difference of more than 30mm out of 100mm, exceeding the MCID of 30mm. Going from 49.9 mm to 13.0 mm is a reduction of 74%.
- For the outcome VAS neck pain, a reduction from 47.8mm to 21.7mm was observed in the conservative group. While this means a reduction of 54.6%, seemingly surpassing the MCID, this difference of 26.1mm lies beneath the threshold MCID of 30mm.
- Although in this publication, this misinterpretation was not overemphasized to indicate a difference when in fact there is none, this is a common misinterpretation/misleading that you should always look out for when reading a paper. When a 30mm reduction on a scale of 100mm is required (which is 30%), you should always look out for the common distorted picture of labeling a 30% difference as being clinically relevant when it is expressed on the initial score instead of on the total scale.
- As you can see, a 30% reduction is not a 30/100-point reduction.
As cervical radicular pain is typically more pronounced in the arm than in the neck, the authors did a good job in prioritizing VAS arm pain as a primary outcome measure. While both groups demonstrated meaningful reductions over time, the decrease in arm pain did not reach a significant between-group difference. Despite that both groups had a worthwhile reduction in arm pain, no superiority of one treatment above another could be pinpointed, as such. Only the VAS for neck pain reached a statistically significant between-group difference at 2 years, favoring the surgical group. But when people complain more about their arm pain when having this condition, and the only significant between-group difference is found for the secondary outcome VAS neck pain, on top, they have to wait 2 years before outperforming the conservative group, does this indicate a superiority of surgery? I don’t think so, and the 95% confidence interval supports this thought since it ranges from -30.71 (which surpasses the MCID) to -7.03 (which lies roughly below the MCID). And on top of that, the only significant difference was obtained in a secondary outcome in a study where no Bonferroni correction for multiple comparisons was adopted, increasing the risk of false-positive findings.
Lastly, very little information was provided regarding the patients throughout the study. As written in the methodology, in the conservative group, physiotherapy was not routinely prescribed, although it was allowed. Nowhere in the publication were coexisting treatments or medication use mentioned. Since the GP and neurologist were in charge of the patient, the care was likely more biomedically oriented. The good improvements in this group do not indicate that a physiotherapy consultation is per se necessary, but since little detail is shared, we do not know exactly how biopsychosocially-oriented the education and information were. Was the talk patient-centered, or did everyone receive the same pre-cooked advice? How much time was spent for this consultation? Furthermore, no information was shared about the affected cervical levels, although MRI scans were necessary for diagnosis. The pre-published protocol does not clarify these issues, advocating for future, more transparent trials.
Take-home messages
While the authors point to potential beneficial results after surgery for cervical radicular pain, closer inspection of the data does not support this conclusion. Furthermore, this cohort design is not able to give conclusive evidence on the superiority of one of the treatments.
Since observational studies can not rule out common biases (selection bias, confounding bias – for example, patients opting for surgery having better expectations for surgery to “cure” them), an RCT might be justified. A pilot RCT should be conducted first to address issues with patient recruitment, as observed in this study.
As in this CASINO trial, the patient population is described in vague terms, which leaves the reader uncertain whether participants were experiencing radicular pain alone or had progressed to cervical radiculopathy with neurological deficits. This ambiguity is not trivial; pain without dysfunction and pain with objective nerve impairment often respond differently to interventions. Without clear diagnostic boundaries, interpreting the results becomes a game of chance, ironically befitting the trial’s name. Like spinning the roulette wheel without knowing which numbers correspond to which clinical presentation, this lack of specificity introduces a form of methodological randomness that undermines the external validity of the findings
Reference
100% Free Headache Home Exercise Program
Download this FREE home exercise program for your patients suffering from headaches. Just print it out and hand it to them for them to perform these exercises at home