Tension-Type Headaches | Diagnosis & Treatment for Physios

Tension-Type Headaches | Diagnosis & Treatment for Physios
Introduction & Epidemiology
Headaches can manifest on their own but are also a very common symptom in neck pain patients as more than 60% of patients with a primary neck pain complaint report having concordant episodes of headaches. Therefore it’s essential to find out what kind of headache the patient is suffering from.
To start off let’s differentiate between primary and secondary types of headaches. But what does this mean? Simply put, primary headaches are a “disease themselves” whereas, in secondary headaches, the headache is a symptom of another condition. So primary headaches would be migraines, tension-type headaches & cluster headaches. Secondary type headaches are headaches caused by tumors, hemorrhage, other trauma, TMJ dysfunction, substance overdose, or neck pain aka. The cervicogenic headache.
Now let’s take a closer look at tension-type headaches, which are primary types of headaches.
Epidemiology
When looking at the current prevalence of different forms of headaches, TTH is the most prevalent form in the adult population worldwide with a mean prevalence of 42%, followed by migraine with 11% (Stovner et al. (2007). The following graph shows the current prevalence of different forms of headaches in different age categories (Stovner et al. (2007):

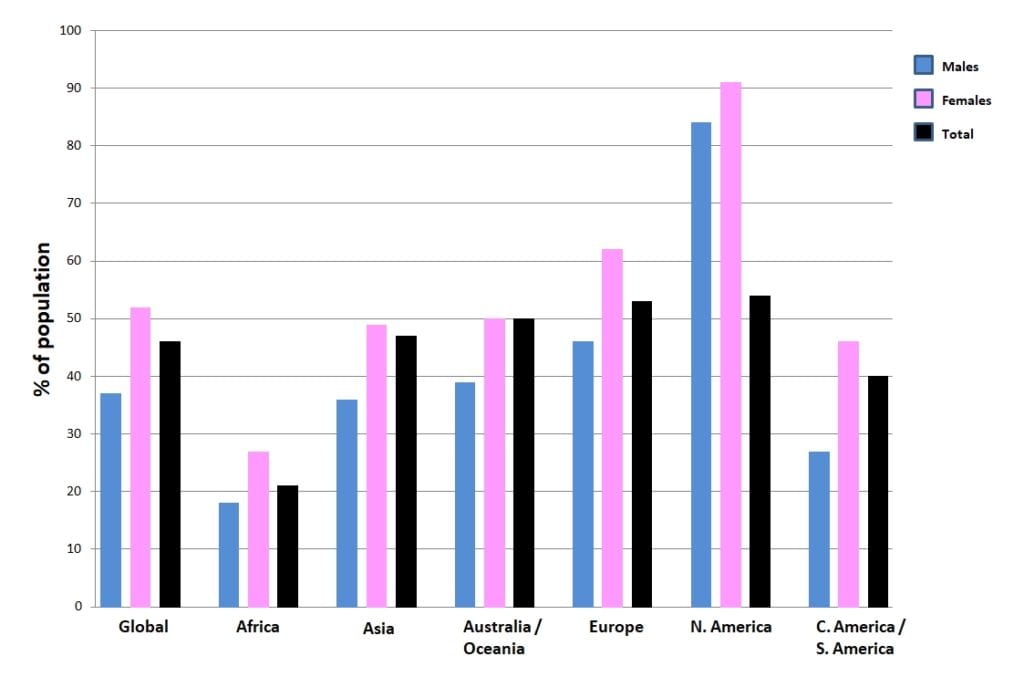
The following figure shows the prevalence of headaches on different continents around the world:
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
Tension-type headaches can vary from infrequent episodic, frequent episodic, to chronic. As seen in this table.

While the frequency and duration differ, patients in all three categories need to report at least 2 of the following four characteristics (ICD-H-III):
-
- The headache is bilateral
- It has a pressing or tightening quality but NOT pulsating
- The intensity is mild to moderate so a patient will usually still be able to complete ADLs as
- The headache is not aggravated by routine physical activity such as walking or climbing stairs.
Also, there is
- NO nausea or vomiting
- No more than one of photophobia or phonophobia which is sensitivity to light and sounds respectively
Tools you can use to assess the impact of a headache on your patient are the HIT-6 questionnaire. Also note that it can be difficult for a patient to answer all of the questions on duration, intensity, and characteristics of their headache during your assessment. Therefore asking them to complete a headache diary can help in the assessment and management of the headache and you should be aware that there can be overlap between multiple headache disorders.
Examination
In comparison with healthy controls, the average patient with tension-type headaches differs on provocation, cervical range of motion, neck muscle endurance and forward head position.
The goal of provocation tests is to recreate the patient’s familiar pain. This way, you are able to confirm the location of nociception in the cervical structures, possibly leading to referred pain to the head. While provocative testing for CGH can be done with the techniques shown in the following tab, the phenomenon of referred pain to the head for tension-type headaches and migraine can be provoked with the Watson test:
Although no clear cut-off values are given, the performance time can give an indication of neck flexor endurance:
Upper cervical range of motion in the direction of rotation can be reliably and accurately assessed with the Flexion-Rotation Test (Hall et al. 2010a, Ogince et al. 2007, Hall et al 2010b). This test – if positive – can give you an indication of limited rotation on segments C1/C2. In turn, hypomobility on C0/C1 or C2/C3 can lead to this limitation in rotation on C1/C2.So in case of a positive test, we still need to perform intervertebral motion assessment of all upper cervical segments in order to find the dysfunctional segment.
Forward head posture (FHP) refers to the anterior positioning of the head relative to the torso in a reproducible upright posture. Measuring the horizontal gap between the tragus and the C7 spinous process has been reported to be the most reliable method compared to the horizontal gap between the tragus and acromion process and the craniovertebral angle between the tragus and the C7 spinous process (Lee et al. 2017). The authors report almost perfect intra-rater reliability in both sitting (comfortably or straight) and standing (comfortably or straight) positions with ICC values >0.9 in young healthy Chinese individuals.

When looking at norm values the literature is rather scarce and usually, the craniovertebral angle is described as the sole measurement. Nemmers et al. (2005) describe that a clinician could expect young healthy adults to exhibit an average normal FHP within a 10° range from 49° to 59° when the craniovertebral angle was used as a reference. In their study, the authors report an angle of 48.84° for the 65-74-year-old, 41.2° for the 75-84-year-old, and 35.6° for people in the 85+ range in healthy community-dwelling older women.
In their randomized controlled trial, Harman et al. (2005) defined a forward head posture as soon as the distance between the tragus to the posterior angle of the acromion was greater than 5cm. Fernández-de-las-Peñas (et al. 2006) found a craniovertebral angle of 45.3° in patients with chronic TTH compared to an angle of 54.1° in healthy controls.
Caneiro et al. (2010) showed that slumped sitting is associated with an increased cervical flexion and anterior translation of the head compared to upright sitting. Such postural stress might activate peripheral cervical nociceptors in upper cervical structures like the suboccipital muscles or facet joints which can lead to referred head pain (Mingels et al. 2019). Neuroanatomical, biomechanical, and non-nociceptive pathways seem to justify profiling patients based on a postural trigger. Further research is needed to determine the contribution of postural dysfunctions to headaches and the effect of specific interventions (Mingels et al. 2019).
100% Free Headache Home Exercise Program
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Van Ettekoven et al. (2006) compared a craniocervical flexion training(CCFT) program with physiotherapy to physiotherapy alone in patients with chronic tension-type headaches. They found a decrease in headache frequency, duration, and intensity in the CCFT group at 6-week follow-up compared to the physiotherapy group. At 6 months follow-up, even after the intervention program had stopped, the effect regarding decreased headache frequency still remained significant.
Castien et al. (2011) have compared manual therapy (MT) interventions including spinal mobilization / manipulation of the cervical and thoracic spine, posture correction, and craniocervical exercises with usual care by a general practitioner in a group of patients with chronic TTH. They found a significantly larger reduction of headache frequency, disability, and increased cervical function in the MT group at 8 weeks follow-up Disability and cervical function While the difference in the primary outcome headache frequency was still significant at 26 weeks, disability and cervical function were not.
2 years later the authors examined which part of their MT intervention was effective (Castien et al. 2013). They found that increased neck flexor endurance appeared to be the working mechanism behind the MT intervention. An increase in cervical ROM and improved posture did not mediate the effect of decreased headache symptoms.
The same authors went on to examine if there is a relation between isometric neck flexor strength and the decrease of pressure-pain thresholds – an indicator for peripheral and central sensitization in patients with chronic TTH (Castien et al. 2015). Their results indicate that a decrease in PPT correlates with increases in isometric strength of neck flexors in patients with chronic TTH in the short- and long term.
In the case that neck endurance is reduced, you might want to try the following exercise program:
A small part of the intervention in the study of Castien et al. (2011) consisted of manual pressure techniques abbreviated as MTP, for which only anecdotal evidence is available as a treatment in isolation. In the following video we will show you 3 manual pressure techniques that can decrease pain and increase upper cervical range of motion.
MTP1:
Have your patient in prone position. If possible you can lower the head part of the bench so that the patient’s head is in slight flexion. This technique targets the ipsilateral rectus capitis posterior major. This muscle runs obliquely from the spinous process of C2 to the lateral part of the inferior nuchal line at the occiput.In order to reach the muscle, we will have to shift the trapezius muscle medially to reach underneath it. You can ask your patient to slightly lift his head to see the course of the trapezius. Inevitably, we will have to palpate through the splenius, which is only a thin muscle layer that still allows you to palpate through to the rectus capitis posterior major.
Now, apply pressure to this muscle with your thumb into medial and cranial direction toward its attachment. This will result in local and then referred pain to the head in patients with tension-type headaches. Hold the pressure for 20 to 60 seconds until the referred head pain has decreased, followed by a decrease in local pain until only local pressure remains. Afterwards, repeat the technique on the contralateral side as well.
MTP 2:
This technique combines compression of myofacial structures with a stretch of the rectus capitis posterior major.To conduct the technique have your patient in supine position and place your index or middle finger on the posterior tubercle of C1, which lies deep between the occiput and spinous process of C2. You can increase your pressure by putting another finger on top. Then gradually increase the tension in the contralateral rectus capitis posterior major by rotating the patients head towards you until submaximal pain is reported by the patient. This can again cause local and referred head pain in patients with tension-type headaches. You can fixate the rotation with your own belly or thigh, so it can be maintained in a submaximal position. Hold the pressure and the stretch 20 to 60 seconds until the referred head pain has decreased, followed by a decrease in local pain until only local pressure remains. Afterwards, repeat the technique on the contralateral side as well.
MTP3:
This technique is targeted at the upper cervical joints C1/C2 and C2/C3.To perform the technique for C1/C2 have your patient in supine lying position and support his head on your forearm. Then rotate the patient’s head 20 degrees away from you and place your thumb onto the ipsilateral arch of C1. Afterwards, rotate your patient’s head back until you feel the resistance on your thumb.Again, this technique will elicit local pain and referred pain to the head in patients with tension-type headaches. Hold the pressure and the stretch 20 to 60 seconds until the referred head pain has decreased, followed by a decrease in local pain until only local pressure remains.
In order to target C2/C3, rotate the patient’s head 30 degrees away from you. Then perform an upward slip movement at the ipsilateral facet joint of C2/C3 by exerting pressure on the ipsilateral arch of C2. Again, hold this position 20 to 60 seconds until first the referred head pain is diminished and the local pain has decreased as well until only local pressure remains.
Afterwards, repeat the technique on the contralateral side as well.
Unlike trigger point techniques, the manual pressure techniques are not targeted at painful taut bands in certain muscles.The goal is to elicit a nociceptive afferent stimulus to the upper cervical area that is innervated by the dorsal ramus of C2. This nociceptive stimulus has shown to activate supraspinal inhibiting systems like the periaqueductal gray (PAG) and the rostroventral medulla abbreviated as RVM. These structures can both inhibit nociception at the dorsal horn.Although pain is usually only decreased on short-term in approaches targeting the neurological system, anecdotal evidence shows that these techniques might have a long lasting effect.
Want to learn more about headaches? Then check out our following blogs & research reviews:
- Physical Tests for Headaches: Useful?
- The Efficacy of Aerobic Exercise vs. Strength Training in the Treatment of Migraine
- Podcast Episode 031: Headaches with René Castien
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Finally Learn how to Diagnose & Treat Patients with Headaches


What customers have to say about this online course
- Robbert Alblas13/09/24Headache Treatment in Clinical Practice Great insights
Very useful evidence based information. I do think this would be better if he would talk in his own language.Barry de Wit17/08/24Headache Treatment in Clinical Practice Review Headache Treatment in Clinical Practice
De cursus is erg duidelijk. Ook zijn de instructievideos wat betreft de tests en behandelingen erg nuttig om in de praktijk toe te passen! - Broes de Landsheer10/05/24Headache Treatment in Clinical Practice REVIEW COURSE HEADACHE
Iets te wetenschappelijk. Er worden heel veel artikels gegeven die je moet lezen en zo kom je aan het aantal uren studietijd. De video’s zijn echter zeer beknopt. Er worden ook geen slides gegeven van de video’s (je hebt dus geen naslagwerk).
Weinig praktisch toepasbaar vond ik.
Comment Physiotutors: Wij hebben inmiddels alle slides toegevoegdGoswin Arts-Opdam10/05/24Headache Treatment in Clinical Practice HEADACHE TREATMENT IN CLINICAL PRACTICE
Erg fijne en duidelijke cursus. Je krijgt genoeg handvatten mee en daarna kan je zelf bepalen welke je toepast in de praktijk. Ik kan patiënten met verschillende hoofdpijn nu in elk geval beter helpen. - Beppeke Molenaar14/04/24Headache Treatment in Clinical Practice OVERALL A GREAT COURSE
Great course, very informative.Tessa van der Zanden26/03/24Headache Treatment in Clinical Practice GOED TOEPASBARE CURSUS
Cursus die gelijk goed toepasbaar is in de praktijk. De Nederlandse ondertiteling is erg fijn. Goede balans tussen theorie en praktijk. Makkelijk in eigen tijd in te plannen en uit te voeren. - Bart de Ruijter20/03/24Headache Treatment in Clinical Practice LEUKE TOEPASSELIJKE CURSUS
Leuke toepasselijke cursus, nu ook vertaald in het Nederlands, wat het makkelijker maakt.
Filmpjes zijn wel in Engels, maar ondertiteling aan is een optie.
Goede combinatie van theorie, wetenschap en praktische handvaten.
Zeker een aanrader.Peter Tuyp27/02/24Headache Treatment in Clinical Practice GOOD COURSE
Good course, easy to follow.
Knowledge up to date after course. - Harmen van Delft25/02/24Headache Treatment in Clinical Practice INSTRUCTIEVE HOOFDPIJN CURSUS
de theoretische achtergrond en praktische vaardigheden zijn goed gecombineerd en bruikbaar in de praktijk.Laura Bradshaw05/02/24Headache Treatment in Clinical Practice GREAT CONTENT AND RESOURSES
The course was full of explanations, plenty of research and demonstrations. I would say that it took me longer than 14 hours to complete as I wanted to be thorough with my reading and practical component.
Rene and the physio tutors team were always available via email if you needed any info.
I would recommend this course if you want a better understanding of the management and manual therapy of headache and migraine. - Jelter Wahlen03/12/23Headache Treatment in Clinical Practice GREAT COURSE!
Great course to update your knowledge about headaches.
Evidence based and easy to implement in practice!Max Dienemann09/10/23Headache Treatment in Clinical Practice TOP
Great course! Everything is covered from diagnosis to treatment (-options) including the latest evidence backing everything up. The practical/skills videos on are also perfectly explained, therefore hands on skills and exercises can be easily implemented in daily practice. - Danitsja Wendt11/09/23Headache Treatment in Clinical Practice UITGEBREIDE HOOFDPIJNCURSUS
Veel informatie over de drie meest voorkomende hoofdpijnsoorten. Eerst uitgebreid theoretische achtergrond.
Daarna ook veel aandacht voor onderzoeken en behandelingen, verduidelijkt met filmpjes.
Fijn dat deze informatie ten alle tijden teruggekeken kan worden voor een opfrisser.
De cursus zelf is vertaald in het Nederlands, maar de vele wetenschappelijke artikelen zijn dat helaas niet.
Hierdoor ging bij mij wel erg veel tijd zitten in het doornemen daarvan.
Comment Physiotutors: All scientific literature is in English. That is a reality that we cannot change.Willem Nijssen31/07/23Headache Treatment in Clinical Practice GOOD QUALITY COURSE WITH UP-TO-DATE LITERATURE
The course is well structured and with up-to-date literature. It provides enough practical tips. There’s definitely a lot to learn about this subject! - Jesse de Louw11/07/23Headache Treatment in Clinical Practice GOOD COURSE
Good EBP study, with a nice variety of information. Sometimes a little bit hard to follow the information given in another language than my own. (Comment Physiotutors: This customer probably did not see the option to switch to Dutch)Hamad Alkahtani16/06/23Headache Treatment in Clinical Practice Very Interesting info and practical knowledge - M.A.G. Kuipers15/06/23Headache Treatment in Clinical Practice INFORMATIEVE CURSUS MBT HOOFDPIJN
Goede cursus, helaas niet in Nederlands en helaas zijn ook niet alle artikelen makkelijk te verkrijgen
duidelijke filmpjes met goede technieken mbt onderzoek en behandeling
Opmerking Physiotutors: De gehele cursus is wel in het Nederlands verkrijgbaar.Lennart Kroes17/04/23Headache Treatment in Clinical Practice A PERFECT COURSE TO UPDATE YOUR KNOWLEDGE ABOUT HEADACHE
Evidence-based, easy to follow. Perfect! - Erik Swarts09/03/23Headache Treatment in Clinical Practice GREAT COURSE!
First time doing a Physiotutors course. great way to learn on a high level of evidence. You can watch and rewatch everything for as long as you want before you take the exam.Daniel Klimsa31/01/23Headache Treatment in Clinical Practice GREAT COURSE!
Well-structured course with lots of evidence-based material.
Theory is well explained and you get a lot of additional reading material.
I would like to see improved quality of the explanations in the video portion of the course.