Frozen Shoulder / Adhesive Capsulitis | Diagnosis & Treatment

Frozen Shoulder / Adhesive Capsulitis | Diagnosis & Treatment
 Frozen shoulder (FS) is a poorly understood condition that typically involves substantial pain, movement restriction, and considerable morbidity. Although function improves over time, a full and pain-free range of motion may not be restored in everyone. Frozen shoulder is also known as adhesive capsulitis, however, the evidence for capsular adhesions is refuted and arguably this term should be abandoned (Lewis et al. 2015).
Frozen shoulder (FS) is a poorly understood condition that typically involves substantial pain, movement restriction, and considerable morbidity. Although function improves over time, a full and pain-free range of motion may not be restored in everyone. Frozen shoulder is also known as adhesive capsulitis, however, the evidence for capsular adhesions is refuted and arguably this term should be abandoned (Lewis et al. 2015).
FS can be differentiated into primary (idiopathic onset) and secondary onset. While primary FS does not have a known cause, secondary FS can further be distinguished into three different groups:
- Intrinsic: trauma, long-lasting immobilization, calcific tendinosis, rotator cuff, and biceps tendinopathy precede intrinsic secondary frozen shoulder with shoulder surgery resulting in iatrogenic intrinsic secondary frozen shoulder
- Extrinsic: When the condition is preceded by pathology remote from the shoulder such as AC joint arthritis, humeral or clavicular fractures, cervical radiculopathy, ipsilateral breast surgery, chest wall tumor CVAs
- Systemic secondary FS: diabetes, thyroid abnormalities, heart disease, genetic factors (such as Dupuytren’s), Parkinson’s disease, or epilepsy
Pietrzak et al. (2016) postulate that similar to DM and CVD, the inflammation and capsular fibrosis seen in FS might be precipitated by metabolic syndrome and chronic low-grade inflammation, which leads to an upregulation of pro-inflammatory cytokine production, sympathetic dominance of autonomic balance, and neuro-immune activation.
The disease process appears to be cytokine driven, which progresses from inflammation and hyperplasia of the synovium to capsular fibrosis with infiltration of chronic inflammatory cells and cytokines with a corresponding reduction of joint volume. At the same time, capsular fibrosis leads to the thickening of the long head of the biceps, coracohumeral ligament, and axillary recess.
An MRI study by Lee et al. (2012) confirmed this by showing that the coracohumeral ligament and the capsule in axillary recess were significantly greater in patients with Frozen Shoulder compared to a healthy control group.
Ryan et al. (2016) report that increased vascularity is a common feature described in histology studies, particularly in the anterosuperior structures but absent in the inferior structures with the exception of the axillary fold. This may also be an explanation for a patient’s pain experience as the literature consistently describes hypervascularity and angiogenesis as potential sources of nociception due to their association with neovessels.
Epidemiology
Primary FS in the general population is reported to affect 2 to 5.3% of patients during their lifetime.
The prevalence of secondary FS increased in patients with diabetes mellitus and thyroid disease from 4.3% to 38% (Kelley et al. 2013).
In most cases, FS occurs between ages 40 and 65 with a slightly higher prevalence among women compared to men (Tasto et al. 2007).
In Japan and China, FS is therefore called the 50-year-old shoulder due to the mean age of onset of 55.0±8.4 years for women and 54.7±8.7 years for men.
In 17% of all cases, FS is reported to occur on the contralateral side within five years after the first episode, while FS occurs bilaterally in 14% of all cases. Recurrence in the same shoulder are rare (Kelley et al. 2013).
At last, the literature describes that the non-dominant side is affected more often than the dominant side, although hard evidence is lacking (Lewis et al. 2015).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
- Pain in the shoulder, radiating into the upper arm, widespread and diffuse characteristic
- Onset: sudden or gradual with a progressive course regarding pain and stiffness
- Pain descriptions: constant, severe, unrelenting, excruciating pain when moved or jarred, occasional ‘neural-like symptoms
- Commonly reported problems: everything
- Commonly reported easing factors: nothing
- Medical history: DM, cardiovascular disease, smoking, high cholesterol, etc.
- Equal loss of active and passive range of motion
Examination
Hollmann et al. (2015) did a study on the amount of active muscle guarding in patients suspected to have FS and found that all patients had experienced a huge increase in passive abduction while under anesthesia. This means that the loss of range of motion in FS cannot only be explained by a true capsular contraction alone but that active stiffness or muscle guarding can play a huge role as well. For this reason, it can make sense to perform the Coracoid Pain Test to distinguish between a real and pseudo-Frozen Shoulder (Carbone et al. 2010)
Another orthopedic test to distinguish Frozen Shoulder from other shoulder pathologies is the Shoulder Shrug Sign.
WATCH TWO 100% FREE WEBINARS ON SHOULDER PAIN AND ULNA-SIDE WRIST PAIN

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
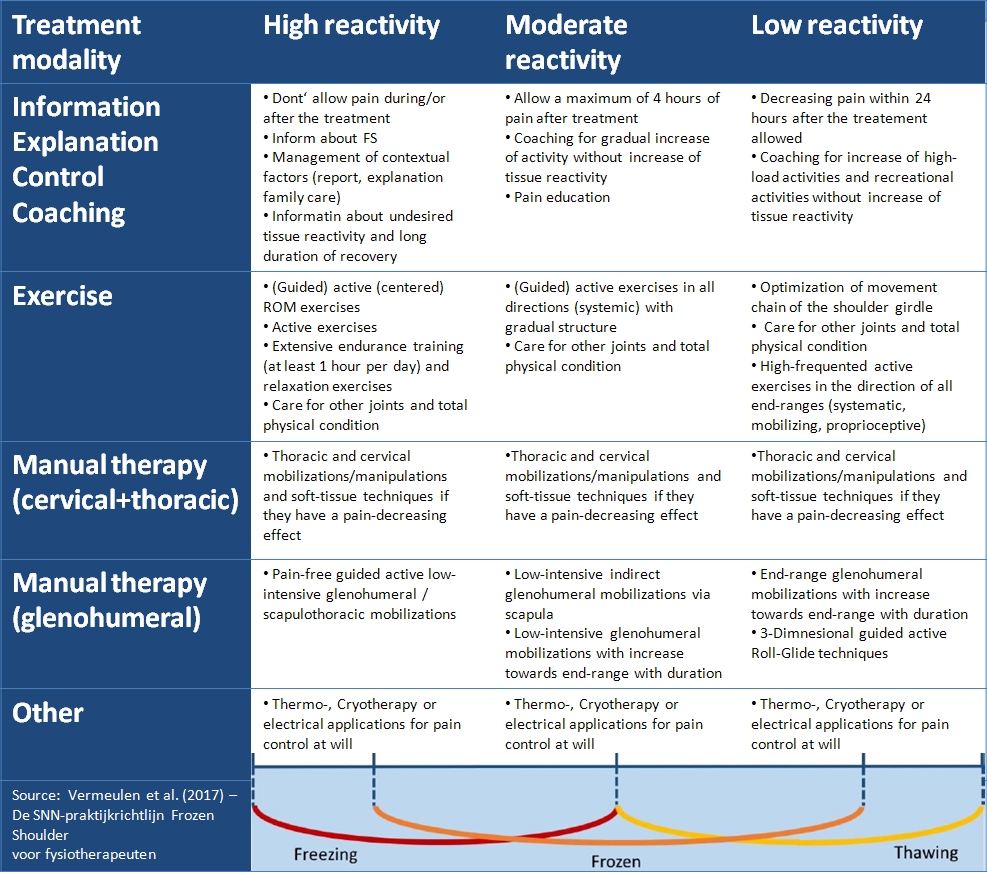
Physiotherapeutic treatment of FS should be tailored according to the degree of reactivity. The following table by the Dutch Shoulder Network aims to guide your treatment including recommended treatment options (Vermeulen et al. 2017).
A Cochrane review by Page et al. (2014) states that the most effective treatment for pain, function and self-reported treatment success in the early stages of a Frozen Shoulder is steroid injections.
While corticosteroid injections were superior to combined manual therapy and exercise in the short term (at 7 weeks), there was no clinically important difference after 6 months and 1 year.
Although steroid injections are an effective treatment in the short term, they may not provide any benefit in the long term (Xiao et al. 2017)
An alternative to corticosteroid injections is hydro-distension injections that inject a high-volume saline solution of 40-50cc combined with steroids and local anesthetics into the joint capsule.
There is moderate level evidence that arthrographic distension with saline and steroid provides short-term benefits in pain, range of movement, and function in adhesive capsulitis. However, it is uncertain whether this is better than alternative interventions (Buchbinder et al. 2008).
The last option for Frozen Shoulder Treatment is manipulation under anesthesia and arthroscopic capsular release. Unfortunately, there is only low-quality evidence available is low that demonstrates little benefit for a capsular release instead of, or in addition to manipulation under anesthesia in terms of abduction, flexion, and external rotation range of motion (Grant et al. 2013). At the same time complications have been reported for both procedures such as shoulder dislocation, rotator cuff tear, or brachial plexus palsy (Birch et al. 1991).
Do you want to learn more about Frozen Shoulder? Then check out the following research review:
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Increase your confidence in assessing and treating the Stiff Shoulder

What customers have to say about this course
- Senne Gabriëls30/12/24A complete understanding of elbow pathologies and management Very broad explanation of al the possible differential diagnosis and nice comprehensive management strategies with a big catalogue of exercises.Barbara14/12/24Really good Like always, perfect support to learn at your own rythm.
clear explanations and evidence based.
Thank you - Mika Tromp06/12/24Nice course! Explained the difference between osteoarthritis and rheumatoid arthritis nicely. Learned a few new things to use in clinical reasoning as well.Anneleen Peeters03/04/24Upper Limb Focus - The Wrist & Hand GREAT CONTENT!
Very happy with the way the course is presented; part videos, text and quizzes.
Great teachers, great refresher on the anatomy. - Dominik Meier01/04/24The Upper Limb Focus: Wrist & Hand CLINICALLY RELEVANT AND VERY WELL STRUCTURED COURSE!
This course is clinically relevant and very well structured. The wrist and hand is a very complex topic which has been described in a comprehensive and logical way. I can really recommend it. I like the theory and especially the cases. Thank you!Lieselot Longé29/12/23Upper Limb Focus - The Stiff Shoulder GOEDE CURSUS OM THUIS OP EIGEN TEMPO TE BEKIJKEN!
Dit is de 2de cursus die ik volg via physiotutors en net als de vorige cursus vond ik ook deze zeer leerrijk. Je krijgt dankzij deze cursus nieuwe inzichten in de behandeling van een stijve schouder. Er worden behandeltechnieken (o.a. mobilization with movement) getoond via video’s. Het leuke is ook dat je de cursus op je eigen tempo thuis kan volgen en na het afronden van de cursus kan je er nog steeds naar terug grijpen. Ik kijk ernaar uit om nog andere cursussen van physiotutors te ontdekken en raadt het ook anderen ten zeerste aan!. - Mieke Versteeg01/12/22Upper Limb Focus - The Elbow Inhoudelijk kwalitatief zeer hoogstaand.
Nog betere vertaling naar Nederlands zou toegevoegde waarde zijn.
Hulp per mail/telefonisch op ieder moment aanwezig/bereikbaar.



