Cluster Headache | Diagnosis & Treatment All you need to know

Cluster Headache | Diagnosis & Treatment All you need to know
Introduction & Epidemiology
Headaches can manifest on their own but are also a very common symptom in neck pain patients as more than 60% of patients with a primary neck pain complaint report having concordant episodes of neck pain. Therefore it’s essential to find out what kind of headache the patient is suffering from.
To start off let’s differentiate between primary and secondary types of headaches. But what does this mean? Simply put, primary headaches are a “disease themselves” whereas, in secondary headaches, the headache is a symptom of another condition. So primary headaches would be migraines, tension-type headaches & cluster headaches. Secondary type headaches are headaches caused by tumors, hemorrhage, other trauma, TMJ dysfunction, substance overdose, or neck pain aka. The cervicogenic headache.
Now let’s take a closer look at cluster headaches, which are primary types of headaches.
Fischera et al. (2008) conducted a meta-analysis to assess the lifetime prevalence of cluster headache and found low numbers of 0,12% with a 1-year prevalence of 53 per 100,000 persons and the overall sex ratio was 4.3 (male to female). Cluster headache had a 1-year prevalence of 0,054% among the working-aged population in a Swedish cohort (Manzoni et al. 2019)
Epidemiology
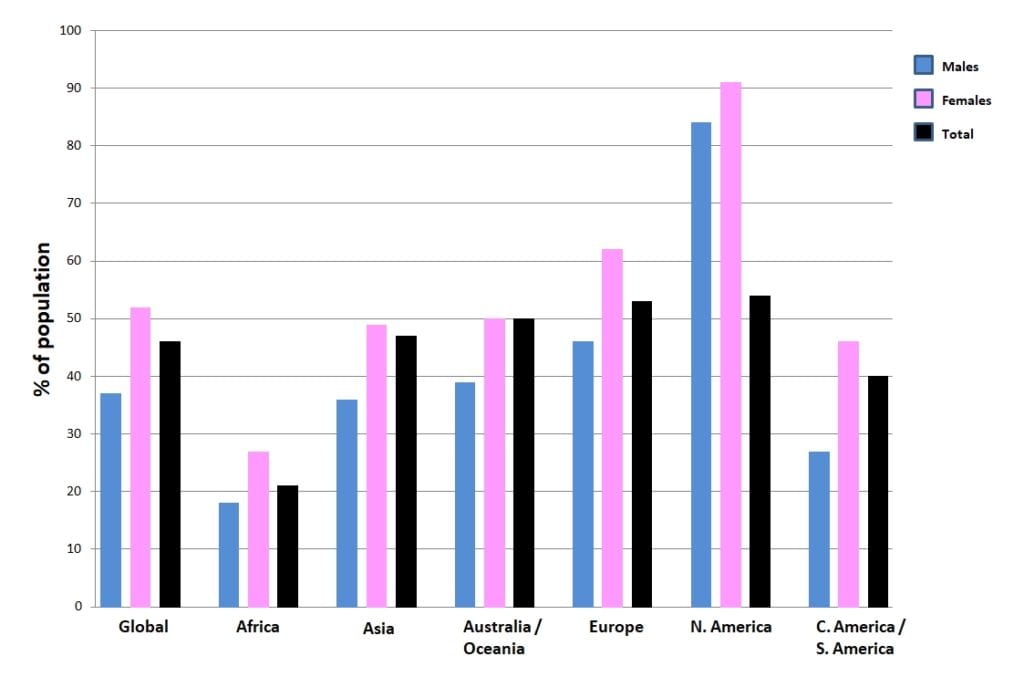
The following figure shows the prevalence of headaches on different continents around the world:
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
In order for a headache to qualify as a cluster headache it has to fulfill certain criteria (ICHD-III):
A. At least five attacks need to fulfill criteria B-D
B. An untreated episode lasts 15-180 minutes and shows severe or very severe unilateral orbital, supraorbital, and/or temporal pain
C. It matches either or both of the following:
- at least one of the following signs and symptoms, ipsilateral to the headache:
– conjunctival injection and/or lacrimation
– nasal congestion and/or rhinorrhoea
– eyelid edema– forehead and facial sweating
– miosis and/or ptosis - a sense of restlessness or agitation. There are reports of patients pacing back and forth through the room, banging their heads due to the severe pain.
D. It occurs with a frequency between one every other day and 8 per day
100% Free Headache Home Exercise Program
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Treatment for cluster headache consists of medication, injections/suboccipital nerve blocks, or intracranial stimulation. We can distinguish between treatment for acute attack and preventative treatment as two facets of cluster headache management. Unfortunately, there are currently no options for physiotherapists to treat patients with cluster headaches.
Currently, only a case study has been published on the combination of endogenous neurostimulation and physiotherapy (Navarro-Fernández et al. 2019).
Acute
100% oxygen therapy is arguably the most well-known method of treating cluster headaches (Obermann et al. 2015). As compared to other types of headaches, cluster headaches are the only condition for which this strategy is a level A recommendation. A minimum of 66% of patients benefit from oxygen therapy. It takes less than ten minutes to take effect. Using oxygen has no risks or adverse effects, making it a great option for treatment. Sadly, oxygen therapy for those with cluster headaches—which can be challenging to obtain—is frequently not covered by insurance.
The only other level A-indicated therapy is triptans. Subcutaneous sumatriptan or nasal spray zolmitriptan delivery of these medications are both options (May et al. 2006). If subcutaneous injections are not tolerated, intranasal triptans might be given on the side opposite the headache. Intranasal sumatriptan (20 mg) and intranasal zolmitriptan (5 mg) are two options. As the onset period of oral medications, in whatever form, is frequently longer than the headache, they are not advised.
Alternative treatments include octreotide, ergotamine, and intranasal lidocaine (with a reported 33% response) (Matharu et al. 2004). Sadly, medication resistance develops in 10% to 20% of people with severe cluster headaches. Patients should be advised to stay away from triggers, particularly alcohol. Patients should be urged to cease smoking even though there is no evidence to suggest that doing so will reduce their likelihood of getting headaches.
Preventive Medicine
The sole tier A suboccipital blockade is advised as a method of cluster headache avoidance. Negative side effects include temporary injection site soreness and mild headaches, both of which are not significant.
The most frequently prescribed prophylactic medication is verapamil (May 2003).
For patients with persistent cluster headaches and those who have episodic cluster headaches for at least two months, it is advised as the first line of preventive treatment (Obermann et al. 2015).
For episodic and persistent cluster headaches, verapamil, which is useful as a preventive medication, is started at 240 mg once daily (Leone et al. 2000). It is advised to perform routine ECGs to check on a patient’s heart health while they are taking this medication. Verapamil has a level C recommendation, despite being widely used by healthcare professionals.
Lithium, valproic acid, melatonin, and intranasal capsaicin are some more pharmaceutical choices (Ekbom et al. 2002).
The effects of electrical stimulation have been extensively studied. The sphenopalatine ganglion, occipital, and vagus nerve are among the areas that are stimulated. The hypothalamus has benefited greatly from deep brain stimulation, which has been particularly effective in treating patients who are drug-resistant (Fontaine et al. 2010). A non-implanted device may offer the option of vagus nerve stimulation (Goadsby et al. 2018).
Want to learn more about headaches? Then check out our following blogs & research reviews:
- Physical Tests for Headaches: Useful?
- The Efficacy of Aerobic Exercise vs. Strength Training in the Treatment of Migraine
- Podcast Episode 031: Headaches with René Castien
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Finally Learn how to Diagnose & Treat Patients with Headaches


What customers have to say about this online course
- Robbert Alblas13/09/24Headache Treatment in Clinical Practice Great insights
Very useful evidence based information. I do think this would be better if he would talk in his own language.Barry de Wit17/08/24Headache Treatment in Clinical Practice Review Headache Treatment in Clinical Practice
De cursus is erg duidelijk. Ook zijn de instructievideos wat betreft de tests en behandelingen erg nuttig om in de praktijk toe te passen! - Broes de Landsheer10/05/24Headache Treatment in Clinical Practice REVIEW COURSE HEADACHE
Iets te wetenschappelijk. Er worden heel veel artikels gegeven die je moet lezen en zo kom je aan het aantal uren studietijd. De video’s zijn echter zeer beknopt. Er worden ook geen slides gegeven van de video’s (je hebt dus geen naslagwerk).
Weinig praktisch toepasbaar vond ik.
Comment Physiotutors: Wij hebben inmiddels alle slides toegevoegdGoswin Arts-Opdam10/05/24Headache Treatment in Clinical Practice HEADACHE TREATMENT IN CLINICAL PRACTICE
Erg fijne en duidelijke cursus. Je krijgt genoeg handvatten mee en daarna kan je zelf bepalen welke je toepast in de praktijk. Ik kan patiënten met verschillende hoofdpijn nu in elk geval beter helpen. - Beppeke Molenaar14/04/24Headache Treatment in Clinical Practice OVERALL A GREAT COURSE
Great course, very informative.Tessa van der Zanden26/03/24Headache Treatment in Clinical Practice GOED TOEPASBARE CURSUS
Cursus die gelijk goed toepasbaar is in de praktijk. De Nederlandse ondertiteling is erg fijn. Goede balans tussen theorie en praktijk. Makkelijk in eigen tijd in te plannen en uit te voeren. - Bart de Ruijter20/03/24Headache Treatment in Clinical Practice LEUKE TOEPASSELIJKE CURSUS
Leuke toepasselijke cursus, nu ook vertaald in het Nederlands, wat het makkelijker maakt.
Filmpjes zijn wel in Engels, maar ondertiteling aan is een optie.
Goede combinatie van theorie, wetenschap en praktische handvaten.
Zeker een aanrader.Peter Tuyp27/02/24Headache Treatment in Clinical Practice GOOD COURSE
Good course, easy to follow.
Knowledge up to date after course. - Harmen van Delft25/02/24Headache Treatment in Clinical Practice INSTRUCTIEVE HOOFDPIJN CURSUS
de theoretische achtergrond en praktische vaardigheden zijn goed gecombineerd en bruikbaar in de praktijk.Laura Bradshaw05/02/24Headache Treatment in Clinical Practice GREAT CONTENT AND RESOURSES
The course was full of explanations, plenty of research and demonstrations. I would say that it took me longer than 14 hours to complete as I wanted to be thorough with my reading and practical component.
Rene and the physio tutors team were always available via email if you needed any info.
I would recommend this course if you want a better understanding of the management and manual therapy of headache and migraine. - Jelter Wahlen03/12/23Headache Treatment in Clinical Practice GREAT COURSE!
Great course to update your knowledge about headaches.
Evidence based and easy to implement in practice!Max Dienemann09/10/23Headache Treatment in Clinical Practice TOP
Great course! Everything is covered from diagnosis to treatment (-options) including the latest evidence backing everything up. The practical/skills videos on are also perfectly explained, therefore hands on skills and exercises can be easily implemented in daily practice. - Danitsja Wendt11/09/23Headache Treatment in Clinical Practice UITGEBREIDE HOOFDPIJNCURSUS
Veel informatie over de drie meest voorkomende hoofdpijnsoorten. Eerst uitgebreid theoretische achtergrond.
Daarna ook veel aandacht voor onderzoeken en behandelingen, verduidelijkt met filmpjes.
Fijn dat deze informatie ten alle tijden teruggekeken kan worden voor een opfrisser.
De cursus zelf is vertaald in het Nederlands, maar de vele wetenschappelijke artikelen zijn dat helaas niet.
Hierdoor ging bij mij wel erg veel tijd zitten in het doornemen daarvan.
Comment Physiotutors: All scientific literature is in English. That is a reality that we cannot change.Willem Nijssen31/07/23Headache Treatment in Clinical Practice GOOD QUALITY COURSE WITH UP-TO-DATE LITERATURE
The course is well structured and with up-to-date literature. It provides enough practical tips. There’s definitely a lot to learn about this subject! - Jesse de Louw11/07/23Headache Treatment in Clinical Practice GOOD COURSE
Good EBP study, with a nice variety of information. Sometimes a little bit hard to follow the information given in another language than my own. (Comment Physiotutors: This customer probably did not see the option to switch to Dutch)Hamad Alkahtani16/06/23Headache Treatment in Clinical Practice Very Interesting info and practical knowledge - M.A.G. Kuipers15/06/23Headache Treatment in Clinical Practice INFORMATIEVE CURSUS MBT HOOFDPIJN
Goede cursus, helaas niet in Nederlands en helaas zijn ook niet alle artikelen makkelijk te verkrijgen
duidelijke filmpjes met goede technieken mbt onderzoek en behandeling
Opmerking Physiotutors: De gehele cursus is wel in het Nederlands verkrijgbaar.Lennart Kroes17/04/23Headache Treatment in Clinical Practice A PERFECT COURSE TO UPDATE YOUR KNOWLEDGE ABOUT HEADACHE
Evidence-based, easy to follow. Perfect! - Erik Swarts09/03/23Headache Treatment in Clinical Practice GREAT COURSE!
First time doing a Physiotutors course. great way to learn on a high level of evidence. You can watch and rewatch everything for as long as you want before you take the exam.Daniel Klimsa31/01/23Headache Treatment in Clinical Practice GREAT COURSE!
Well-structured course with lots of evidence-based material.
Theory is well explained and you get a lot of additional reading material.
I would like to see improved quality of the explanations in the video portion of the course.