Cervicogenic Headache | Diagnosis & Treatment for Physios

Cervicogenic Headache | Diagnosis & Treatment for Physios
Introduction & Epidemiology
Headaches can manifest on their own but are also a very common symptom in neck pain patients as more than 60% of patients with a primary neck pain complaint report having concordant episodes of neck pain. Therefore it’s essential to find out what kind of headache the patient is suffering from.
To start off let’s differentiate between primary and secondary types of headaches. But what does this mean? Simply put, primary headaches are a “disease themselves” whereas, in secondary headaches, the headache is a symptom of another condition. So primary headaches would be migraines, tension-type headaches & cluster headaches. Secondary type headaches are headaches caused by tumors, hemorrhage, other trauma, TMJ dysfunction, substance overdose, or neck pain aka. The cervicogenic headache.
Now let’s take a closer look at cervicogenic headache, which is a secondary type of headache.
Epidemiology
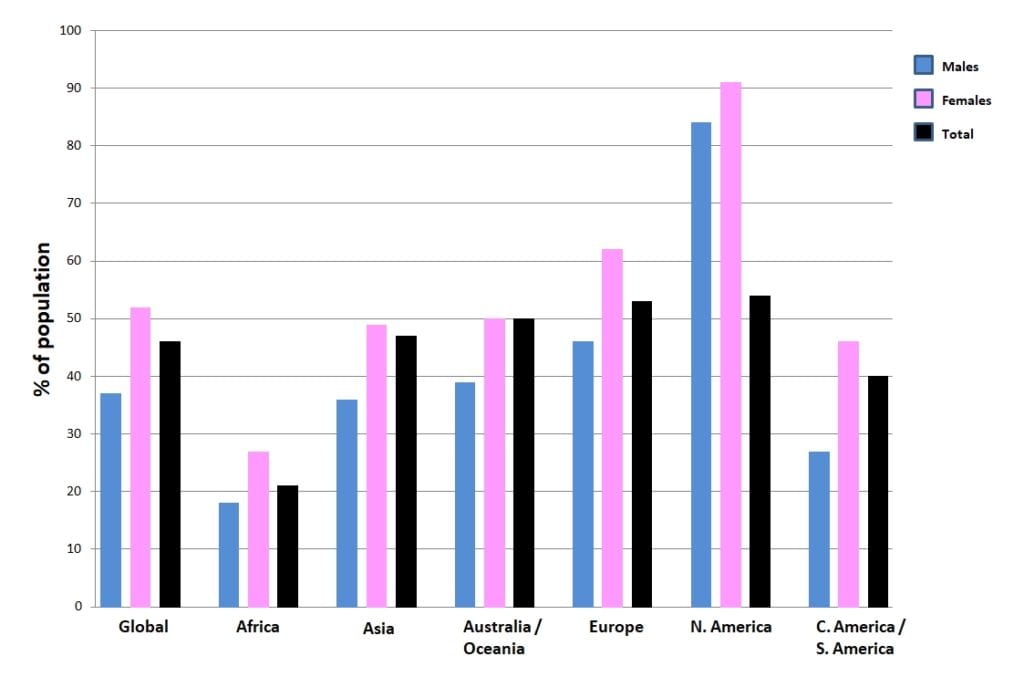
The following figure shows the prevalence of headache on different continents around the world:
Other studies on the prevalence of CGH have reported a prevalence range between 0,17 – 4,1% (Knackstedt et al. 2010; Antonaci et al. 2011; Sjaastad et al. 2008).
But how can the neck refer pain to the head?
In the case of referred pain, pain is perceived in a region other than the site of the painful stimulus. Thus, pressure or load on the place where the pain is felt usually does not lead to an increase in pain intensity. However, pressure or load on the place of the sensitized nociceptors results in an increase in pain intensity in the referred area. In the case of cervicogenic headache, nociception in the structures of the neck leads to referred pain in the head.
If we follow the convergence-projection theory outlined in our other video, we first need a structure responsible for nociception in the high cervical area that has a low density of nociceptive afferent innervation. These are usually structures that are lying deep, such as the facet joints including their joint capsules at C2/C3 or the alar ligaments reaching from the dens of C2 to the occiput for example. The afferent innervation of those structures converges on the second-order neuron in the dorsal horn at the height of C1/C2.
At the same time, our face has a very high density of afferent nociceptive innervation and receives sensory innervation from cranial nerve number 5 – the trigeminal nerve. The trigeminal nerve in turn converges onto the second-order neuron in the trigeminal nerve nucleus, which is the largest cranial nerve nucleus. It extends from the midbrain, to the pons and medulla into the spinal cord until C1/C2. So the trigeminal nerve’s innervation and the innervation of deep structures of the upper cervical spine converge onto the same spinal segment.
So when the afferent nociceptive stimulus from the neck, travels to the second-order neuron in the dorsal horn at segment C1/C2 and finally reaches the somatosensory cortex, this part of the brain then has to figure out the origin of the stimulus. In this case, the brain makes a projection error and decides that the nociceptive stimulus must be coming from the area with the higher nociceptive afferent innervation, which is the face rather than the poorly innervated upper cervical area. In other words, the brain projects pain into the fronto-orbital area of the head.

If the whole face is innervated by the trigeminal nerve, why do we only feel headaches in the frontal-orbital area and not the cheek and the jaw? The trigeminal nerve splits into 3 different branches, which are:
- The ophthalmic nerve supplying the scalp, forehead, and orbital area amongst others
- The maxillary nerve supplying the cheek, upper lip, and upper teeth amongst others
- The mandibular nerve supplying the lower lip, chin and jaw up to the temporal area
When those 3 nerve branches reach the trigeminal nerve nucleus, they are inverted. Remember that the trigeminal nerve nucleus is large and it consists of three different subparts. The mandibular and maxillary nerves converge onto the pars oralis and pars interpolaris of the trigeminal nerve nucleus respectively, which both don’t reach as far caudal as the spinal cord. Only the ophthalmic nerve converges onto the pars caudalis of the trigeminal nerve nucleus which is located in the spinal cord at the height of C1/C2, exactly where the afferents from structures in the upper cervical spine converge.
It’s important to mention that we are talking about unilaterally innervated structures of the neck and face. So referred pain from the structures of the neck on the right for example will always lead to headache on the right side and the left side will refer to the left side.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Picture & Examination
In order for a headache to qualify as a cervicogenic headache it has to fulfill certain criteria (ICHD-III):
First and foremost, there will be clinical, laboratory, and or imaging evidence of a disorder or lesion in the cervical region known to be able to cause headaches such as for example the facet joints or certain muscles.
Furthermore, at least two of the following criteria have to apply:
- The headache has developed after the onset of the cervical disorder or lesion. So patients will probably describe a trauma during patient history.
- The headache improves or resolves in parallel with the improvement and/or resolution of the cervical disorder or lesion
- Cervical range of motion is reduced, the pain is movement/posture dependent and the headache is made significantly worse by provocative testing. For example, decreased upper cervical spine rotation as assessed by the flexion rotation test can be linked to cervicogenic headache
- The headache is abolishe after diagnostic blockade of a cervical structure or its nerve supply
Next to the ICDH-III criteria, Sjaastad et al. (2008) have proposed the following criteria to classify a headache as cervicogenic:
- Provocation: unphysiological neck positions
- Provocation externally, neck
- Reduced range of motion in the neck ( ≥ 10 degrees deficit)
- Shoulder pain ipsilateral
- Arm pain, ipsilateral
- Unilateral headache (without side shift)
- Onset posteriorly in the neck/occipital area
Examination
Compared with healthy controls, the average patient with cervicogenic headaches differs on provocation, cervical range of motion (including the flexion-rotation test), and neck muscle endurance.
The goal of provocation tests is to recreate the patient’s familiar pain. This way, you are able to confirm the location of nociception in the cervical structures, possibly leading to referred pain to the head. Cervicogenic headache can be provoked with the following technique:
Passive assessment of the quantity and quality of segmental intervertebral motion, also known as motion palpation, is part of the diagnostic clinical expertise of manual practitioners to guide decisions on a therapeutic strategy for patients with spinal pain
Hypomobility indicates mobilizing interventions while hypermobility calls for a stabilizing approach. A systematic review done by van Trijffel et al. (2005) evaluated the reliability of passive segmental assessment of the cervical spine and found an overall reliability of poor to fair. However, for segments C1/C2 and C2/C3 at least fair reliability was reached consistently. For this reason, we give this examination a moderate clinical value.
In order to perform regional range of motion assessment for upper cervical spine flexion of vertebrae’s C0 til C3 have your patient sit upright at the edge of the bench or on a stool, the bench height should be adjusted so that your patient’s head is at the same height as your belly.
First, fixate the spinous process of C3 with a key grip into a ventrocranial direction. Be aware that this is the other way around than in other parts of the spine due to the ligamentous connections of the upper cervical spine.
Then your working hand is placed low on the patient’s occiput and the patient’s head is fixated between your working hand and chest. Now perform a maximal heteronymous 3D movement with equal components of flexion, contralateral lateral flexion, and ipsilateral rotation.
For the regional assessment of upper cervical spine extension, change your fixation of C3 into ventrocaudal direction and place your working hand higher on the patient’s occiput. Then perform a maximal heteronymous 3D movement with equal components of extension, contralateral lateral flexion, and ipsilateral rotation.
Both movements are judged on resistance during motion and at end range, range of motion, as well as possible pain provocation compared to the other side.
For upper cervical spine assessment be aware that a limitation at C2/C3 can influence the movement of the higher segments for this reason C2/C3 has to be assessed first. A limitation of C0/C1 can limit the movement of C1/C2. For this reason, we will start with the segmental assessment of C0/C1 first.
First, fixate your patient’s spinous process C2 with a key grip. Then place your hypothenar eminence on the patient’s mastoid process on the contralateral side and fixate the patient’s head with your chest. Then rotate your patient’s head until you feel resistance.
To assess movement at C0/C1 perform a lateral flexion movement to the contralateral side by a coupled movement between your working hand and your chest. The movement has to take place around a sagittal axis through the nose of your patient. Furthermore, you can specify if the limitation lies on the contralateral or the ipsilateral condyle of the occiput to pronounce the downslip movement of the contralateral condyle of C0 (condyle on the side of your working hand) and perform the same lateral flexion movement with C0/C1 in extension.
To pronounce the upslip movement of the ipsilateral condyle of C0 (side of your chest) perform the same lateral movement with C0/C1 in flexion.
For the assessment of C1/C2 keep your fixation and move the hypothenar eminence of your working hand down to the contralateral arch of C1. Your patient’s head is in neutral position and no lateral flexion is present. Then rotate maximally and assess the end feel. Both movements are judged on resistance during motion, end-feel, as well as possible pain provocation, compared to the other side.
Upper cervical range of motion in the direction of rotation can be reliably and accurately assessed with the Flexion-Rotation Test (Hall et al. 2010a, Ogince et al. 2007, Hall et al 2010b). This test – is positive – can give you an indication of limited rotation on segments C1/C2. In turn, hypomobility on C0/C1 or C2/C3 can lead to this limitation in rotation on C1/C2.So in case of a positive test, we still need to perform intervertebral motion assessment of all upper cervical segments in order to find the dysfunctional segment.
Although no clear cut-off values are given, the performance time can give an indication of neck flexor endurance:
100% Free Headache Home Exercise Program
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
Jull et al. (2002) compared the effects of cervical joint mobilization / manipulation to low-load endurance exercises to train muscles of the cervicoscapular region versus the combination of both interventions. They found that all three interventions were equally effective in the reduction of headache frequency, intensity, and duration at a follow-up of 7 weeks (directly post-intervention), 3, 6, and 12 months. Although there was no statistical evidence of an additive effect from the treatments, there were some different effects of the interventions on some outcomes, and 10% more participants receiving the combined therapy obtained good and excellent outcomes.
Mobilization exercises are identical to the PIVM assessment, but can be done in supine position as well in order to have the patient relax as much as possible:
Want to learn more about headaches? Then check out our following blogs & research reviews:
- Physical Tests for Headaches: Useful?
- The Efficacy of Aerobic Exercise vs. Strength Training in the Treatment of Migraine
- Podcast Episode 031: Headaches with René Castien
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Finally Learn how to Diagnose & Treat Patients with Headaches


What customers have to say about this online course
- Robbert Alblas13/09/24Headache Treatment in Clinical Practice Great insights
Very useful evidence based information. I do think this would be better if he would talk in his own language.Barry de Wit17/08/24Headache Treatment in Clinical Practice Review Headache Treatment in Clinical Practice
De cursus is erg duidelijk. Ook zijn de instructievideos wat betreft de tests en behandelingen erg nuttig om in de praktijk toe te passen! - Broes de Landsheer10/05/24Headache Treatment in Clinical Practice REVIEW COURSE HEADACHE
Iets te wetenschappelijk. Er worden heel veel artikels gegeven die je moet lezen en zo kom je aan het aantal uren studietijd. De video’s zijn echter zeer beknopt. Er worden ook geen slides gegeven van de video’s (je hebt dus geen naslagwerk).
Weinig praktisch toepasbaar vond ik.
Comment Physiotutors: Wij hebben inmiddels alle slides toegevoegdGoswin Arts-Opdam10/05/24Headache Treatment in Clinical Practice HEADACHE TREATMENT IN CLINICAL PRACTICE
Erg fijne en duidelijke cursus. Je krijgt genoeg handvatten mee en daarna kan je zelf bepalen welke je toepast in de praktijk. Ik kan patiënten met verschillende hoofdpijn nu in elk geval beter helpen. - Beppeke Molenaar14/04/24Headache Treatment in Clinical Practice OVERALL A GREAT COURSE
Great course, very informative.Tessa van der Zanden26/03/24Headache Treatment in Clinical Practice GOED TOEPASBARE CURSUS
Cursus die gelijk goed toepasbaar is in de praktijk. De Nederlandse ondertiteling is erg fijn. Goede balans tussen theorie en praktijk. Makkelijk in eigen tijd in te plannen en uit te voeren. - Bart de Ruijter20/03/24Headache Treatment in Clinical Practice LEUKE TOEPASSELIJKE CURSUS
Leuke toepasselijke cursus, nu ook vertaald in het Nederlands, wat het makkelijker maakt.
Filmpjes zijn wel in Engels, maar ondertiteling aan is een optie.
Goede combinatie van theorie, wetenschap en praktische handvaten.
Zeker een aanrader.Peter Tuyp27/02/24Headache Treatment in Clinical Practice GOOD COURSE
Good course, easy to follow.
Knowledge up to date after course. - Harmen van Delft25/02/24Headache Treatment in Clinical Practice INSTRUCTIEVE HOOFDPIJN CURSUS
de theoretische achtergrond en praktische vaardigheden zijn goed gecombineerd en bruikbaar in de praktijk.Laura Bradshaw05/02/24Headache Treatment in Clinical Practice GREAT CONTENT AND RESOURSES
The course was full of explanations, plenty of research and demonstrations. I would say that it took me longer than 14 hours to complete as I wanted to be thorough with my reading and practical component.
Rene and the physio tutors team were always available via email if you needed any info.
I would recommend this course if you want a better understanding of the management and manual therapy of headache and migraine. - Jelter Wahlen03/12/23Headache Treatment in Clinical Practice GREAT COURSE!
Great course to update your knowledge about headaches.
Evidence based and easy to implement in practice!Max Dienemann09/10/23Headache Treatment in Clinical Practice TOP
Great course! Everything is covered from diagnosis to treatment (-options) including the latest evidence backing everything up. The practical/skills videos on are also perfectly explained, therefore hands on skills and exercises can be easily implemented in daily practice. - Danitsja Wendt11/09/23Headache Treatment in Clinical Practice UITGEBREIDE HOOFDPIJNCURSUS
Veel informatie over de drie meest voorkomende hoofdpijnsoorten. Eerst uitgebreid theoretische achtergrond.
Daarna ook veel aandacht voor onderzoeken en behandelingen, verduidelijkt met filmpjes.
Fijn dat deze informatie ten alle tijden teruggekeken kan worden voor een opfrisser.
De cursus zelf is vertaald in het Nederlands, maar de vele wetenschappelijke artikelen zijn dat helaas niet.
Hierdoor ging bij mij wel erg veel tijd zitten in het doornemen daarvan.
Comment Physiotutors: All scientific literature is in English. That is a reality that we cannot change.Willem Nijssen31/07/23Headache Treatment in Clinical Practice GOOD QUALITY COURSE WITH UP-TO-DATE LITERATURE
The course is well structured and with up-to-date literature. It provides enough practical tips. There’s definitely a lot to learn about this subject! - Jesse de Louw11/07/23Headache Treatment in Clinical Practice GOOD COURSE
Good EBP study, with a nice variety of information. Sometimes a little bit hard to follow the information given in another language than my own. (Comment Physiotutors: This customer probably did not see the option to switch to Dutch)Hamad Alkahtani16/06/23Headache Treatment in Clinical Practice Very Interesting info and practical knowledge - M.A.G. Kuipers15/06/23Headache Treatment in Clinical Practice INFORMATIEVE CURSUS MBT HOOFDPIJN
Goede cursus, helaas niet in Nederlands en helaas zijn ook niet alle artikelen makkelijk te verkrijgen
duidelijke filmpjes met goede technieken mbt onderzoek en behandeling
Opmerking Physiotutors: De gehele cursus is wel in het Nederlands verkrijgbaar.Lennart Kroes17/04/23Headache Treatment in Clinical Practice A PERFECT COURSE TO UPDATE YOUR KNOWLEDGE ABOUT HEADACHE
Evidence-based, easy to follow. Perfect! - Erik Swarts09/03/23Headache Treatment in Clinical Practice GREAT COURSE!
First time doing a Physiotutors course. great way to learn on a high level of evidence. You can watch and rewatch everything for as long as you want before you take the exam.Daniel Klimsa31/01/23Headache Treatment in Clinical Practice GREAT COURSE!
Well-structured course with lots of evidence-based material.
Theory is well explained and you get a lot of additional reading material.
I would like to see improved quality of the explanations in the video portion of the course.