Achilles Tendinopathy / Achilles Tendinitis | Diagnosis & Treatment

Achilles Tendinopathy / Achilles Tendinitis | Diagnosis & Treatment
Achilles tendinopathy is a common musculoskeletal condition characterized by localized Achilles tendon load-related pain and dysfunction. It is common in both athletic populations and sedentary people, and many suffer profound and longstanding impairments in activities such as walking and running (Turner et al. 2020).
Achilles tendinopathy affects approximately 9% of recreational runners and up to 5% of professional athletes, this condition is career-ending (Lysholm et al, 1987). The incidence of mid-portion Achilles tendinopathy in general practice within the adult population is 2.35 per 1000, and in 35% of cases, a relationship with sports activity has been recorded (de Jonge et al, 2011).
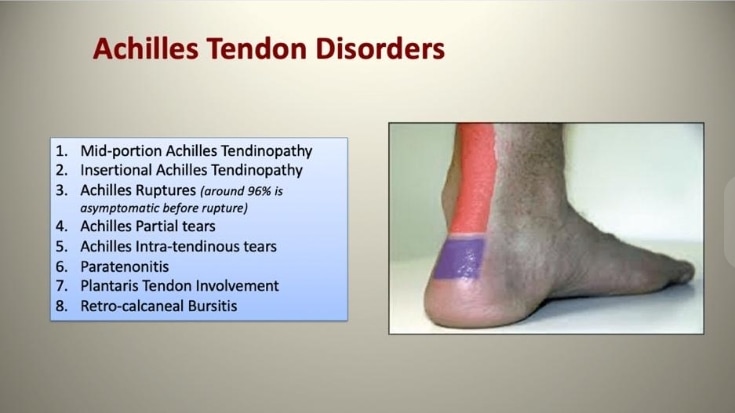
Achilles tendinopathy is a condition that results in the loss of normal collagen architecture, replaced with amorphous, mucinous material, hypercellularity, and increased glycosaminoglycans and neovascularization (Cook et al. 2009). The tendon can be affected within its mid-substance, typically 2cm to 6cm from the insertion point, or at the point of insertion itself.

Pathomechanism
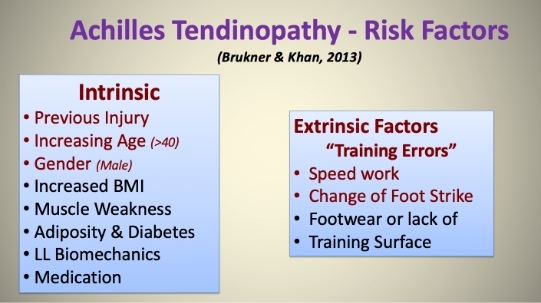
The high prevalence among runners points to mechanical overloading as an important etiological factor. Key risk factors include advanced age, male sex, high body mass index, hypercholesterolemia, and the presence of genetic variants of genes related to collagen mechanisms. The postulated intrinsic etiological factors include tendon vascularity, weakness, as well as lack of flexibility of gastrocnemius–soleus complex, pes cavus, and lateral ankle instability (Van Der Vlist et al. 2019).
Mechanical overload results in inflammation, although the inflammation is not a typical full-blown inflammation (Anderson et al. 2010). The tenocytes produce inflammatory mediators such as Substance P and Prostaglandin E2. The peritendinous region becomes filled with fibrinous exudate (perceived as crepitus) and forms adhesions. The imbalance between matrix degeneration and synthesis leads to intra-tendinous changes. The four cornerstones of histopathology are cellular activation/increase in cell numbers, increase in ground substance, collagen disarray, and neovascularization (Alfredson et al. 2007).
There is also evidence of neurogenic inflammation in the presence of neuropeptides such as Substance P and calcitonin gene-related peptides. The neural pathway may be associated with neovascularization. Biopsies have shown that nerves are in close relationship with neovascularization in areas of tendinosis (Bjur et al. 2005).
The pain mechanisms in tendinopathy are not clear but are thought to involve local nociception mediated by changes within the tenocytes (Rio et al. 2014). The etiology of chronic tendinopathy is complex and multifactorial. The current understanding is the imbalance between the load demands placed on the tendon and its capacity to remodel (Cook et al. 2009).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
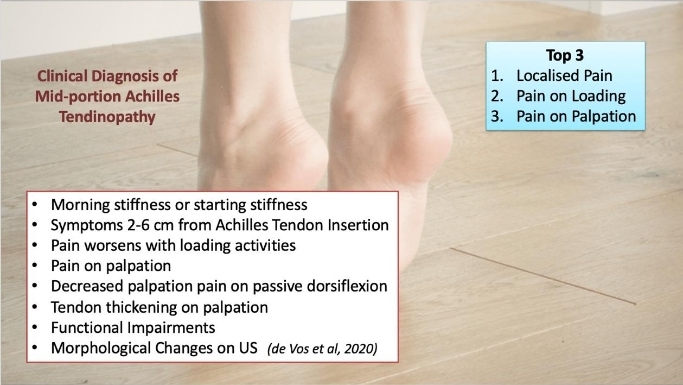
Clinical Presentation & Examination
The most common group presenting with non-insertional Achilles tendinopathy are athletes, especially middle to long-distance runners. A common symptom is morning stiffness or stiffness following a period of inactivity. As the condition progresses, pain may occur with even minor exertion and interfere with activities of daily living. In severe cases, pain persists at rest. In the acute phase, the tendon is diffusely swollen and oedematous and tenderness is usually greatest 2-6cm proximal to the tendon insertion. A tender nodular swelling can be present in chronic cases.
There are multiple causes of Achilles tendon pain as shown in the figure below:
For further information on the differential diagnosis of Achilles tendinopathy, watch the video below:
The patient is examined standing and prone with legs exposed from the knee downwards. The foot and heel should be examined for malalignment, deformity, obvious asymmetry, tendon size, localized thickening, and previous scars. The tendon excursion is examined to determine the tightness of the tendon. A swelling in the tendon due to pure tendinopathy will move with the tendon on movement of the ankle, conversely, swelling of the paratenon will not move (Arc test).
In the Royal London Hospital test, a swelling that is most painful when the ankle is in maximum dorsiflexion indicates tendinopathy. Maffulli et al. (2003) studied sensitivity and specificity of palpation, painful arc test, and Royal London Hospital test in 2003 and found that all three tests had good interobserver agreement.
A later study by Hutchinson et al. (2013), which studied ten clinical tests, found that only two tests, location of pain and pain on palpation, are the most reliable and accurate An overview of diagnostic tests for mid-portion Achilles tendinopathy is described in this video below:
Imaging
Imaging techniques include Ultrasound and Magnetic Resonance Imaging (MRI) scans. Ultrasound may be useful with power Doppler sonography, as Achilles tendinopathy seems to be related to areas of neovascularization. Multiple studies have shown equal or improved accuracy with ultrasound when compared with MRI scans in detecting tendinopathy (Khan et al. 2003). The advantage of ultrasonography over other imaging modalities is its interactive capability and cost-effectiveness.
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN – FOR FREE!

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
In general, non-operative care should be implemented for a minimum of six months prior to consideration for surgery.
Exercise Interventions
Exercise-based treatments that restore the load capacity of the tendon have become the primary management tool for the management of Achilles tendinopathy and are recommended in systematic reviews and clinical practice guidelines (Malliaras et al. 2013).
Eccentric exercise has been shown to be the most effective treatment for non-insertional Achilles tendinopathy. The specific form of exercise varies from trial to trial, but the principal goal is to provide a strong, controlled, mechanical force to the Achilles tendon. This is usually achieved through eccentric muscle activity; for instance, heel drop over a step. As patient tolerance of the exercise improves, the load can be progressively increased. In Alfredson’s protocol, which is the most commonly employed non-operative treatment method, exercises are performed in three sets of 15 repetitions, twice a day, for 12 weeks (Scott et al. 2011). The Alfredson Rehab protocol for Achilles Tendinopathy is described below
Other exercise protocols, such as eccentric-concentric, progressing to eccentric and eccentric-concentric, and heavy-slow resistance training have been described with similar success (Beyer et al. 2015).
A systematic review investigating exercise response (i.e., adaptative outcomes such as tendon stiffness) in healthy Achilles and patellar tendons concluded that load intensity is a key determinant of tendon tissue adaptation to load, and the type of contraction (e.g., eccentric versus concentric) did not influence adaptation (Bohm et al. 2015).
There is also evidence that longer-duration contractions at the same intensity result in greater Achilles tendon adaptation, most likely because there is a time-dependent transmission of external load to the tendon cytoskeleton and cells (Bohm et al. 2014).
In general, the overall trend suggests a positive effect of progressive loading with no reported major adverse side effects.
From a practical standpoint, it is important to match the exercise type and progression, based on the individual level of pain and tissue irritability. As stretch-shorten cycle exercises that store and release energy in the tendon are considered high load for patients, these activities need to be trained as well. Sancho et al. (2019) proposed the following hopping program:
Limitations of Exercises
Despite being recommended as first-line recommended treatment, the benefit from exercise is variable and inconsistent. A longitudinal study found 60% had continued pain and disability after 5 years despite exercise interventions, and 48% sought additional treatment including injections and surgery (van der Plas et al. 2012).
One potential reason for disparate outcomes of exercise for Achilles tendinopathy is poor knowledge about whether exercise parameters (i.e., different exercise doses) influence the outcome. Exploration of exercise dose response in Achilles tendinopathy is warranted. Knowing whether certain exercise parameters improve outcomes for Achilles tendinopathy management will assist in developing more effective exercise approaches (Malliaras et al. 2016)
Many parameters can be influenced in exercise prescription, including load intensity (e.g., repetition maximum [RM], maximal voluntary contraction), volume (repetitions and sets), and time under tension per contraction. However, it is important to acknowledge that whether these parameters that are important for tendon adaptation such as load intensity and duration of contraction (or time-under-tension) have a positive influence on pain and function in patients with Achilles tendinopathy has not been investigated, to date.
ESWT (Extra-corporeal Shock Wave Therapy)
This forms the second-line management in chronic Achilles tendinopathy. The RCT study that compared ESWT with eccentric training showed favorable outcomes, with 60%of patients showing improvement with a similar outcome to eccentric exercise and both groups were better than the “wait and see” subset (Rompe et al. 2007).
Rompe et al. (2007) showed eccentric strengthening plus repetitive low-energy shock-wave therapy was better than eccentric strengthening alone. There was a significant improvement in combined therapy than strengthening group alone.EWST is normally performed three times, spaced one week apart, 2000 pulses with a pressure of 2.5 bars and a frequency of eight pulses per second in an area of maximal tenderness in a circumferential pattern.The clinical response to shockwave is linked to two aspects, one is tissue healing with an increased level of tissue healing factors and the other is pain transmission modulation by selective dysfunction of sensory unmyelinated nerve fibers, either directly or through neuropeptides (Chen et al. 2004).
Topical application of Glyceryl trinitrate
In one RCT, topical Glyceryl trinitrate was found to be effective, with benefits persisting for more than three years (Paoloni et al. 2004).However, Kane et al. (2008) did not find any significant superiority in the outcomes of the patients who underwent the application of the patch compared with control in terms of pain and disability at six months. No histological difference in neovascularisation, collagen synthesis, or stimulated fibroblasts from the two groups who were operated on was found (Kane et al. 2008).
Conclusion
Chronic Achilles tendinopathy is a painful, chronic and debilitating condition affecting both the athletic population and sedentary individuals. The majority of patients with Achilles tendinopathy can be treated non-operatively. Progressive loading programs seem to be the most successful evidence-based treatment, with adjuncts such as ESWT in certain individuals.
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Running Expert Reveals His 5 Step Formula to Become a Running Rehab Specialist!

What customers have to say about this course
- gustaf hübinette05/02/25A fantastic course A fantastic and comprehensive course that I feel has both broadened and deepened my knowledge of running-related injuries and their rehabilitation. The content maintains a clear and cohesive structure, firmly grounded in research. A big plus is that even after completing the course, you can revisit the material whenever you need to review certain areas.Simon20/01/25Good, but too much! It's of course a luxury problem. It delivers, absolutely. I know a lot more about running injuries now. But you need to review how much time it takes to finish this monster.
- Salih Kuzal30/12/24Running Rehab Salih Kuzal Een hele leuke uitgebreide cursus wat goed toepasbaar is in de dagelijkse praktijk. Heb er veel van geleerd!Sander Wierstra27/12/24Leerzame cursus Deze cursus heeft me inzicht gegeven om topatleten en sporters beter te begeleiden richting een duurzame herstel, ik raad deze cursus zeker aan!
- Jaime van der Lugt27/12/24Running Rehab 2.0 Well organised and clear set-up course to dive deeper into Running Rehab. Very extensive. Would definitely recommend it!Jasper Campfens24/12/24Top cursus Erg sterke cursus. Zeer uitgebreid wordt er ingegaan op alle meest voorkomende hardloopblessures. Van diagnose tot RTR.
- Carmen21/12/24Running Rehab Very good en clear course!Thorin21/12/24Sterke aanrader! Zeer uitgebreide cursus over een grote populatie binnen de bevolking. Elke kinesitherapeut zal hier veel uit bijleren, of hij nu zelf aan lopen doet of niet! Gestructureerde cursus bestaande uit Evidence-Based teksten en video's. Duidelijke toepassing van de theorie terug te vinden in de video's.
- Ivo Rigter03/12/24Running Rehab: From Pain to Performance Bedankt voor de zeer uitgebreide en informatieve cursusEllen Oosting27/11/24Veel geleerd! Veel geleerd over blessures, behandeling, training en terugkeer naar sport. Afwisselende inhoud. Veel praktische tools. Punten ook snel bijgeschreven na afronding.
- Olivier19/11/24Goede cursus! Ik kan deze cursus alle fysiotherapeuten aanraden!Joas de Bijl07/11/24Fijne cursus Goede cursus waar wetenschap en klinische ervaring in terug komt. Leuke video’s die wat mij betreft goed aansluiten op de praktijk!
- Koen24/10/24Leerzame Cursus Een cursus die een absolute bijdrage levert voor therapeuten die veel patiënten zien met hardloopblessures.
Vooral de praktische tips en de opbouw na een blessure zijn erg bruikbaar en toepasbaar in een eerste lijn praktijk.
Tevens zijn de evidence based artikelen een mooie toevoeging op de kennis die al wordt gegeven.Tim14/10/24Great course Learned a lot about running injuries. So much more structure in assessing and treating all lower limb injuries. - Maria Kramer14/10/24Running Rehab: From Pain to Performance Goede cursus voor therapeuten die veel hardloopblessures behandelen en hier meer over willen weten. Veel evidence based informatie en praktische tips voor de opbouw na een blessure.Emin Yildiz26/08/24Running Rehab: From Pain to Performance Leerzaam, uitleg en inhoud van top kwaliteit!
- Daniel Deyhle02/02/24Running Rehab: From Pain to Performance A VERY DETAILED COURSE
Really nice! Lot´s of high quality content! I learned so much. Thank you!Jarne Standaert18/04/23Running Rehab: From Pain to Performance Dit is een uitstekende cursus voor therapeuten die patiënten met loopblessures gerichter en efficiënter willen behandelen. Je krijgt enerzijds een uitgebreid overzicht van welke loopgerelateerde blessures zich vaak voordoen. Anderzijds krijg je een goed onderzoekskader om de tekorten bij je patiënten op te sporen en dus ook gerichter te behandelen. De cursus is heel duidelijk. Je krijgt ook een goed beeld van welke oefentherapie je best toepast in een bepaald stadium van een bepaalde pathologie - Hannah Yelin09/04/23Running Rehab: From Pain to Performance A great course that gives you a comprehensive and detailed knowledge of various running complaints. The content is evidence based and the literature is attached. It is very well taught how to transfer the evidence into everyday practice. I highly recommend this course to all physios who work with runners.
Thank you for a great course!Ruba Al Barghouthi23/10/22Running Rehab: From Pain to Performance Very informative course. Highly recommended for every MSK Physiotherapist and any other health care providers who deal with runners.