AC Joint Pain / Acromioclavicular Injury | Diagnosis & Treatment

AC Joint Pain / Acromioclavicular Injury | Diagnosis & Treatment
Introduction & Epidemiology

The clavicle functions in support and mobility of the upper extremity. It serves as a transition point between the shoulder girdle and the trunk of the body, connecting the upper extremity to the axial skeleton. On top of that, it serves to protect the subclavian vessels and brachial plexus (Balcik et al. 2013).
A fibrocartilaginous intra-articular disk of variable size and shape is interposed between the bony articulation, which functions to correct bony incongruities between the concave acromial surface and the convex distal clavicle. Disk degeneration may begin as early as the second decade of life, often resulting in little more than a fibrocartilaginous remnant by early adulthood (Menge et al. 2014).
While injuries are a common precipitating cause of ACJ pain, arthritis is usually the main cause of pain and develops as a consequence of constant stress on the joint, often in people who perform repeated overhead lifting activities (Buss et al. 2003).
During your screening process, it is important to rule out a fracture of the clavicle or severe AC joint separation. Clavicular fractures account for 2,6-5% of all fractures and their mechanism of injury is similar to that of an AC injury (Melenevsky et al. 2011).
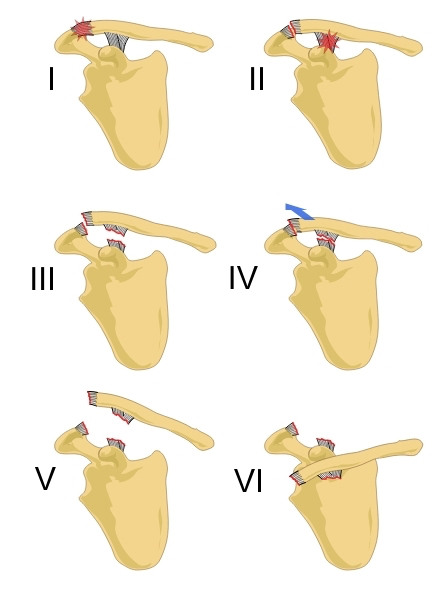
Acromioclavicular joint separations are graded according to severity based on the Rockwood classification:
I: AC ligament stretched
II: Partial rupture of AC ligaments
III: Complete rupture AC ligaments and coracoclavicular (CC) ligaments
IV: Clavicle displaced posteriorly over the acromion
V: Clavicle displaced just under the skin
VI: Clavicle underneath coracoid (very rare!)
There is consensus in the literature that grade I-III (according to the Rockwood classification) is managed conservatively and grades IV-VI are managed surgically (Reid et al. 2012).
The mechanism of injury is reported to be either a fall onto the point of the shoulder or the outstretched arm.
Epidemiology
Van der Windt et al. (1995) found a 1-year prevalence of 4% for acromioclavicular syndrome in a Dutch cohort of 349 patients with shoulder complaints (restriction of horizontal adduction, pain in the area of the AC joint, and/or C4 dermatome).
Östör et al. (2005) evaluated 131 patients with shoulder pain in an English cohort over a period of one year and found a prevalence of 24% for AC Joint pathology.
The differences between these findings might be explained due to different diagnostic criteria that were used, which were more strict in the study of Van der Windt et al. (1995).
So one might assume that the study of Östör et al. (2005) includes a high rate of false-positive results as they classified AC joint pathology based on painful horizontal adduction only.
For AC joint sprains Hibberd et al. (2016) found an incidence rate of 1,72 cases per 10.000 athlete-exposures. The majority of sprains were reported in football (50,4%), followed by ice hockey (34,6%), wrestling, and during competition (66,0%). The male: female ratio was 4.67 with most sprains being caused by player contact (54,7%) followed by surface contact (29,0%).
The Recurrency rate was as high as 9,7% with 1% of all sprains requiring surgery.
Be aware that diagnostic imaging of the AC joint can be misleading. Jordan et al. (2002) have found that the only statistically significant correlation was between the high signal in the distal clavicle and clinically found degenerative changes. Furthermore, they state that a weaker relationship existed between the fluid in the joint and clinical examination and between increasing degenerative changes and advancing age. Otherwise, no material relationship was found between any of the other MRI abnormalities and the clinical picture.
On top of that, Girish et al. (2011) examined 51 asymptomatic shoulders in men (average age 56y, range 40-70y) and found a prevalence of osteoarthritis of the AC joint in 65% of all cases.
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
Signs & Symptoms
AC arthritis generally presents with complaints of progressively worsening shoulder pain, although minor trauma or strenuous activity may cause an acute exacerbation of this chronic degenerative condition. The pain is typically located over the anterior aspect of the shoulder in the region of the AC joint or referred to the shoulder and upper arm.
Overhead activities, weight lifting, and cross-body movements using the affected arm often are associated with worsening symptoms.
Pain at night is more common when patients lie on the affected side and difficulty sleeping can be a reason why contact with a health professional is sought in the first place.
Additionally, popping, clicking, grinding, and a catching sensation with movement of the shoulder might be present. A careful history of trauma or injuries can raise suspicion for instability or other associated pathologies (Menge et al. 2014).
Cadogan et al. (2013) have developed a cluster including signs & symptoms and items from physical examination in order to diagnose non-traumatic AC joint.
Examination
The painful arc test can be used in the evaluation of the symptomatic AC joint as well. The only difference compared to the subacromial pain syndrome category is that patients commonly report symptoms at shoulder flexion and abduction end range between 170-180° of movement:
Krill et al. (2018) have performed a systematic review evaluating the most accurate combination of physical tests in order to evaluate the ACJ as the source of nociception. Watch the following video to learn which tests have been included:
Other common orthopedic tests for the AC Joint are:
- AC Shear Test
- Paxinos Sign
- AC Resisted Extension Test
- AC Joint Line Tenderness
- Cluster of Chronopoulos
LEARN TO DISTINGUISH SHOULDER FACTS FROM FICTION

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Treatment
The main goal of treatment for ACJ arthritis is to reduce pain, allowing a full range of motion and strength. The first line of treatment is nonoperative management, and options include rest, activity modification, non-steroidal anti-inflammatory medications, corticosteroid injections, and physical therapy. Patients who present after an acute exacerbation of their symptoms often will benefit from an initial period of rest, brief immobilization in a sling, and periodic application of ice or moist heat (Mazzocca et al. 2007).
Activity modification involves avoidance of repetitive, overhead, and cross-body movements and is paramount in preventing the re-aggravation of symptoms. Physical therapy is aimed at improving strength and range of motion of the shoulder girdle, specifically the periscapular and rotator cuff musculature (Mall et al. 2013).
Until now, no randomized controlled trials have been conducted to compare arthroscopic surgery, open surgery, steroid injections, and rehabilitation programs with each other. At the moment there is also no clear evidence that steroid injections are effective or ineffective in treating ACJ pain as few studies report long-term outcomes (Chaudhury et al. 2017). Surgery is usually considered in patients with severe ongoing symptoms despite having tried conservative therapy. While the trend is going towards arthroscopic surgery over open surgery, the long-term clinical outcome of pain relief and function are probably comparable (Flatow et al. 1992).
References
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
It’s Time to Stop Nonsense Treatments for Shoulder Pain and To Start Delivering Evidence-based Care

What customers have to say about this course
- Tineke De Vries26/01/25Goede cursus. Goede cursus, gericht op de praktijk Veel geleerd. Met name wat betreft de opbouw van de oefeningenDempsey Thiele02/01/25Overzichtelijk en praktisch! Ik heb de cursus met plezier afgemaakt. Ik denk dat dit een relevante cursus is voor iedere fysiotherapeut die meer inzicht wil krijgen over de huidige evidence omtrent schouder rehabilitatie. Alle informatie wordt overzichtelijk aangeboden.
Ik kan weer kritisch aan de slag mijn patiënten te helpen in de toekomst! - Carlijn Duursma27/12/24Goede cursus Veel verdieping. duidelijke uitleg. misschien wat tekeningen toevoegen voor extra verduidelijking. Veel geleerd.Vanessa Burnet22/12/24Leerzame cursus Opfrissing van kennis wat is weg gezakt.
- Paul Mensink15/12/24Paul Mensink High level literature composed course, videos are perfect examples for used techniques and exercisesFrank Kleyn12/12/24CRSP Ik kan bovengenoemde cursus zeer aanbevelen , nieuwste inzichten , zin en onzin van Subacromiale ruimte , de duidelijke vertaling naar de praktijk en de behandeltafel .
- Marty26/11/24RCRSP CURSUS Niet heel veel nieuws maar wel een goed overzicht en duidelijke uitleg over biomechanica.
Goede filmpjes van Filip en technieken ook goed uitgelegd.
Goede toetsen die de lesstof vrij compleet behandeld..
Website werkt naar mijn mening niet goed. Nogal onoverzichtelijk…
Vergt wat tijd om er mee om te gaan maar voordeel van de cursus is de gunstige prijs per accreditatie punt. Netjes.maria Kramer01/11/24goede cursus voor rcrsp Goede cursus met veel praktische vaardigheden en oefeningen die je direct kunt toepassen, aanrader. - Erik Versluis13/08/24Rotator Cuff Related Shoulder Pain RCRSP by Filip Struijf
State of the art course and very useful for physiotherapists with shoulder expertise or who want to further develop their skills in research and treatment of patients with shoulder complaints. A nice addition is a shoulder case in which you can process the knowledge you have recently acquired.
A major advantage is the possibility to read the course material offered and to watch the video material again.Birgit Schmitz28/04/24Rotator Cuff Related Shoulder Pain RCRSP
Ik vond het een waardevolle cursus met onderbouwd wetenscahppelijk onderzoek dat ondersteunt in mijn praktisch handelen. Ik heb al een nieuwe cursus uitgezocht. 🙂 - Thijs de Jager22/04/24Rotator Cuff Related Shoulder Pain GOEDE RCRSP CURSUS.
Over het algemeen een goede cursus waarbij ik veel ben opgestoken. Goede, evidence based informatie met hier een daar wat uitleg video’s die zeker helpvol waren. Het is ook fijn dat je onder de cursusonderdelen vragen kan stellen en hier een antwoord op kan verwachten van Filip zelf. 4 sterren i.p.v. 5 sterren omdat ik graag meer duidelijkheid en uitleg in video format over de oefeningen had willen zien. Er worden een hoop oefeningen getoond maar het is aan de cursist zelf om te bedenken welke in te zetten in de praktijk.Larson de Neve16/04/24Rotator Cuff Related Shoulder Pain GOOD COURSE
Good theoretical and practical course with exercises that you can immediately use in practice. - Beppeke Molenaar13/04/24Rotator Cuff Related Shoulder Pain OVERALL A GREAT COURSE
This is a very informative and comprehensive course.
Some of the quiz answers that are correct are counted as incorrect, which is a pity.
(Comment Physiotutors: We are currently doing an overhaul of our quizzing system and have fixed this issue now.)Willem Zee28/01/24Rotator Cuff Related Shoulder Pain PRIMA CURSUS!
goed te doen, uiterst praktisch - Jason Pearson11/01/24Rotator Cuff Related Shoulder Pain RCRSP COURSE
Very satisfied with this course. Provides a great framework with which to build your assessment and rehabilitation strategiesMichal Wajdeczko09/01/24Rotator Cuff Related Shoulder Pain Ik ben super blij ermee.
Het was een zeer interessante training. Het cursus was rijk met ge-update informatie, alles wordt volledig en transparant uitgelegd. Ik moet ook toevoegen dat deel van nuttige sets oefeningen briljant is! Veel nuttige tips en combinaties om rotator cuff pijn te kunnen verminderen en alle spieren efficiënt te trainen. Ik ben er trots op dat ik weer mijn kennis en competenties kon ontwikkelen en om mijn patiënten een professionele benadering van schoudercomplexe aandoeningen te kunnen bieden.
Super bedankt!! - Ante Houben30/12/23Rotator Cuff Related Shoulder Pain RCRSP
This course is well designed and based on solid evidence. The information is presented in a structured manner, using text, images and videos to enhance understanding. In addition, I appreciated the course’s emphasis on effectively conveying this information to patients. However, I wished the exercise therapy was more extensive.
Naomi Tiller20/12/23Rotator Cuff Related Shoulder Pain RCRSP COURSE
Fantastic course that’s easy to follow, up to date and evidence based. I’ve immediately been able to implement what I’ve learnt in to my own work which has given me a lot more confidence as well as made it more enjoyable! A good refreshed for me on how the rotator cuff works, a better understanding of how to treat these problems and better communicate with my patients as well as exercise inspiration (always appreciated!). Overall very happy to have done this course!
Super bedankt!! - Stijn de Loof17/12/23Rotator Cuff Related Shoulder Pain GOOD THEORY, LESS EXERCESIS
I liked the theoretical part of the course. A good refresher about the shoulder and rotator cuff with new insights
I was a bit disappointed in the part ‘exercises’. They were super basic and without explinations.Mehdi Benkirane24/11/23Rotator Cuff Related Shoulder Pain REVIEW
Très bon cours, je le recommande pour se remettre à jour sur les tendinopathies de l’épaule.




