Patellar Instability

Body Chart
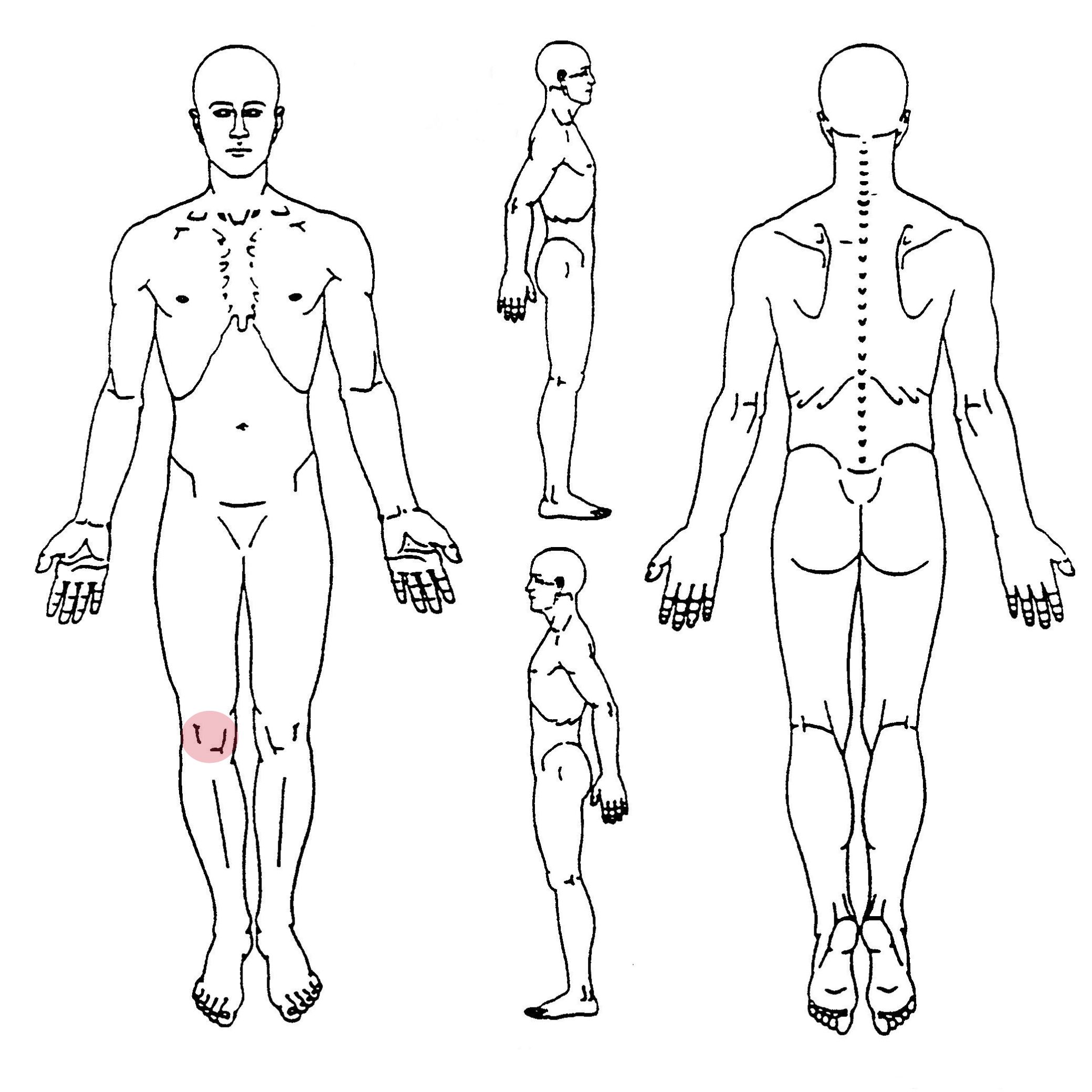
- Pain behind or around the patella
Background Information
Patient Profile
- Adolescent patients
- Peak age between 10 and 20 years
- Trauma in history or recurrent subluxations
Pathophysiology
Patellar dislocations occur most frequently during sports but in some cases can occur atraumatically. In a traumatic event, the knee is mostly flexed and subject to a valgus force or receives an anterior or medial blow to the knee. Atraumatic dislocations occur mostly in individuals who have diminished quadriceps strength and neuromuscular control and may present with anatomical abnormalities such as trochlear dysplasia, shallow and short trochlear groove, pes planus, a large tibial tuberosity-trochlear groove distance, increased ligamentous laxity, amplified patellar tilt, valgus limb alignment and rotational abnormalities of the tibia and femur.
Course
Patients who sustained a patellar dislocation are at increased risk of sustaining a second dislocation. The 5-year recurrence-free estimate for a sports-related dislocation is 53% versus 76% for atraumatic dislocations.
History & Physical Examination
History
Usually traumatic history – The knee is mostly flexed and subject to a valgus force or receives an anterior or medial blow to the knee. The patient will most likely tell you about the knee giving way and a “popping” sensation or sound that may be followed by swelling and possibly hemarthrosis. The patella may reduce spontaneously. Atraumatic dislocations mostly occur in young individuals who have reduced quadriceps strength and control. Movements requiring minimal force usually lie at the base of their instability symptoms and subluxations or dislocations occur often without trauma.
- Local
- Intense
- Swelling
- Feeling of instability/giving way
Physical Examination
Inspection
In case the patella is still dislocated, it will be most likely displaced laterally. Misalignment: trochlear dysplasia, an increased Q-angle, patella alta, increased tibial tuberosity-trochlear groove distance, knee valgus and torsional abnormalities
Functional Assessment
Squatting; range of motion and lower extremity strength
Active Examination
J-Sign can be indicative of patellar maltracking. Inability to move and load the knee with signs of apprehension
Passive Examination
Pain and swelling often impede a passive assessment. Tenderness at the medial epicondyle of the femur and medial patella, and apprehension during lateral displacement of the patella. The lateral femoral epicondyle may be tender from collision with the patella during dislocation and/or reduction. Tenderness over the origin of the medial patellofemoral ligament may be indicative of a ligamentous disruption. An increased lateral glide of the patella (2 or 3 quadrants of the patellar width) accompanied by apprehension can give an idea about ligamentous laxity or rupture. A positive patellar grind test may be suggestive of a chondral injury. Lateral tilting of the patella may suggest a tight lateral retinaculum.
Differential Diagnosis
- Fracture of the patella, femur or tibia
- Rupture of the cruciate or collateral ligaments
- Osteochondral loose bodies or lesions of the patella or trochlea
- Meniscal tear
- Patellofemoral syndrome
- Medial synovial plica
Treatment
Strategy
Patient education, progression of weight bearing, analgesics, active exercises for hip and knee muscles
Interventions
Passive: Brace/Tape, NSAIDs help in the acute stage, Patient education
Active: Address biomechanics of the lower limb, strengthening of quadriceps, hip abductor strengthening, hamstrings and gastrocnemius, proprioception
References
- Seitlinger G, Ladenhauf HN, Wierer G. What is the chance that a patella dislocation will happen a second time: update on the natural history of a first time patella dislocation in the adolescent. Curr Opin Pediatr. 2018 Feb;30(1):65-70. doi: 10.1097/MOP.0000000000000568. PMID: 29176355. https://pubmed.ncbi.nlm.nih.gov/29176355/
- Petri M, Ettinger M, Stuebig T, Brand S, Krettek C, Jagodzinski M, Omar M. Current Concepts for Patellar Dislocation. Arch Trauma Res. 2015 Sep 1;4(3):e29301. doi: 10.5812/atr.29301. PMID: 26566512; PMCID: PMC4636822. https://pubmed.ncbi.nlm.nih.gov/26566512/
- Hiemstra LA, Kerslake S, Lafave M, Heard SM, Buchko GM. Introduction of a classification system for patients with patellofemoral instability (WARPS and STAID). Knee Surg Sports Traumatol Arthrosc. 2014 Nov;22(11):2776-82. doi: 10.1007/s00167-013-2477-0. Epub 2013 Mar 28. PMID: 23536205. https://pubmed.ncbi.nlm.nih.gov/23536205/
- Johnson DS, Turner PG. Management of the first-time lateral patellar dislocation. Knee. 2019 Dec;26(6):1161-1165. doi: 10.1016/j.knee.2019.10.015. Epub 2019 Nov 11. PMID: 31727430. https://pubmed.ncbi.nlm.nih.gov/31727430/
- Baryeh K, Getachew F. Patella dislocation: an overview. Br J Hosp Med (Lond). 2021 Aug 2;82(8):1-10. doi: 10.12968/hmed.2020.0429. Epub 2021 Aug 4. PMID: 34431342. https://pubmed.ncbi.nlm.nih.gov/34431342/
- Ménétrey J, Putman S, Gard S. Return to sport after patellar dislocation or following surgery for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2014 Oct;22(10):2320-6. doi: 10.1007/s00167-014-3172-5. Epub 2014 Jul 22. PMID: 25047793; PMCID: PMC4169614. https://pubmed.ncbi.nlm.nih.gov/25047793/
- Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A. An Algorithmic Approach to the Management of Recurrent Lateral Patellar Dislocation. J Bone Joint Surg Am. 2016 Mar 2;98(5):417-27. doi: 10.2106/JBJS.O.00354. Erratum in: J Bone Joint Surg Am. 2016 Jun 15;98(12):e54. PMID: 26935465. https://pubmed.ncbi.nlm.nih.gov/26935465/
- Martin RK, Leland DP, Krych AJ, Dahm DL. Treatment of First-time Patellar Dislocations and Evaluation of Risk Factors for Recurrent Patellar Instability. Sports Med Arthrosc Rev. 2019 Dec;27(4):130-135. doi: 10.1097/JSA.0000000000000239. PMID: 31688530. https://pubmed.ncbi.nlm.nih.gov/31688530/
- Ling DI, Brady JM, Arendt E, Tompkins M, Agel J, Askenberger M, Balcarek P, Parikh S, Shubin Stein BE. Development of a Multivariable Model Based on Individual Risk Factors for Recurrent Lateral Patellar Dislocation. J Bone Joint Surg Am. 2021 Apr 7;103(7):586-592. doi: 10.2106/JBJS.20.00020. PMID: 33787553. https://pubmed.ncbi.nlm.nih.gov/33787553/


