Helping you become the best physiotherapist you can be

Premium online courses & webinars from clinical experts
Research Reviews, Blogs, Exams, Clinical Patterns, & More...
New Podcast Episode Every Month
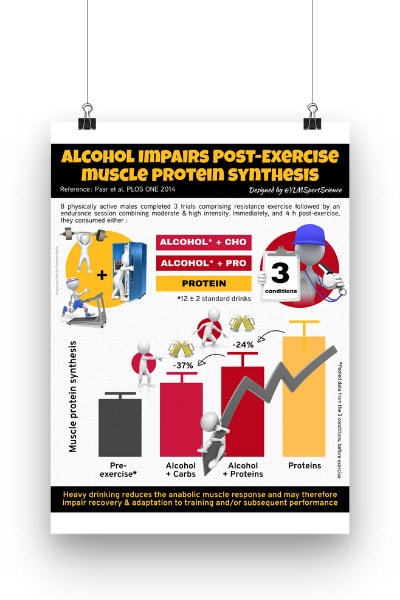
100% FREE POSTER PACKAGE
Receive 6 High-Resolution Posters summarising important topics in sports recovery to display in your clinic/gym.