Diagnosing Gluteus Medius Tendon Tears in Clinical Practice Using the Broken Wing Sign

Introduction
Gluteus medius pathology spans a spectrum from tendinopathy and partial tears to full-thickness and massive ruptures with fatty muscle degeneration and is common in older women and in post-hip arthroplasty or post-trauma patients. Symptoms are reported in the lateral hip and may lead to gait disturbances and functional loss. Early recognition is crucial to prevent irreversible atrophy. Therefore, this study examines the Broken Wing Sign, a simple prone clinical test to detect gluteus medius insufficiency when conventional standing tests or MRI are unavailable. This study was necessary since accurate diagnosis of gluteus medius tears remains challenging. Missed or delayed identification of gluteus medius pathology can lead to chronic pain, weakness, and irreversible muscle degeneration. Existing clinical tests, such as the Trendelenburg sign, often lack sensitivity or cannot be performed in patients with pain, balance issues, or postoperative restrictions, while MRI – the current gold standard – is costly and not always accessible. By introducing and validating the Broken Wing Sign, this study provides a simple, reliable, and non-weight-bearing test to detect hip abductor insufficiency early, and its accuracy is examined here.
Methods
A prospective study was conducted between 2022–2025, and included patients referred to specialized care for suspected abductor insufficiency. The patients underwent a clinical assessment by the lead author and surgeon. The assessment consisted of detailed history taking (identifying pain characteristics, prior hip trauma or surgery, and signs of abductor weakness) and standard physical examination tests of hip abductor function. Conventional assessments, such as the Trendelenburg sign and resisted hip abduction, were performed where possible. The authors noted that many patients could not tolerate these assessments due to pain, instability, or postoperative limitations. The Broken Wing Sign was then applied as a non-weight-bearing alternative.
The Broken Wing Sign is described as follows:
- The patient lies prone, with the knee of the tested leg flexed to 90°.
- Then the patient is asked to actively extend the hip against gravity
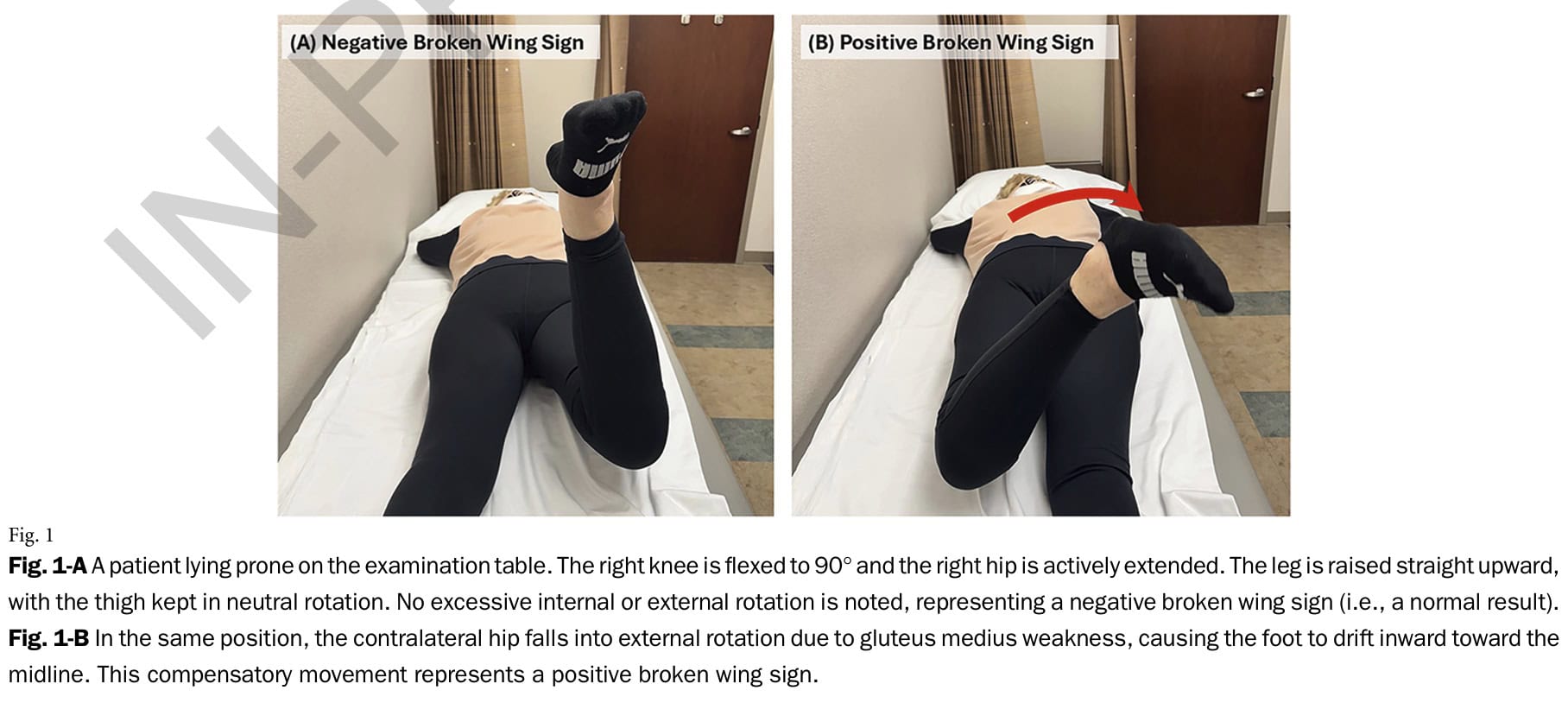
A negative Broken Wing sign indicates that the patient can lift the thigh without the hip drifting outward (external rotation). This indicates that the gluteus medius (especially its anterior fibers) is functioning well enough to stabilize the hip and maintain proper alignment during extension. It suggests that abductor strength and control are likely preserved, and significant tendon tear or advanced degeneration is unlikely.
A positive Broken Wing Sign occurs when the leg drifts into external rotation. This indicates that the gluteus medius – particularly its anterior, internally rotating fibers – has difficulty maintaining the hip’s neutral alignment, leading to compensatory external rotation. A positive test thus suggests weakness or tearing of the gluteus medius tendon, potentially accompanied by fatty degeneration or atrophy, and warrants further assessment or imaging to determine the extent of abductor insufficiency.
All findings were subsequently correlated with MRI results, which served as the reference standard for confirming tear presence, severity, and fatty infiltration. Tears were classified as none, partial, full-thickness, or massive (≥3 cm retraction). Fatty infiltration was graded via the Goutallier scale (0-4). Further, analyses of sensitivity, specificity, PPV, NPV, diagnostic odds ratio (DOR), and ROC curves were computed. The amount of external rotation of the hip in case of a positive Broken Wing Sign was analyzed as a continuous variable to determine optimal cutoffs.
Results
A total of 59 patients (75 hips) referred for suspected abductor insufficiency were included.The indications for referral included preoperative THA evaluation (7 hips), prior hip trauma (9 hips), post-THA pain (28 hips), or chronic lateral hip pain consistent with greater trochanteric pain syndrome (GTPS) (24 hips), and 7 asymptomatic contralateral hips were also included in the analysis.
A positive Broken Wing sign was observed in 49 hips (65% of the included 75 hips). The MRI scans identified 55 tears:
- 14 partial
- 13 full-thickness
- 28 massive
- 20 no tear
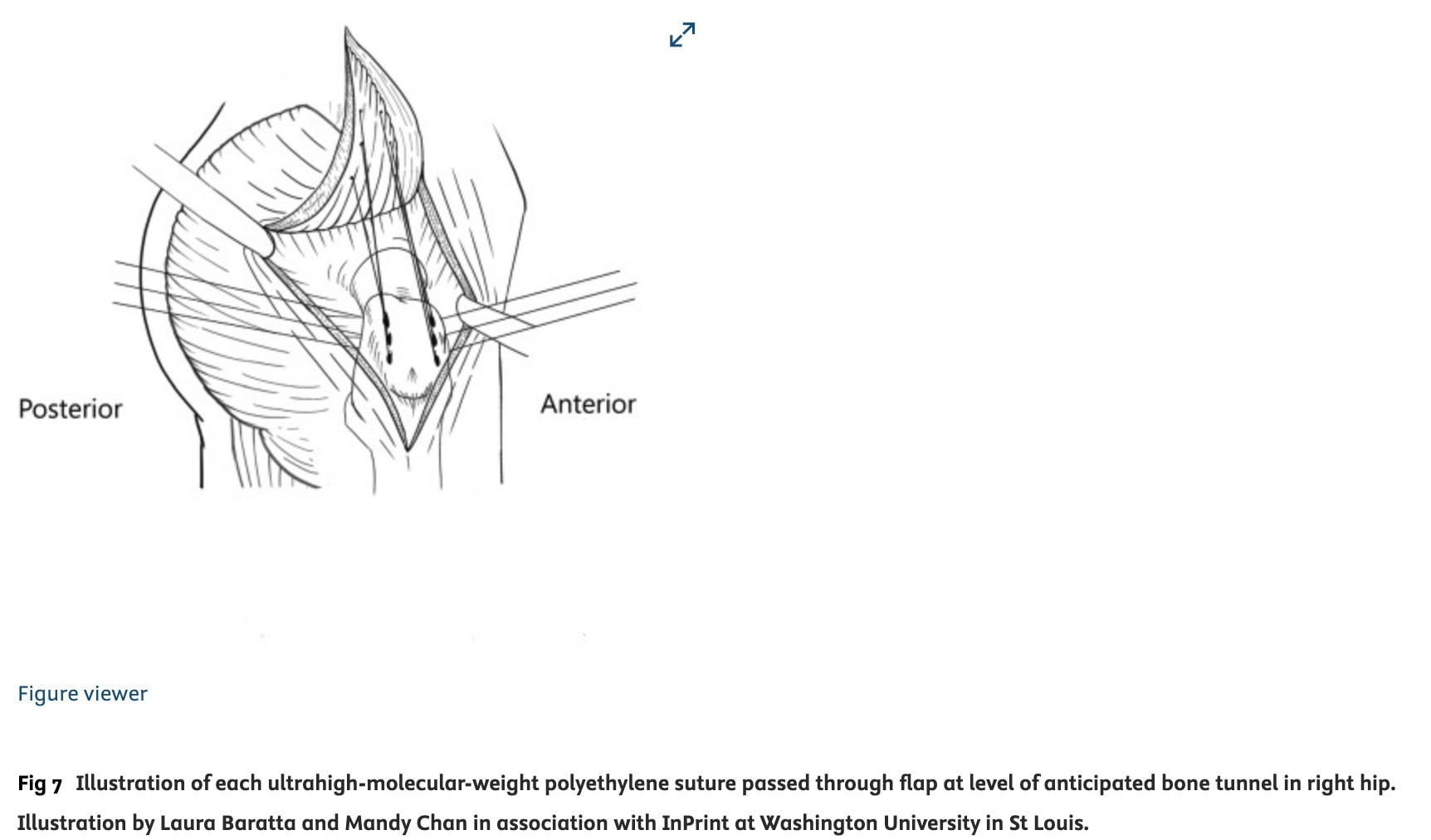
Surgery was performed in 35 patients; 11 out of 13 full-thickness tears were repaired using Achilles tendon augmentation, and 24 out of 28 massive tears were repaired using Gluteus Maximus transfer. All intra-operative findings matched the MRI conclusions.
Patients who had a positive broken wing sign during the examination presented with significantly more fatty infiltration than those with a negative broken wing sign (24.1% +/- 11.2% vs 14.6% +/- 7.1%). The amount of fatty infiltration of the gluteus medius was significantly higher in those patients having massive tears.
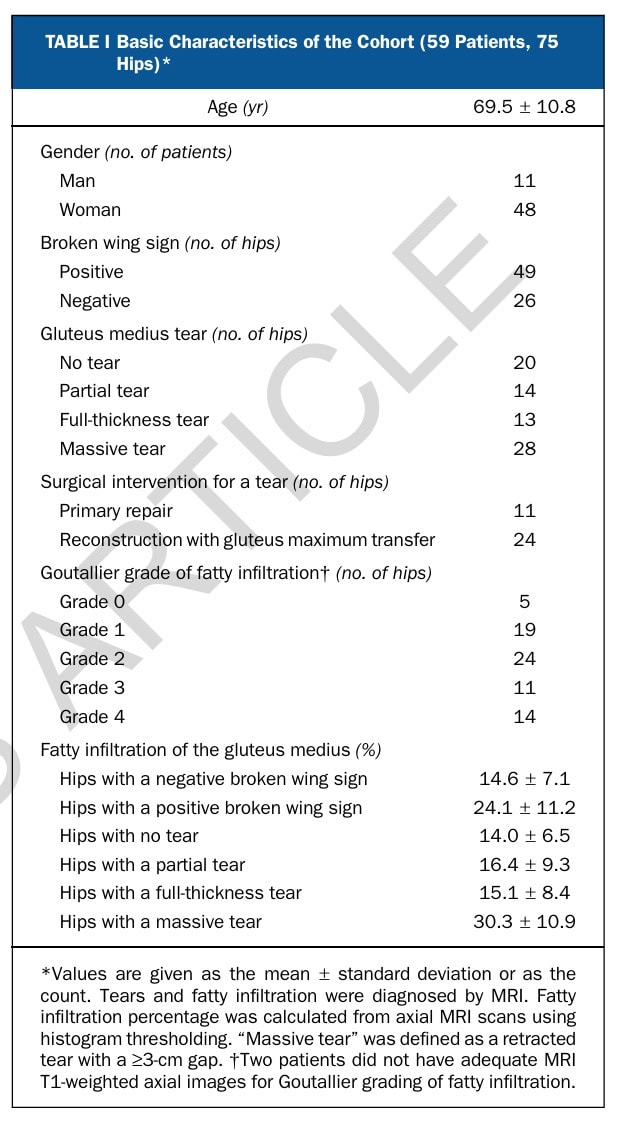
The diagnostic performance of the Broken Wing sign for diagnosing gluteus medius tendon tears was examined. The Broken Wing Sign showed strong diagnostic performance for identifying gluteus medius tears, with a sensitivity of 81.8%, specificity of 80.0%, and a positive predictive value of 91.8%. Its diagnostic odds ratio (17.8) indicated reliable discrimination between healthy and torn tendons. It also proved particularly useful in ruling out massive tears, with a negative predictive value of 96.1%. Furthermore, a markedly positive result—when the hip externally rotated by 30° or more—was always linked to a tear, achieving 100% specificity and PPV for significant gluteus medius damage.
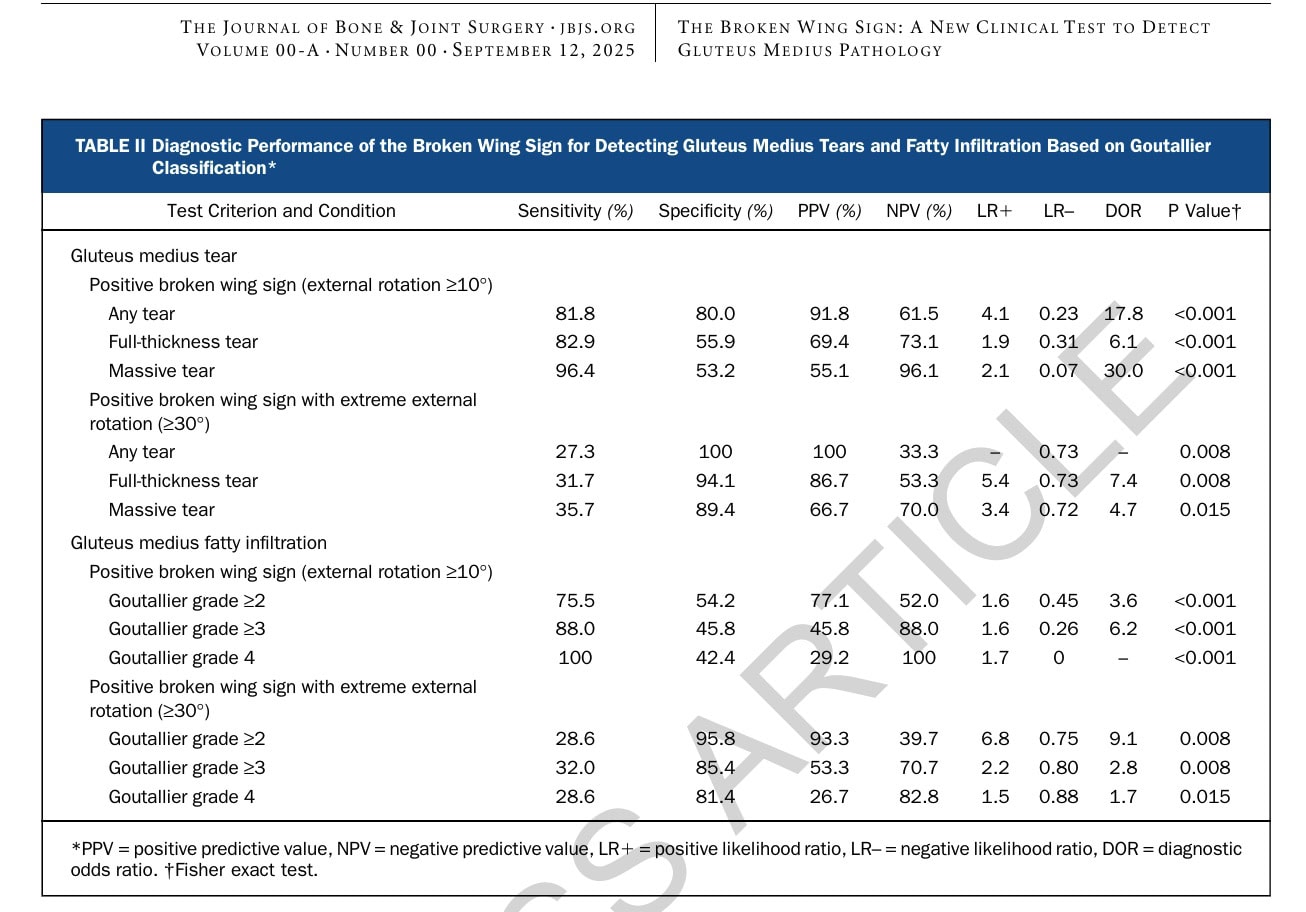
When the researchers then examined how the angle of external rotation related to severity, they found that the greater the rotation angle, the more severe the pathology. Hips with tears showed an average external rotation of 20°, compared with 1° in hips without tears. Hips with massive tears had also significantly greater external rotation during the Broken Wing assessment compared to hips with non-massive tears (27° vs 8°). A rotation of 30° or more was always associated with a tear – achieving 100% specificity and PPV – while smaller angles around 10° captured a broader range of tear severities with greater sensitivity.
The ROC curve analysis confirmed excellent diagnostic performance (AUC 0.873 for any tear and 0.846 for massive tears). The optimal cutoff determined statistically was around 12.5°, leading the authors to recommend ≥10° as a sensitive threshold (for any tear) and ≥30° as a highly specific indicator of major abductor pathology (massive tears).
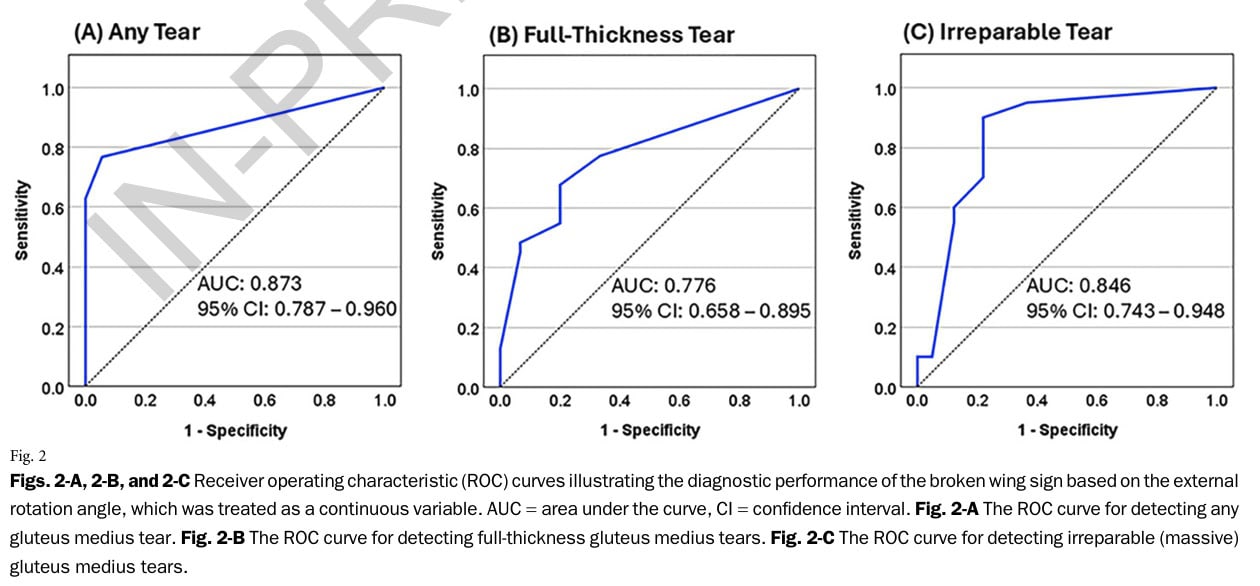
The authors also examined the association between the Broken Wing sign and the presence of fatty infiltration of the gluteus medius tendon. The external rotation angle correlated with the percentage of fatty infiltration (r = 0.498, p < 0.001), meaning that higher rotation angles generally reflected more muscle atrophy, though not in a perfectly linear way. A positive Broken Wing Sign was far more common in hips with advanced fatty infiltration, showing 88% sensitivity for Goutallier grade ≥3 and 100% sensitivity for grade 4.
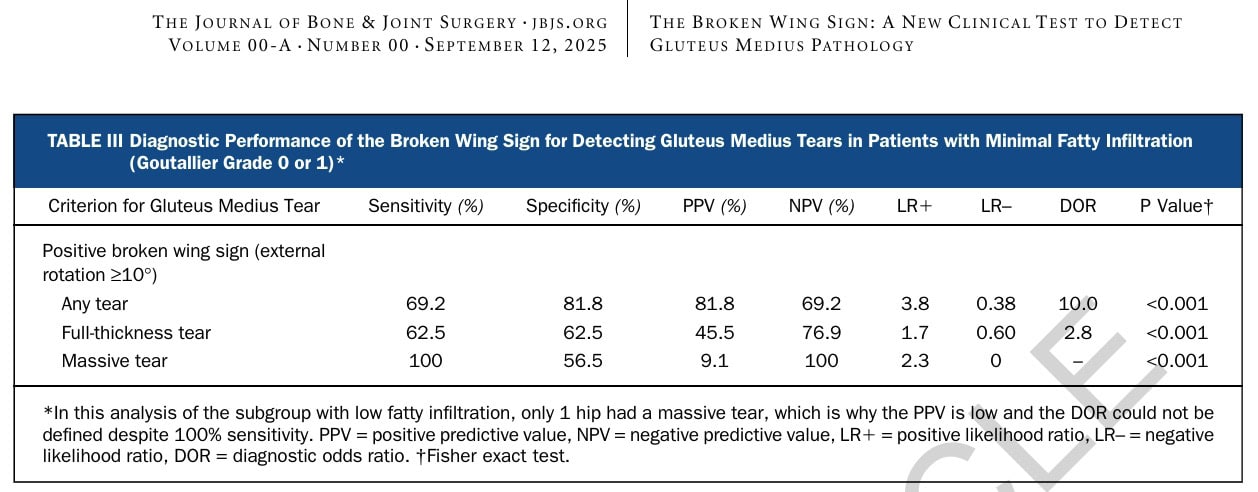
Even among patients with minimal fatty infiltration (Goutallier 0–1), representing more acute tears, the Broken Wing Sign performed reasonably well. It detected any tear with 69.2% sensitivity and 81.8% specificity, yielding a DOR of 10.0. For full-thickness tears, performance was lower (PPV 45.5%, DOR 2.8), suggesting that early or smaller lesions may not yet produce sufficient weakness to cause noticeable external rotation. The single massive tear in this subgroup also tested positive, though this isolated finding should be interpreted with caution. Overall, the test remained a helpful early detection tool, though it performed best in chronic, degenerative cases.
Questions and thoughts
To understand the Broken Wing Sign fully, we must take a look at the anatomical background of the assessment. The gluteus medius originates from the outer surface of the ilium and inserts onto the lateral surface of the greater trochanter. Its fibers can be functionally divided into anterior fibers, which internally rotate and flex the hip; middle fibers, which abduct the hip; and posterior fibers, which extend and externally rotate the hip. As such, the gluteus medius is a key hip abductor and stabilizer that also contributes to internal rotation of the femur through its anterior fibers. The Broken Wing sign specifically targets these anterior fibers of the gluteus medius.
When the patient lies prone with the knee flexed to 90° and actively extends the hip against gravity, the gluteus maximus provides the extension force and an external rotation torque, while the gluteus medius (particularly the anterior fibers) counteracts the external rotation.
- The femur stays neutral, the lower leg remains vertical, and the movement is smooth and controlled, representing a negative Broken Wing Sign.
When the gluteus medius is weak or torn, it can no longer resist the external rotation torque generated by the gluteus maximus during hip extension. Without this internal rotation control, the gluteus maximus overpowers the movement, pulling the femur into external rotation.
- This results in a visible outward rotation of the thigh and inward movement of the foot; the hallmark of a positive Broken Wing Sign.
Given that the Trendelenburg sign already exists and assesses Gluteus Medius function, one might question the necessity of developing this new test. The authors mentioned that in many cases, the Trendelenburg test could not be performed, as the patients had difficulties with balance and experienced too much pain in this standing assessment. Furthermore, the Trendelenburg has a good specificity, but the reported sensitivity is lower, which may lead to false-negative results. There, this test comes in handy as it does not require balance and can be tested in patients severely affected by pain.
In a subset of the sample (35 hips), both the Trendelenburg test and the Broken Wing sign were conducted. When both the Trendelenburg test and the Broken Wing Sign could be performed, the diagnostic accuracy was almost identical. Each showed 92.9% sensitivity, 100% specificity, and 100% PPV, and 77.8% NPV for detecting any tear. When either test was positive, sensitivity increased to 100% without any loss of specificity. However, more than half of the cohort couldn’t perform the Trendelenburg test because of pain, balance problems, or assistive device use. This demonstrated the practical advantage of the Broken Wing Sign, which can be reliably performed in the prone position even when standing tests are not feasible.
The article mentioned that several patients were operatively treated, either using a gluteus maximus transfer or an Achilles tendon augmentation. In case you wonder what the gluteus maximus transfer technique encompasses, the video from Arthroscopy Techniques and the picture below explain it nicely.
Talk nerdy to me
The lead author was also the assessor and the interpreter of the study results, this can give bias. Interobserver agreement for the MRI grading was substantial (κ = 0.757), reinforcing that the test reflects genuine degenerative changes rather than observer bias.
A limitation is that in the text, the authors mentioned that the external rotation angle was strongly correlated with the amount of fatty infiltration. However, inspection of the correlation coefficient r=0.498, p < 0.001 tells us that it is only a moderate positive relationship: as the external rotation angle increases, fatty infiltration tends to increase as well, but it’s not a perfect or tightly coupled relationship.
Despite its strong diagnostic accuracy, the Broken Wing Sign isn’t without limitations. False positives may occur in patients with hip arthritis, lumbar radiculopathy, or gluteus maximus weakness, as these conditions can also limit internal rotation and create compensatory patterns. The test also requires patients to tolerate a prone position with the knee flexed, which can be uncomfortable for those with lumbar or knee problems. Severe gluteus maximus weakness might even mask a positive response.
The Broken Wing Sign showed high diagnostic accuracy for gluteus medius tears, with 81.8% sensitivity, 80.0% specificity, a PPV of 91.8%, an NPV of 61.5%, a diagnostic odds ratio of 17.8, and an AUC of 0.873. In a subset of patients who underwent surgery, intraoperative observations were consistent with both MRI classifications and Broken Wing Sign results, supporting the accuracy of the test. However, we must add a caveat here. Since this population was preselected, the diagnostic accuracy was inflated by the high pretest probability. This is the chance that a patient already has the condition before you perform the test. This probability is determined by the prevalence of the condition in your population. The article states: “This prospective study, approved by our institutional review board, included 59 consecutive patients (75 hips) who were referred to a specialized hip clinic from December 2022 to February 2025 for suspected hip abductor insufficiency.”
- In a high pretest probability group (like this study’s cohort, where most patients were already suspected of abductor tears), a positive test is far more likely to be a true positive—the PPV increases.
- However, the NPV decreases, meaning a negative test becomes less reliable at ruling out disease.
- Conversely, in a low pretest probability setting (e.g., a general musculoskeletal clinic where few patients actually have tears), the PPV falls—you’ll see more false positives—but the NPV rises, so a negative test becomes more reassuring.
Take-home messages
The Broken Wing Sign offers a simple, practical way for diagnosing gluteus medius tendon tears or weakness, especially in patients who can’t tolerate standing tests like the Trendelenburg sign. When the hip externally rotates during prone extension, it signals that the gluteus maximus is overpowering a weak or torn gluteus medius, a clear marker of abductor insufficiency.
This test not only detects the presence of tears but also correlates with the degree of muscle degeneration: larger external rotation angles are typically seen with greater fatty infiltration and chronic damage. For clinicians, it serves as a fast, low-cost screening tool to decide when MRI or surgical referral may be warranted.
However, the test isn’t flawless. Other causes of hip weakness (such as arthritis, lumbar radiculopathy, or gluteus maximus dysfunction) can mimic a positive result. It also requires the patient to tolerate prone positioning with the knee flexed, which can limit its use in those with spinal or knee pain. These factors pose potential threats to the specificity and generalizability of the findings. It is worth remembering that the test was studied in a sample with high prevalence and that the diagnostic accuracy is dependent on the setting you are working in.
Reference
