Conservative Meniscus Tear Management: 2024 ESSKA-AOSSM-AASPT Consensus on Prevention, Rehabilitation & Return to Sport

Introduction
This is the second installment in our two-part series on meniscus rehabilitation. While Part 1 addressed post-surgical care, this article focuses on conservative meniscus tear management—a critical first-line approach for patients with meniscal injuries. Surgery carries inherent risks, consumes significant healthcare resources, and isn’t always necessary, especially given evidence that structural damage doesn’t consistently correlate with pain.
Conservative care offers a patient-centered framework, prioritizing function, psychosocial factors, and active participation. This approach aligns with growing evidence supporting non-operative strategies as a valuable option for meniscus tear management.
This review examines evidence-based prevention, non-operative treatment for acute/degenerative tears, and return-to-sport criteria—applying the 2024 ESSKA- AOSSM-AASPT consensus to optimize conservative meniscus tear management in practice.
Methods
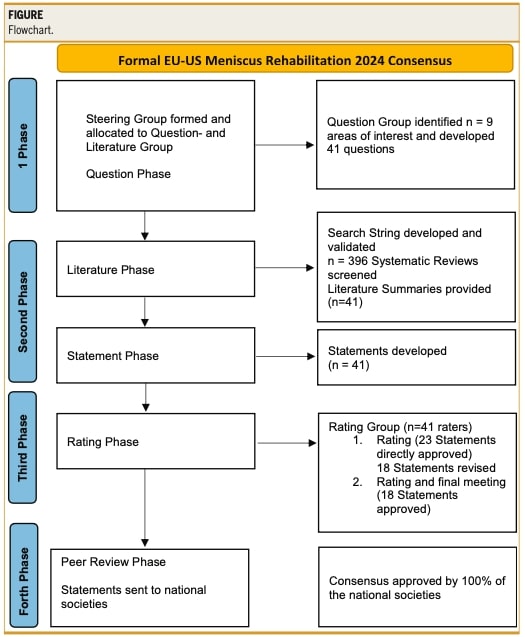
This study employed the same methodology as Part 1 of the consensus on post-surgery meniscus rehabilitation. Building on our previous discussion of the research approach, we briefly outline the key steps below.
A 26-member steering group (50% physiotherapists, 50% surgeons from Europe and the US) identified key questions, conducted literature reviews, and drafted consensus statements. An independent international rating group then evaluated these statements through two rounds of scoring using a 9-point Likert scale (0=unacceptable, 9=strong agreement). Disagreements were resolved through structured discussions between both groups.
Statements were graded by scientific strength (A=high evidence; B=presumption; C=low evidence; D=expert opinion) and consensus level:
- Relative agreement: median score >7 (all raters ≥5)
- Strong agreement: median >7 (no scores <7)
This transparent process ensures clinically relevant recommendations for conservative meniscus tear management while maintaining scientific rigor.
Results
Prevention of Meniscus Injuries
Can We Prevent Traumatic Meniscus Tears?
Neuromuscular training programs like FIFA11+, PEP (Prevent Injury and Enhance Performance), and Knäkontroll may help prevent traumatic meniscus injuries, despite being originally designed for ACL and general lower extremity injury prevention. (GRADE C) Relative Agreement: Mean 7.95 ± 1.63, median 8.5 (range 5-9).
Risk Factors
High-risk activities for meniscal injuries include:
- Sports involving cutting, pivoting, and landing maneuvers
- Occupational tasks (>10 lbs/4.5kg lifting, kneeling, deep squatting)
- High volume of climbing
(GRADE A) Relative Agreement: Mean 8.38 ± 0.85, median 8.5 (range 5-9).
Rehabilitation Management of NON- OPERATED Acute Meniscus Tears
Rehabilitation vs Surgical Treatment for Meniscal Tears
The consensus found no definitive allocation criteria for choosing between conservative meniscus tear management and surgical intervention due to insufficient scientific evidence. (GRADE D) Relative Agreement: Mean 7.85 ± 1.62, median 8 (range 5-9).
Surgical Considerations
Larger tears (bucket handle, RAMP lesions) and younger patient populations may benefit more from surgical intervention. (GRADE D) Relative Agreement: Mean 7.85 ± 1.62, median 8 (range 5-9).
Patient-Reported Outcomes
Two studies showed equivalent self-reported outcomes between surgical and conservative management for both traumatic and non-traumatic meniscal tears. (GRADE A) Relative Agreement: Mean 7.85 ± 1.62, median 8 (range 5-9).
Factors influencing rehabilitation effectiveness
The authors identified a lack of scientific evidence to accurately determine factors influencing rehabilitation outcomes. (GRADE D) Relative Agreement: Mean 8.04 ± 1.08, median 8 (range 6-9).
However, several potential factors may play a role, including lower extremity alignment, BMI, medical comorbidities, psychosocial and socioeconomic factors, tobacco consumption, treatment compliance, and activity level. Additionally, the presence of osteoarthritis and meniscal tear characteristics (type, location, and magnitude) might impact rehabilitation outcomes. (GRADE D) Relative Agreement: Mean 8.04 ± 1.08, median 8 (range 6-9).
Optimal Interventions for Conservative Meniscus Tear Management
While no interventions exist specifically for isolated meniscal rehabilitation, lower extremity injury management principles can be applied. Key priorities include resolving knee effusion, reducing pain, restoring quadriceps strength, and regaining joint-specific motor control. (GRADE D) Relative Agreement: Mean 7.16 ± 1.90, median 8 (range 5-9).
Adjunctive Modalities
The authors propose considering NMES, TENS, cryotherapy, and blood flow restriction exercises, though evidence remains limited. (GRADE D) Relative Agreement: Mean 7.16 ± 1.90, median 8 (range 5-9).
Rehabilitation Setting
When comparing home-based versus supervised rehabilitation with tailored home exercises, the consensus favors supervised programs despite no available evidence. (GRADE D) Relative Agreement: Mean 8.26 ± 1.20, median 9 (range 5-9).
Rehabilitation Planning
Clinicians should adopt a criterion-based milestones approach (consistent with post- surgical protocols) when designing rehabilitation plans. (GRADE B) Relative Agreement: Mean 7.55 ± 1.86, median 8 (range 5-9).
Rehabilitation of non-operated degenerative meniscal lesions
Non-Operative Treatment vs. Arthroscopic Partial Meniscectomy for Degenerative Lesions Strong evidence indicates comparable outcomes between conservative management and surgery for degenerative meniscal lesions, supporting non-operative treatment as first-line therapy. (GRADE A) Relative Agreement: Mean 7.87 ± 1.61, median 8 (range 5- 9).
Surgical Consideration
If symptoms persist after 3-6 months of conservative treatment, surgical intervention may be considered despite limited prognostic indicators. (GRADE D) Relative Agreement: Mean 7.87 ± 1.61, median 8 (range 5-9).
Factors Influencing Rehabilitation Effectiveness for Degenerative Meniscal Tears
As with traumatic lesions, no clearly identifiable factors impede recovery in degenerative meniscal tears. However, higher BMI, osteoarthritis, and longer symptom duration may negatively influence outcomes. (GRADE D) Strong Agreement: Mean 8.23 ± 0.59, median 8 (range 7-9).
Recommended Rehabilitation Approaches
Evidence-supported interventions include:
- Manual therapy and joint mobilization techniques
- ROM and neuromuscular control exercises
- Progressive knee/hip strengthening
- Neuromuscular electrical stimulation (NMES)
(GRADE B) Relative Agreement: Mean 7.62 ± 1.12, median 8 (range 5-9)
Adjunctive Therapies
- Blood flow restriction training for early-stage strengthening
- Combined supervised and home-based exercise programs
- Knee bracing for stability perception and symptom management
(GRADE D) Relative Agreement: Mean 7.62 ± 1.12, median 8 (range 5-9)
Return to sport After meniscus injury and surgery.
Return to Sport Criteria and Timeframes After Meniscal Injury
Return to sport (RTS) following meniscal injury should follow both time-based and criterion-based progression. For detailed healing timelines, consult the EU-US Meniscus Rehabilitation Consensus document.
Key RTS Criteria
Joint function:
- Full ROM restoration
- Absence of effusion
Strength metrics:
- Quadriceps/hamstring strength and activation
Performance testing:
- Coordination and stabilization tasks
- Hop tests (limb symmetry ≥90%)
Psychological readiness:
- Patient confidence and motivation
(GRADE C). Relative Agreement: Mean 7.68 ± 1.39, median 8 (5–9).
On-Field Rehabilitation for Athletes
Athletes require tailored on-field rehabilitation programs that incorporate comprehensive task analysis and progressive return-to-sport protocols. (GRADE D) Relative Agreement: Mean 8.08 ± 1.25, median 9 (range 5-9).
Factors Influencing Return-to-Sport Timelines
The time required to return to sport is influenced by multiple factors including the lesion type, location, and size, as well as the surgical technique when applicable. Additionally, concomitant injuries and specific surgical procedures may further impact RTS timelines. (GRADE D) Relative Agreement: Mean 8.13 ± 1.21, median 9 (range 5-9).
Activity Outcomes and Contraindications for Return to Sport
Activity outcomes following meniscus injury or surgery are largely dependent on injury characteristics, including tear type, size, and location. Return to sport (RTS) should only be considered when all established clinical milestones are met; conversely, RTS is not recommended when these rehabilitation benchmarks remain unachieved. (GRADE D) Relative Agreement: Mean 7.84 ± 1.60, median 8 (range 5-9).
Patients reported outcomes measures and assessment.
What patient self-reported outcomes should be used after meniscal tear or surgery?
Following meniscal injury or surgery, clinicians should implement validated assessment tools including: the Western Ontario and McMaster Universities Arthritis Index (WOMAC), Knee Injury and Osteoarthritis Outcome Score (KOOS), and International Knee Documentation Committee (IKDC) for knee-specific function; the Tegner Activity Scale and Marx Activity Rating Scale for activity levels; and the Visual Analog Scale (VAS) for pain measurement. (GRADE B) Agreement: Mean 8.39 ± 1.02, median 9 (range 5-9).
Clinical Assessment Measures for Meniscal Rehabilitation Monitoring
For objective evaluation during post-injury or post-surgical rehabilitation, clinicians should incorporate multiple assessment domains. Range of motion (ROM) measurements and effusion quantification provide fundamental joint status indicators, while handheld dynamometry offers practical strength assessment of knee flexion/extension. Functional progression should be evaluated through standardized hop tests, with advanced-stage rehabilitation incorporating distance measurements interpreted via limb symmetry index calculations. (GRADE D) Relative Agreement: Mean 7.78 ± 1.20, median 8 (range 5-9).
Indications for Referral Following Meniscal Injury
Patients should be referred for surgical evaluation when demonstrating persistent pain unresponsive to conservative management, recurrent joint stiffness or effusion, mechanical symptoms (locking/catching), persistent instability, or unexpected neurological manifestations. (GRADE C) Additionally, failure to achieve predefined rehabilitation milestones within expected timeframes warrants specialist consultation. (GRADE D) Relative Agreement: Mean 8.24 ± 1.0, median 9 (range 6-9).
Questions and Thoughts
This consensus highlights activities like kneeling and squatting as potential risks, but we must contextualize these findings—proper load progression and recovery protocols likely mitigate risks more than absolute avoidance. In conservative meniscus tear management, we should focus on building resilient movement patterns rather than fostering kinesiophobia through overly restrictive recommendations.
The application of GRADE criteria (from high-quality evidence [A] to expert opinion [D]) warrants clarification. How are these ratings quantitatively determined? While the consensus provides valuable guidance, clinicians implementing conservative meniscus tear management strategies should critically evaluate whether lower-grade recommendations (like cryotherapy in this consensus study) align with emerging paradigms such as PEACE & LOVE principles, which challenge traditional icing protocols.
As we proposed in Part 1 of meniscus rehabilitation, return-to-sport (RTS) decisions remain clinically challenging due to limited evidence on optimal progression. Handheld dynamometry and isokinetic testing, while valuable for quantifying strength, fail to capture the dual load demands of sport: external loads (the measurable biomechanical stresses—cutting, jumping, and pivoting forces) and internal loads (the athlete’s physiological response, including tissue tolerance, cardiorespiratory strain, and perceived exertion). To address this gap, rehabilitation must evolve from isolated strength metrics to sport-specific testing that replicates external loads while rigorously monitoring internal load responses. Only by integrating both dimensions—through progressive drills that simulate competitive demands and real-time physiological assessment—can clinicians establish objective RTS milestones tailored to an athlete’s healed tissue capacity, neuromuscular control, and psychological readiness.
Talk nerdy to me
While the methodological approach was detailed in our prior publication, this analysis specifically examines the evidence-grading framework applied to individual consensus statements.
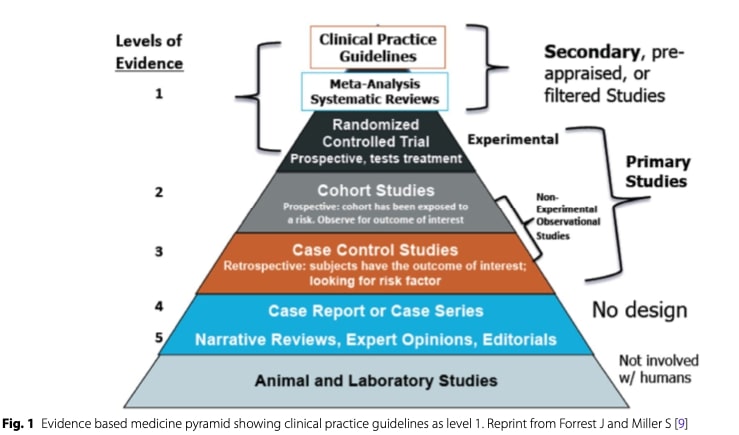
The consensus methodology employs a rigorous evidence hierarchy to assign GRADE levels (A-D) to each clinical statement. At the foundation of this system lies the evidence- based medicine pyramid, where study designs are stratified by their scientific robustness. Randomized controlled trials (RCTs) and meta-analyses occupy the apex as level 1 evidence, providing the strongest support for clinical recommendations through their controlled experimental designs that establish causation. These form the basis for GRADE A recommendations, such as the well-established efficacy of conservative management for degenerative meniscal tears.
Progressing down the pyramid, large prospective cohort studies constitute level 2 evidence, offering valuable correlational data that typically result in GRADE B recommendations. Retrospective case-control studies represent level 3 and 4 evidence and generally correspond to GRADE C, while isolated case reports and expert opinion form level 5 evidence that underpins GRADE D recommendations. The consensus panel evaluated three critical dimensions when assigning these grades: the aggregate risk of bias across available studies, the consistency of findings between studies, and the direct applicability of the evidence to clinical practice.
This systematic approach explains why certain common interventions receive modest grades – their clinical adoption may precede robust evidentiary support. For instance, blood flow restriction training currently holds a GRADE D classification due to limited high-quality studies, despite promising clinical observations. The grading system serves not to dismiss lower-grade recommendations, but to contextualize their evidence base and guide appropriate clinical implementation.
The evidence stratification system, adapted from Forrest and Miller’s foundational work and subsequently modified for the ESSKA consensus methodology, illustrates the authors’ hierarchical approach to classifying evidence levels.
Take-home messages
1. Prevention
- Specific program such as PEP, FIFA11+, and Knäkontroll may reduce injury riskeven though it is not specific to meniscus injuries.
- High-risk movements like cutting with high forces or repetitive deep squatting,heavy lifting increase risk for meniscus pathologies.
2. Conservative and Surgery management.
- No clear rules for surgery vs. rehab, but larger tears (e.g., bucket handle) mayneed surgery (Grade D).
- Degenerative tears? Rehab first—surgery only if symptoms persist after 3–6 months (Grade A).
3. Rehab Essentials
- Early focus: Reduce pain/effusion, restore ROM and quad strength, then improve motor control.
- Tools: NMES, BFR, supervised + home exercises.
- Progress based on milestones and time.
4. Return to Sport (RTS)
- Test strength, hops, psychological readiness before clearing.
- On-field rehab should be sport-specific.
For persistent pain and unresolved symptoms refer to surgeon.
Reference
MASSIVELY IMPROVE YOUR KNOWLEDGE ABOUT LOW BACK PAIN FOR FREE
5 absolutely crucial lessons you won’t learn at university that will improve your care for patients with low back pain immediately without paying a single cent