Achilles Tendinopathy / Achilles Tendinitis | Diagnosis & Treatment

Achilles Tendinopathy / Achilles Tendinitis | Diagnosis & Treatment
Achilles tendinopathy is a common musculoskeletal condition characterized by localized Achilles tendon load-related pain and dysfunction. It is common in both athletic populations and sedentary people, and many suffer profound and longstanding impairments in activities such as walking and running (Turner et al. 2020).
Achilles tendinopathy affects approximately 9% of recreational runners and up to 5% of professional athletes, this condition is career-ending (Lysholm et al, 1987). The incidence of mid-portion Achilles tendinopathy in general practice within the adult population is 2.35 per 1000, and in 35% of cases, a relationship with sports activity has been recorded (de Jonge et al, 2011).
Achilles tendinopathy is a condition that results in the loss of normal collagen architecture, replaced with amorphous, mucinous material, hypercellularity, and increased glycosaminoglycans and neovascularization (Cook et al. 2009). The tendon can be affected within its mid-substance, typically 2cm to 6cm from the insertion point, or at the point of insertion itself.

Pathomechanism
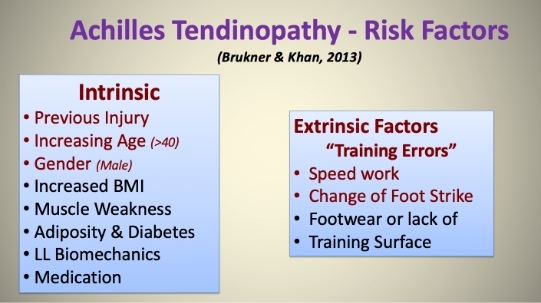
The high prevalence among runners points to mechanical overloading as an important etiological factor. Key risk factors include advanced age, male sex, high body mass index, hypercholesterolemia, and the presence of genetic variants of genes related to collagen mechanisms. The postulated intrinsic etiological factors include tendon vascularity, weakness, as well as lack of flexibility of gastrocnemius–soleus complex, pes cavus, and lateral ankle instability (Van Der Vlist et al. 2019).
Mechanical overload results in inflammation, although the inflammation is not a typical full-blown inflammation (Anderson et al. 2010). The tenocytes produce inflammatory mediators such as Substance P and Prostaglandin E2. The peritendinous region becomes filled with fibrinous exudate (perceived as crepitus) and forms adhesions. The imbalance between matrix degeneration and synthesis leads to intra-tendinous changes. The four cornerstones of histopathology are cellular activation/increase in cell numbers, increase in ground substance, collagen disarray, and neovascularization (Alfredson et al. 2007).
There is also evidence of neurogenic inflammation in the presence of neuropeptides such as Substance P and calcitonin gene-related peptides. The neural pathway may be associated with neovascularization. Biopsies have shown that nerves are in close relationship with neovascularization in areas of tendinosis (Bjur et al. 2005).
The pain mechanisms in tendinopathy are not clear but are thought to involve local nociception mediated by changes within the tenocytes (Rio et al. 2014). The etiology of chronic tendinopathy is complex and multifactorial. The current understanding is the imbalance between the load demands placed on the tendon and its capacity to remodel (Cook et al. 2009).
Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK
Clinical Presentation & Examination
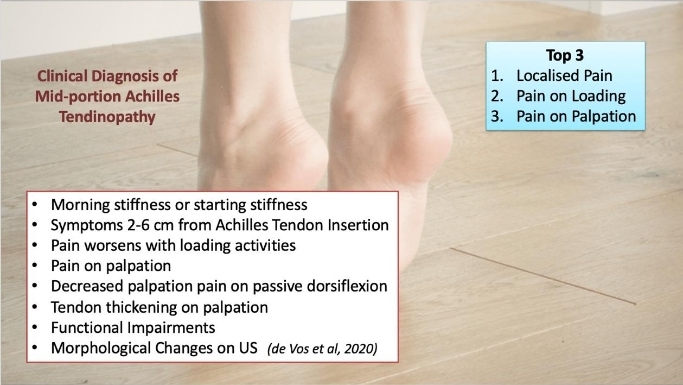
The most common group presenting with non-insertional Achilles tendinopathy are athletes, especially middle to long-distance runners. A common symptom is morning stiffness or stiffness following a period of inactivity. As the condition progresses, pain may occur with even minor exertion and interfere with activities of daily living. In severe cases, pain persists at rest. In the acute phase, the tendon is diffusely swollen and oedematous and tenderness is usually greatest 2-6cm proximal to the tendon insertion. A tender nodular swelling can be present in chronic cases.
There are multiple causes of Achilles tendon pain as shown in the figure below:
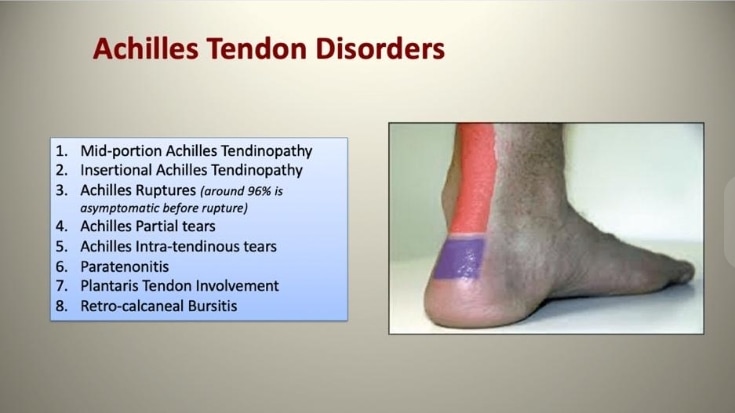
For further information on the differential diagnosis of Achilles tendinopathy, watch the video below:
The patient is examined standing and prone with legs exposed from the knee downwards. The foot and heel should be examined for malalignment, deformity, obvious asymmetry, tendon size, localized thickening, and previous scars. The tendon excursion is examined to determine the tightness of the tendon. A swelling in the tendon due to pure tendinopathy will move with the tendon on movement of the ankle, conversely, swelling of the paratenon will not move (Arc test).
In the Royal London Hospital test, a swelling that is most painful when the ankle is in maximum dorsiflexion indicates tendinopathy. Maffulli et al. (2003) studied sensitivity and specificity of palpation, painful arc test, and Royal London Hospital test in 2003 and found that all three tests had good interobserver agreement.
A later study by Hutchinson et al. (2013), which studied ten clinical tests, found that only two tests, location of pain and pain on palpation, are the most reliable and accurate An overview of diagnostic tests for mid-portion Achilles tendinopathy is described in this video below:
Imaging
Imaging techniques include Ultrasound and Magnetic Resonance Imaging (MRI) scans. Ultrasound may be useful with power Doppler sonography, as Achilles tendinopathy seems to be related to areas of neovascularization. Multiple studies have shown equal or improved accuracy with ultrasound when compared with MRI scans in detecting tendinopathy (Khan et al. 2003). The advantage of ultrasonography over other imaging modalities is its interactive capability and cost-effectiveness.
LEVEL UP YOUR DIFFERENTIAL DIAGNOSIS IN RUNNING RELATED HIP PAIN – FOR FREE!

Follow a course
- Learn from wherever, whenever, and at your own pace
- Interactive online courses from an award-winning team
- CEU/CPD accreditation in the Netherlands, Belgium, US & UK