Responsiveness to scapular repositioning in neck pain

Introduction
Neck pain patients often display tissue sensitivity in the neck and shoulder girdle. Often they report tensed muscles in this region. As several muscles around the shoulder blade are connected to the neck or influence movement in the shoulder girdle, it is a common examination area. Some studies postulated that impaired scapular function may be a risk factor for neck pain. Other studies found different patterns of shoulder girdle orientations in chronic neck pain sufferers. In this light, the correction of scapular positions had been examined previously. Some experienced improvement in neck pain and increased cervical range of motion, while others did not. Therefore, Wannaprom et al. 2021 studied whether subgroups existed based on the outcomes of scapular repositioning in neck pain patients. They found that almost 75% of their sample (who had an altered scapular alignment) responded positively to scapular repositioning. In the current study, the authors investigated whether or not there exist subgroups of neck pain patients based on different scapular orientations. The second aim was to determine why some did and others did not respond positively to scapular repositioning in neck pain.
Methods
A cross-sectional analysis was conducted as part of the previous study by the same research group. The original study included 144 participants and found a positive response in 107 after scapular repositioning in neck pain patients. Of the sample, 37 experienced no clinically meaningful improvement. In the present study, all non-responders to the repositioning were invited. Via a random number generator, the responders of the study were selected on a 1:1 ratio. The sample included participants from 18-59 years who had chronic neck pain (>3 months) with an intensity of at least 3/10 on the VAS in the past week and a current Neck Disability Index of at least 10/100. Furthermore, they had signs of an altered scapular position.
At baseline, they filled in the Neck Disability Index and the response to scapular repositioning was examined. In brief: neck pain and rotation range of motion were examined on an 11-point numeric rating scale (NRS) and using a CROM device, respectively. Hereafter, the clinician modified the scapular position to the “more anatomically correct” position. Then, the neck pain and rotation range of motion was reassessed. An average change score of at least 2 points on the NRS and/or an increase of 7° in cervical rotation range of motion was considered as a positive response to scapular repositioning in neck pain. The position of the scapula was assessed using a 3D measurement with reflective markers.
Results
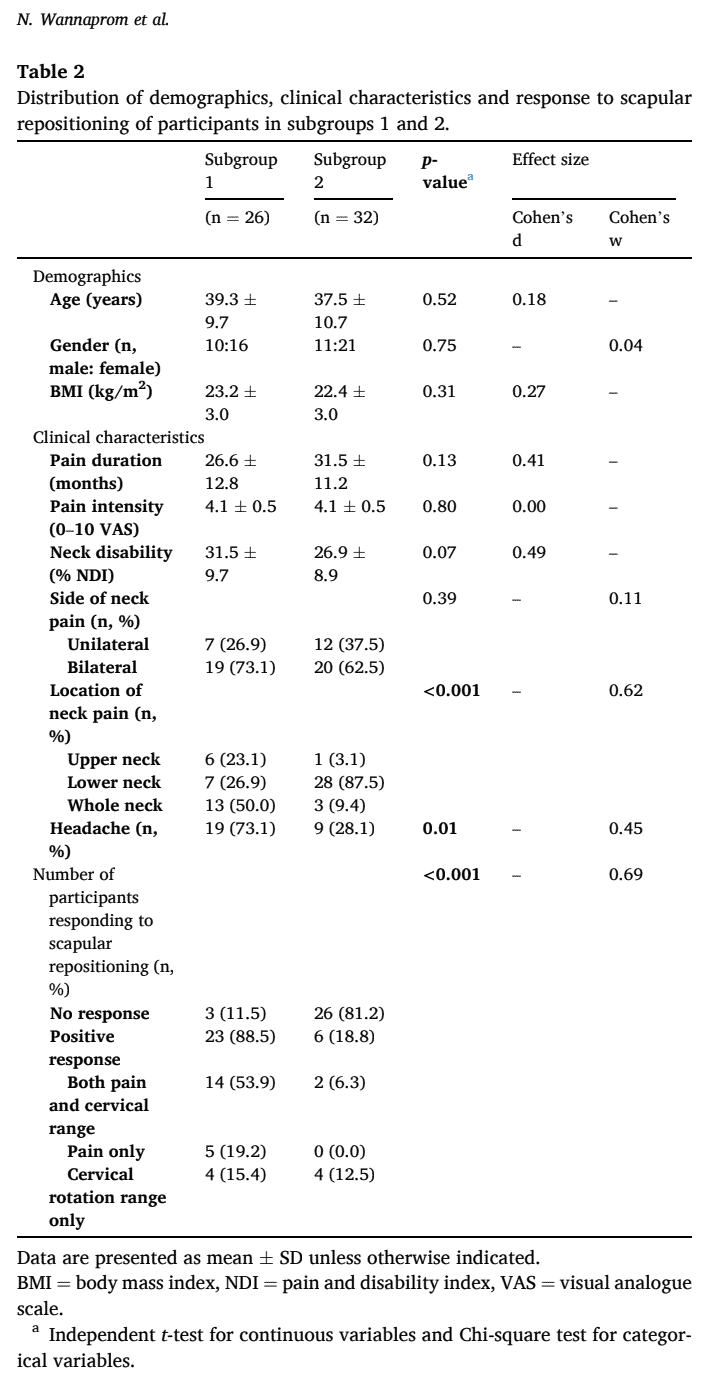
In the current study, 58 participants agreed to participate. Of them, 29 were responders as they had previously experienced positive outcomes on neck pain and range of motion following the scapular repositioning. Twenty-nine people were classified as non-responders. The sample consisted of approximately 60% of women who were 38 years on average (+/- 10 years). Their neck pain intensity was 4.1 (+/- 0.5) on the VAS and they had a Neck Pain Disability Index of 29.0 (+/-9.4).
Two subgroups were identified based on the 3D measurements. In subgroup 1, the participants demonstrated greater clavicular retraction and scapular downward rotation. In subgroup 2, the elevation of the clavicle was increased and the scapula was tilted more anteriorly and rotated more internally. Subgroup 1 had more frequent reports of headaches and more pain in either the upper or whole neck, whereas those from subgroup 2 reported more pain in the lower neck. For all other outcomes (demographics, neck pain intensity, duration, and disability), the subgroups were equal.
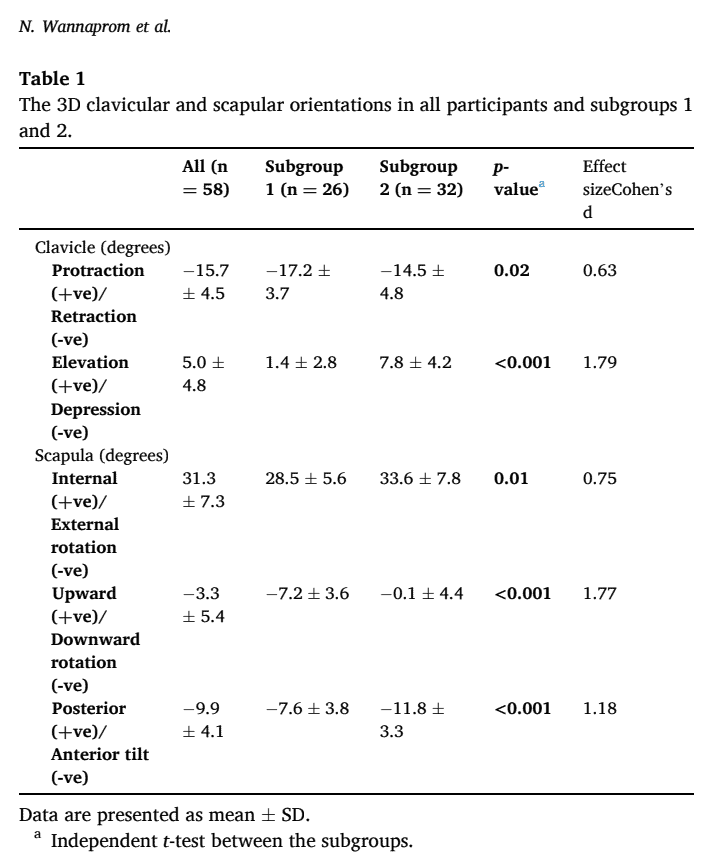
Considering the response to scapular repositioning in neck pain, this study found that 88.5% of participants in subgroup 1 responded positively, whereas 81.2% in subgroup 2 did not.
Questions and thoughts
What can you conclude from these results? Participants with chronic neck pain having frequent reports of headaches, and more pain in the upper neck may respond well to an intervention targeted at repositioning of the shoulder blade. In this study, they displayed more scapular downward rotation and clavicular retraction. This may mean that they have a shortened levator and a lengthened upper trapezius with weakness in the 3 parts of the trapezius and serratus anterior. The fact that the levator muscle attaches to C1-C4 may explain why these patients had more frequent reports of headaches and upper neck pain. The authors postulate that this may contribute to increased upper neck loads.
How can we help scapular reposition in neck pain? The 2021 study by Wannaprom explained:
“Manual repositioning of the scapula was performed ipsilateral to the most painful side of the neck (figure 1). Participants sat in an upright position with hands on thighs and feet flat on the floor. Neck pain intensity and cervical rotation range to the painful side were measured before (uncorrected) and then in the modified (corrected) scapular position. The examiner (an experienced physiotherapist) first observed and then manually assessed the scapular position. The examiner then performed the corrective movements based on this assessment that is, correction of any rotational (upward/ downward, anterior/posterior, internal/external) and translational (superior/inferior, protraction/retraction) positions. During the test, participants were asked to fully relax the muscles of the shoulder girdle and maintain the sitting position without any compensation (eg, thoracic extension and rotation).”

But how is the correct anatomical position defined? Based on the systematic review by Struyf et al. (2014), the scapula should be internally rotated about 40° in respect to the frontal plane and anteriorly tilted about 10°. The medial border of the scapula should be parallel to the thoracic spine. It is normal that the dominant shoulder blade is slightly lower and further away from the spine than the non-dominant scapula. The superior scapular angle lies at T3-T4 and the inferior scapular angle at T7-T8-T9 or T10. This study by Wannaprom used the following procedure to determine the anatomical position:
“The neutral position was defined as the scapula situated parallel to the spine approximately 2 inches from the midline of the thorax, between the second through seventh ribs, rotated forward (in the vicinity of 30◦), inclined slightly inferiorly-laterally, without any prominence of scapular angle and border.”
As you can see, there doesn’t seem to be 1 correct position. Furthermore, not everyone with an altered scapular position has complaints of the neck/shoulder, and equally, having an altered shoulder blade position is not pathological. This scapular repositioning in neck pain may therefore only be relevant in those demonstrating a good response: an increase of rotation range of motion and/or a decrease in pain intensity.
It should be noted that this study made use of 3D measurements to define the orientation of the clavicle and scapula. This is of course not available in clinical practice and would be too time-consuming. To assess the orientation in clinical practice, visual observation of static and semi-dynamic observations were found to be reliable in the review of Struyf et al. (2014). Another useful static measure was the distance of the acromion to the wall. Inclinometry for upward rotation is another reliable method to measure the dynamic movement of the scapula. However, this study used only static measurements.
Talk nerdy to me
A good aspect of this study was that it provided a lot of details, which are needed to reproduce this trial. It would be interesting to see what randomized controlled trials conclude about this scapular repositioning in neck pain. This study found 2 subgroups of neck pain patients based on different scapular orientations, But importantly, the subgroups did not show differences in demographics, neck pain intensity, duration, and disability. So we can assume that the people were quite homogenous, except for their anatomically different orientations in the shoulder girdle and location of neck pain. These subgroups were identified based on large effect sizes.
Further, the trial based its required sample size on the minimum required for cluster analysis. Prior to the 3D measurements of the position of the scapula and clavicle, 8 participants were analyzed to examine the intra-rater reliability of this procedure. The intraclass correlation coefficients showed excellent values with values ranging from 0.81 to 0.94.
Take home messages
This study identified 2 distinct subgroups in chronic neck pain patients based on 3D measurements of scapular orientation. The group who had greater scapular downward rotation and clavicular retraction were responsive to scapular repositioning, whereas those who had more clavicular elevation and internal rotation and anterior tilt of the scapula were non-responsive to scapular repositioning in neck pain. Furthermore, those who were responders had more upper neck pain and headaches, whereas those who did not attain a good response had more lower neck pain. This may have an important role in selecting your treatment options in those patients.
Reference
100% FREE HEADACHE HOME EXERCISE PROGRAM
Download this FREE home exercise program for your patients suffering from headaches. Just print it out and hand it to them for them to perform these exercises at home