Rotator Cuff Tear Treatment Algorithm - Co-Designed by Patients and Clinicians to Improve Care

Introduction
Large to massive rotator cuff tendon tears place a substantial burden on the healthcare system, as there is a misconception at the primary care level that magnetic resonance imaging (MRI) is required to determine which care pathway to follow. This increases patient waiting times and overwhelms secondary and tertiary care settings with people who could have been managed in primary care. Meanwhile, as these waiting times induce treatment delays, the risk for chronicity rises. Since large to massive rotator cuff tears mainly affect the elderly population, the acquired limitations in function and activities of daily living may lead to substantial morbidity and disability.
As it is known that imaging has poor correlation with shoulder symptoms, the overreliance on MRI encourages surgical interventions, which do not significantly outperform exercise-only interventions in all patients affected. Some patients, however, need to be seen by a surgeon. As there is still a lot of diagnostic uncertainty, leading to non-optimized care, more information has to emerge. Therefore, the current study started from scratch to design a care pathway, gathering information and experiences from clinicians, patients, and researchers, to achieve more effective and efficient care. This resulted in a rotator cuff tear treatment algorithm that informs and helps guide care.
Methods
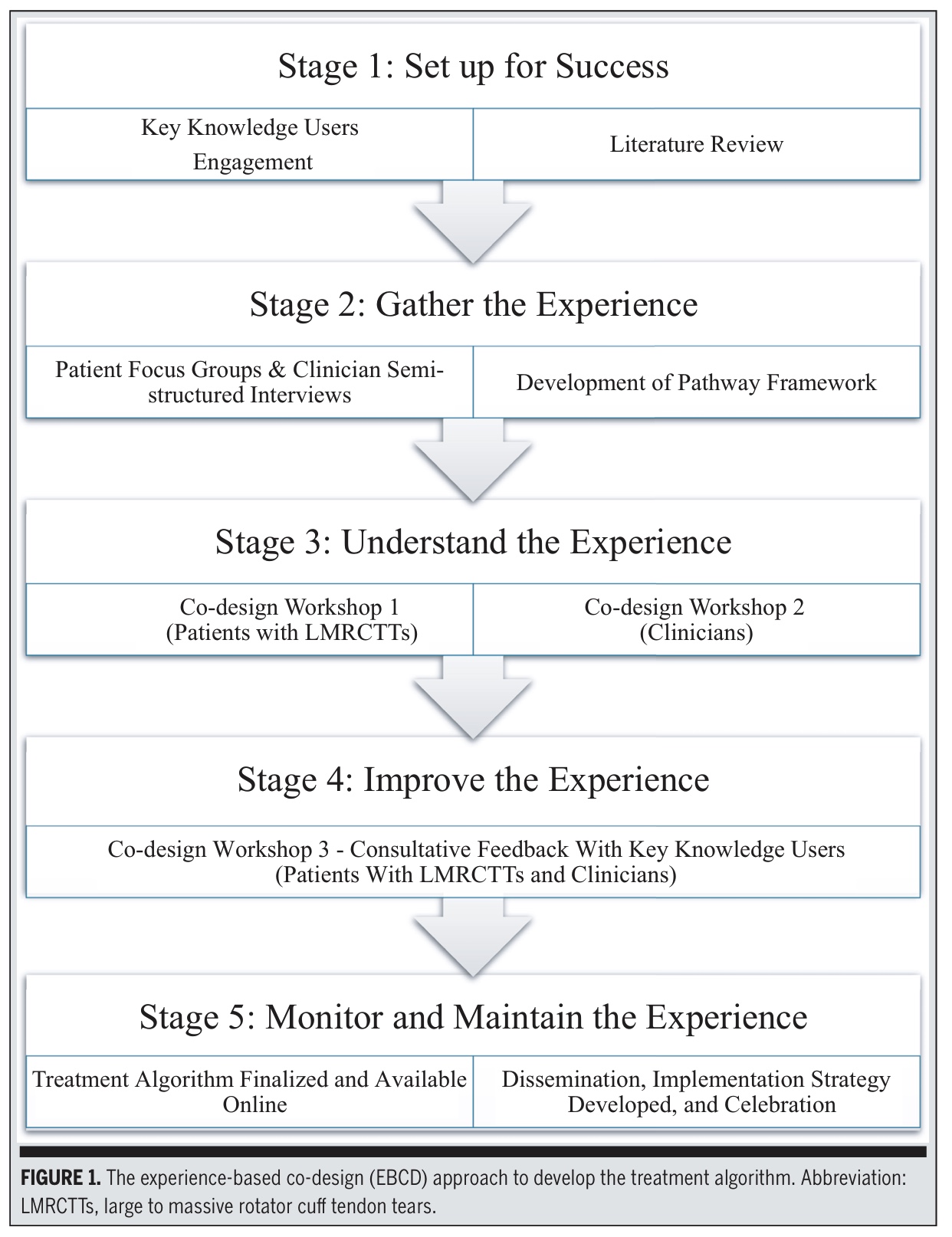
This study used Experience-Based Co-Design (EBCD), which is a mixed-methods participatory methodology involving patients with massive-to-large rotator cuff tears and clinicians as equal partners. These rotator cuff tears were defined as tears involving ≥2 tendons and >3 cm in size. Stages 1–4 were completed over 18 months.
Stage 1: Set up for Success
A steering committee was created, including physiotherapists, orthopaedic surgeons, physicians, and researchers. Findings from a meta-analysis comparing surgery versus exercise for large to massive rotator cuff tendon tears, clinical guideline reviews, and prior qualitative studies were used to draft the initial framework. This foundational work provided the structure and direction needed to begin building a preliminary framework for the treatment algorithm.
Stage 2 – Gather the Experience
Researchers created an initial “skeleton framework” using:
- Patient focus groups
- Clinician semi-structured interviews
- Evidence mapping of best-practice MSK pain guidelines
The researchers created a “skeleton framework” informed by several earlier studies, including patient-focused qualitative research and clinician interviews examining the delivery of shoulder care. They also incorporated insights from concept-mapping work on adherence and examined clinical guideline recommendations for musculoskeletal pain management. This stage involved collecting and synthesizing the lived experiences and professional perspectives that would shape the first draft of the pathway.
Stage 3 – Understand the Experience
The researchers invited a purposive sample of patients with large-to-massive rotator cuff tears and the clinicians who had previously participated in interviews to attend two separate workshops.
Workshop 1 – Patients (n=8)
The first workshop was held face-to-face with patients and presented the initial framework. Patients were asked to identify what had helped or hindered their care at key points along the treatment pathway. Patients discussed their encounters with assessment, imaging, referral processes, and communication. They also contributed ideas regarding how the algorithm should look, feel, and function, and they described behaviours and approaches that health professionals should avoid. Their feedback was consolidated to ensure that their experiences were meaningfully integrated. Most importantly, they indicated what they needed most in communication, education, referrals, and decision-making.
Workshop 2 – Clinicians (n=8)
The second workshop brought together clinicians (surgeons, physicians, and physiotherapists) who reviewed the same framework. They evaluated the strengths and weaknesses of their current services, identified gaps in knowledge or workflow, suggested improvements to the structure and content of the pathway, and refined goals and key principles.
Surgeons, physicians, and physiotherapists together:
- Identified what works in current practice
- Highlighted gaps in appropriateness, triage, and consistency
- Refined the structure and essential decision points
- Requested clarity on when MRI is or isn’t needed
The information of both workshops was combined and integrated into a near-final version.
Stage 4 – Improve the Experience
A third workshop mixed patients and clinicians to finalize the treatment algorithm. Three new patients were added to ensure information saturation. The group:
- Voted on the final layout and usability
- Adjusted emphasis at certain time points
- Added supplementary materials (QR-linked videos, checklists)
Results
In the first two workshops, five intervention components were identified crucial for assessing and treating these massive-to-large rotator cuff tears. From their discussions, the researchers distilled five major “intervention components.” These are essentially the five big areas that must be addressed in any effective care pathway.
These five components (shown in Table 3 of the study) include things like:
- How the first clinical assessment should be conducted
- How information and education should be delivered
- How referrals should be handled
- What the intervention (treatment) should include
- How the care pathway should be structured and communicated
Three “drivers” were identified as essential influences on these five components. A “driver” means an underlying force or theme that shapes everything else.
These drivers are:
- Confidence: Patients need to feel confident in the plan, and clinicians need confidence in their decision-making.
- Education: Everyone agreed that clear, credible, and consistent information is needed to improve understanding and expectations. A need for a “one-stop” resource was expressed both by clinicians and patients
- The Plan: Each patient needs an individualized, well-communicated plan using shared-decision making.
These three drivers act as foundational pillars that support the five intervention components and guide the priorities and outcomes the group identified.
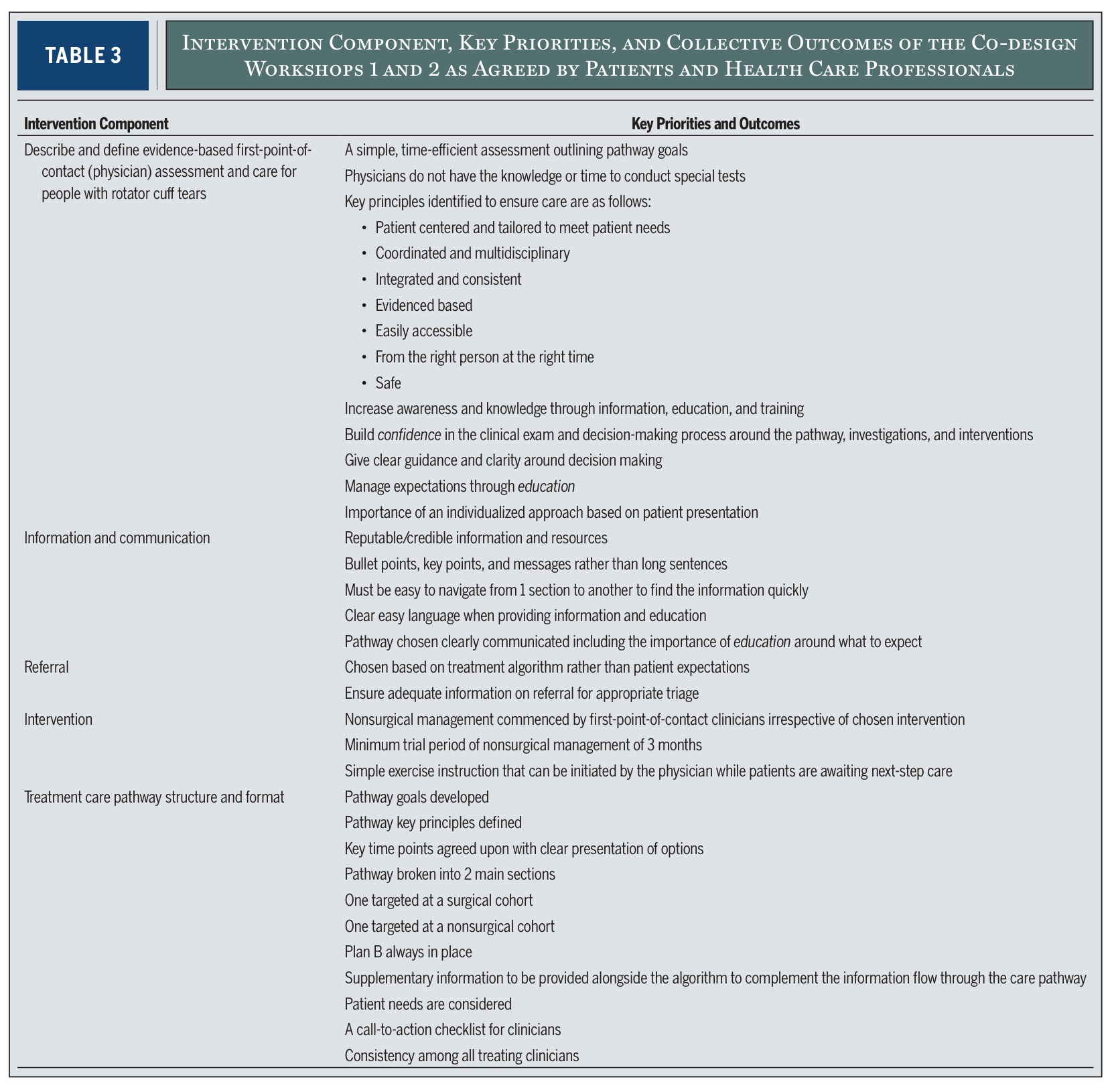
As such, the five components describe what needs to happen in a good care pathway. The three drivers explain what must be present for those components to work effectively. This information was used to create 10 clinical action points to support the assessment and surgical and non-surgical management.
Key Clinical Action Points
Both the clinician and patient groups highlighted the need for:
- Consistent messaging (“clinicians have to speak with one voice”)
- Simple, time-efficient first-point assessment
- Clear education that sets realistic expectations
- A minimum 12-week trial of nonsurgical management for eligible patients
- Better triage criteria for referral and imaging
- Shared decision making and individualized planning
- Simple exercise options linked to pain response
- A ‘Plan B’ for all patients, surgical or nonsurgical
- A call-to-action clinician checklist
- Two separate but connected pathways (surgical & nonsurgical)
The CALMeR Cuff Pathway
Lastly, the final output was constructed. The acronym CALMeR Cuff stands for Comprehensive Approach for Large to Massive Rotator Cuff Tears.
The rotator cuff tear treatment algorithm includes a clinical examination algorithm, consisting of 4 steps:
- Patient selection and red flags: Use key questions to rule out instability, stiff shoulder, or concerning presentations (red flags), according to the British Elbow and Shoulder Society Pathway (BESS).
- Essential clinical exam components
- Age, history, functional demands and onset
- Active ROM in 3 planes: flexion, abduction, hand-behind-back/extension
- Documentation of expectations for treatment
- Pathway division—Surgical vs Nonsurgical
- MRI is not recommended in non-surgical pathway
- MRI is reserved for the surgeon’s consideration when planning surgery
- Use mechanism (traumatic vs persistent/non-traumatic) to guide urgency
- Nonsurgical management recommendations
- At least 12 weeks of home or supervised exercise
- Analgesics as needed
- Physician-initiated basic exercise if wait times exist
- Physiotherapy referral for structured progression
Exercises are described via QR codes and include two gentle rotation-based movements selected for low provocation and high safety.
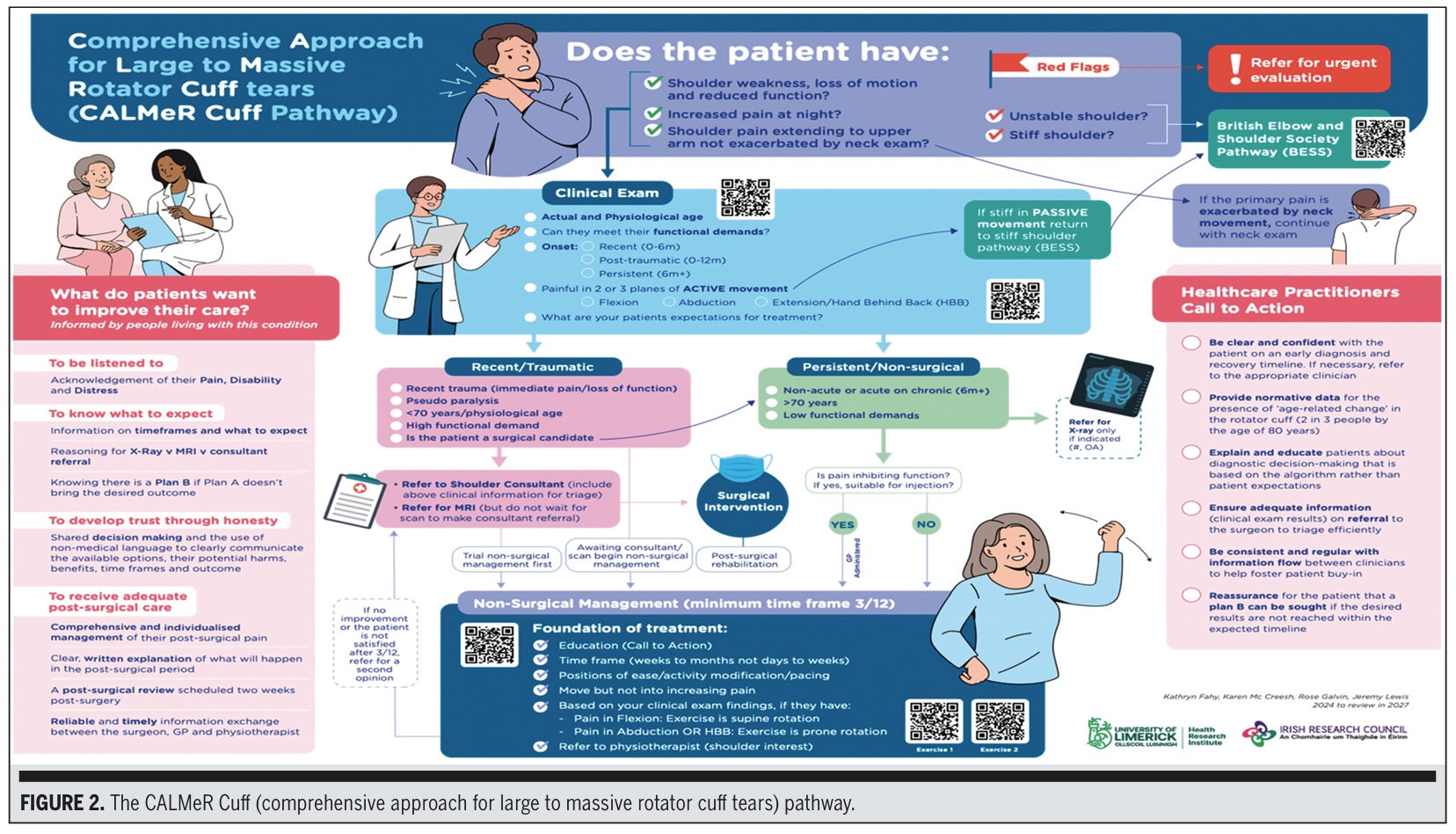
The patients asked:
- To be listened to
- To receive simple, clear explanations
- To know what to expect
- To have confidence in the plan
- To avoid mixed messages
- To understand non-surgical options and timelines
The Healthcare Practitioner Call-to-Action Box contains reminders about:
- Delivering consistent messaging
- Providing early exercise and education
- Using imaging judiciously
- Clear documentation for referrals
Updating patient expectations early
Questions and thoughts
The rotator cuff tear treatment algorithm, as proposed here, offers only two exercises. Although the patients and clinicians agreed on an individualized care pathway, the proposition of two exercises is not per se an individual-targeted approach. Although this framework is designed to provide a starting point for assessment and the associated next steps, its effectiveness has yet to be validated and may change in the future. It isn’t unfair to think that a broader, progressive loading plan could yield better outcomes than 2 exercises, but a care pathway has to start somewhere.
Following the design of the “ideal” care pathway, the logical next step would be to implement this rotator cuff tear treatment algorithm in real-life care settings. Then, when this pathway is implemented, its efficiency and effectiveness have to be validated. So, where this pathway can help organize care, it is not a proven “best” care algorithm (yet).
One key aspect is the need for consistency across providers. Yet, can physiotherapists, general practitioners, and surgeons truly “speak with one voice” across different health systems? This is an important step that enhances patient confidence and will likely also influence patient adherence. If everyone is on the same page and delivers consistent messages, no doubt that the patients will be more reassured that they are in good hands.
The pathway explicitly states that routine MRI is not necessary for nonsurgical management. A trial of 3 months of physiotherapy can, even without having an MRI of the shoulder, produce meaningful differences in a lot of people. Will general practitioners adhere to guidance not to refer for MRI, despite patient expectations and previous practice norms?
Talk nerdy to me
The study by Fahy et al. employed an Experience-Based Co-Design (EBCD) methodology, which is increasingly valued in healthcare improvement research as it combines empirical evidence with real-world user experience. Unlike traditional top-down pathway development, EBCD places equal weight on the insights of patients and clinicians. This approach is particularly interesting in the context of shoulder pain, where diagnostic ambiguity, variable decision-making, and inconsistent care have been reported. By embedding both stakeholder groups across multiple iterative stages, the researchers created a pathway shaped not only by the literature but also by the lived experience of those receiving and providing care. This represents a methodological strength, as it enhances ecological validity and improves the likelihood of clinical uptake. Yet, its effectiveness has not been investigated to date. As the ultimate goal of this rotator cuff tear treatment algorithm is to improve the efficiency and quality of care, implementation-based studies evaluating its adoption in the real-world setting and its ability to change patient outcomes have to be investigated further.
From an analytical standpoint, the study relied entirely on qualitative data. Audio recordings of the workshops were transcribed and subjected to content analysis, an approach that allows researchers to detect patterns across multiple forms of input (discussion, voting, feedback, and behavioural observations). The co-design process used iterative synthesis at each stage, meaning early insights informed the subsequent workshop structures and discussions.
Importantly, the study adhered to the SQUIRE 2.0 standards for quality improvement reporting, which reinforces transparency and methodological rigor even in the absence of quantitative statistics. In qualitative healthcare design, such methodological scaffolding is essential, as it guards against selective interpretation and ensures that each thematic element included in the final pathway is supported by multiple data sources.
The EBCD method also created an interplay between theory-driven and experience-driven knowledge. Evidence from the systematic review and meta-analysis underpinning the project guided the content of the skeleton framework, ensuring that surgical and nonsurgical recommendations were rooted in best available research. Meanwhile, patients provided insight into emotional, behavioural, and practical aspects of their care journey, which are elements that traditional trials often fail to capture. For example, the emphasis on consistent messaging, clear expectations, and credible educational material emerged directly from patient narratives, demonstrating how qualitative methodologies enrich clinical pathways by incorporating aspects of care that profoundly influence adherence and outcomes.
Despite its strengths, the study contains several methodological limitations. The workshops recruited individuals who were likely more motivated, engaged, or health-literate than the general patient population, introducing a risk of selection bias. This could result in a pathway that reflects the needs of more proactive patients while underrepresenting those who are less confident navigating healthcare systems. Furthermore, although the research team consciously attempted to flatten hierarchical dynamics by first seeing the patients and clinicians apart and bringing them together in step 4 only, the potential influence of clinician authority in joint workshops remains a recognised challenge in co-design research. Another limitation is the single-country context; health system structures, referral behaviours, and professional boundaries differ internationally, so the pathway may require adaptation before being applied elsewhere. Finally—and perhaps most importantly—the CALMeR Cuff pathway has not yet undergone feasibility or implementation testing. While the design is methodologically sound and strongly grounded in stakeholder experience, its real-world effectiveness remains untested.
Take-home messages
This study created the first co-designed rotator cuff tear treatment algorithm, specifically for large-to-massive rotator cuff tears, combining evidence with patient experience. For most patients, nonsurgical care should start immediately, including simple exercises and education. The pathway states that MRI and surgery are not automatically needed. Furthermore, the pathway aims to ensure everyone (general practitioners, physiotherapists, and surgeons) provides consistent messages, coordinated work, and confidence-building care. The algorithm has not yet been tested in real-world clinics. Until feasibility and effectiveness studies occur, its practical impact remains uncertain.
Reference
TWO MYTHS BUSTED & 3 KNOWLEDGE BOMBS FOR FREE
What university doesn’t tell you about shoulder impingement syndrome and scapula dyskinesis and how to massively level up your shoulder game without paying a single cent!