RCRSP Exercise or Education?

Introduction
Rotator cuff-related shoulder pain (RCRSP) forms a substantial burden as it is associated with decreased function and pain. As such, people can avoid moving their arms, adopt movement-related fear and develop catastrophization. To counteract this, a good session of physiotherapy would start with education where information is provided about the condition to tackle false illness beliefs and kinesiophobia and to improve self-efficacy. But as the condition of RCRSP leads to strength and movement-related complaints, it is possible that education on itself would not be adequate enough to tackle the movement problems. Therefore, the management of RCRSP is frequently supplemented by exercise. In this spectrum, the most common exercise approaches are strengthening and motor control exercises. To date, none of the exercise approaches has shown to be superior to the other, the aim of this study was to compare the effectiveness when added to education.
Methods
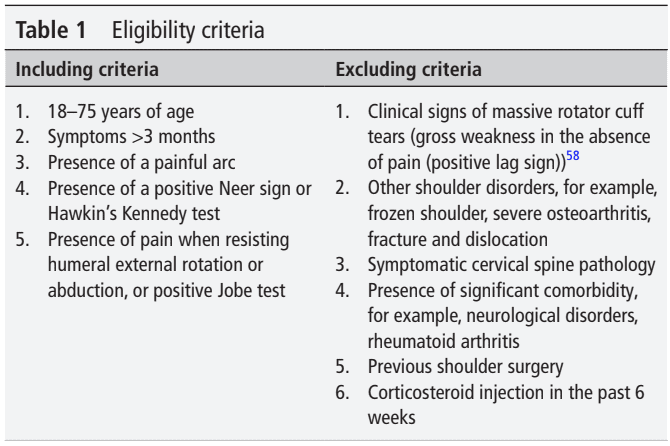
This study used a randomized controlled design to include adult participants with RCRSP between the ages of 18-75 years. They had shoulder symptoms for more than 3 months and a painful arc. They were examined with the Neer sign, Hawkin’s Kennedy test, resisted shoulder external rotation and abduction, and the Jobe test. At least 3 positive tests were required to include RCRSP. This cluster was proposed to include the subjects in this study and was adapted from Michener et al., 2009.
The study was set up to compare the three interventions over the course of 12 weeks. A group receiving education was compared to a group where strengthening exercises were added to the education program and to a group performing motor control exercises on top of education. The education group received 2 education sessions over the 12-week period. The exercise groups participated in 6 intervention sessions over 12 weeks.
The education which was provided for every group consisted of basic shoulder anatomy and function, pain science, pain management, and activity modification. This was provided in the two educational sessions and thereafter, participants were required to watch a series of educational videos which discussed the importance of physical activity, healthy sleep, and eating habits and further highlighted the previously discussed anatomy, and pain management principles.
In the strengthening group, the education described below was provided together with a progressive shoulder strengthening program. Both concentric and eccentric exercises were performed at 90% of 1RM using free weights and resistance bands. The exercises were targeted at the internal and external rotators, abductors, and scapular muscles. One set of the maximum number of repetitions was performed until muscular fatigue. With increasing or decreasing pain levels, the required repetitions were lowered or increased respectively.
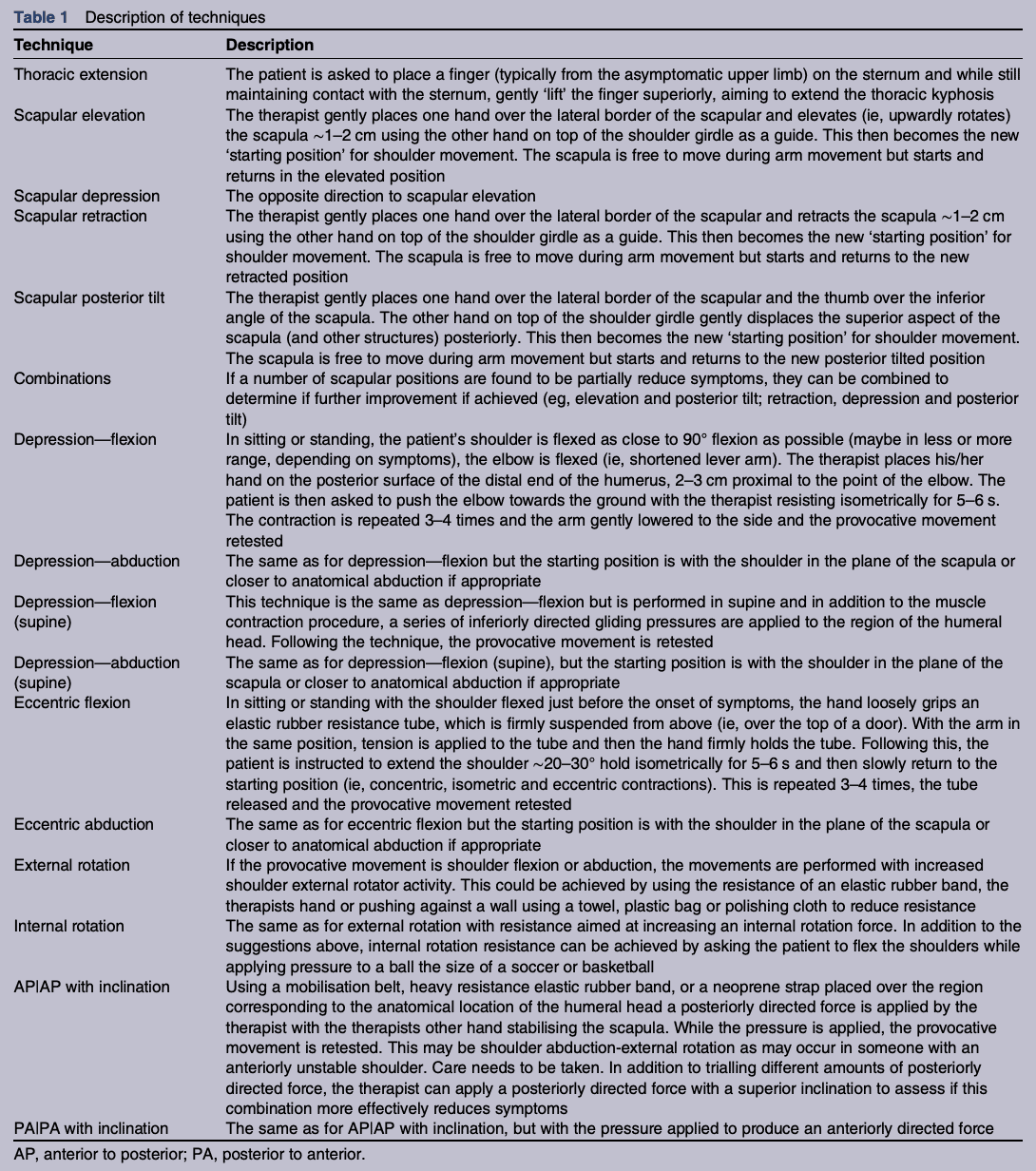
The motor control group received the same educational advice and participated in shoulder symptom modification procedures to alleviate symptoms during shoulder movements, based on Lewis et al., 2016. Briefly, this incorporated identifying symptom-reproducing movements, activities, or postures from daily activities to work-related and sports-related activities. Symptoms were defined as pain, reduction in movement, instability, and symptoms associated with neurovascular compromise. Basically, the symptom-modification procedure was described as follows:
“A series of clinical tests were performed in a sequential format through three key areas: thoracic ‘finger on sternum technique’, scapular procedures, ‘humeral head’ procedures. If a technique reduced pain, that technique was then used during elevation exercises in three planes (flexion, abduction, scaption) and incorporated into the participant’s everyday functional movements. MCE during arm elevation progressed through a standardized six-phase retraining sequence, where external feedback was progressively decreased and the external load was slowly increased (without the load exceeding 50% of 1 RM (>15 reps)).”
When we dive into the references of the symptom-modification procedure, this is the description of possible modifiers.
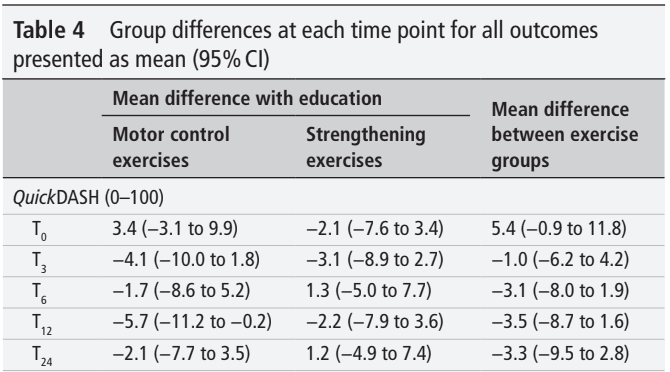
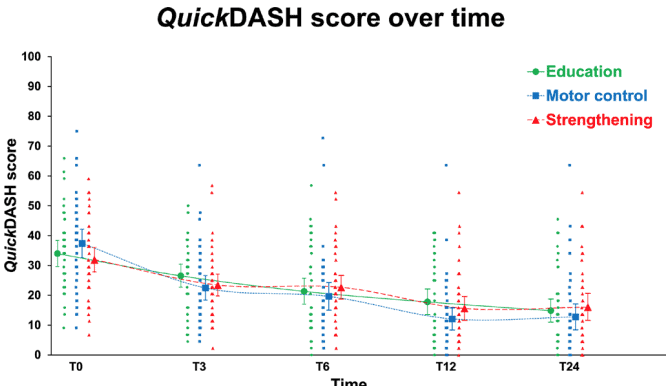
The outcome of interest was the QuickDASH, which is an 11-item questionnaire that measures the physical function and symptoms related to the shoulder. The minimal clinically important difference (MCID) was 8.0 points for the QuickDASH and the minimal detectable change (MDC) was 11.2 points.
Results
A total number of 123 participants were included in the RCT. They were on average 47 years old and had RCRSP complaints for on average 2 years. As you can see, every participant, independent of group allocation, improved. The difference from the baseline scores at 24 weeks exceeded the MCID and MDC for all interventions.
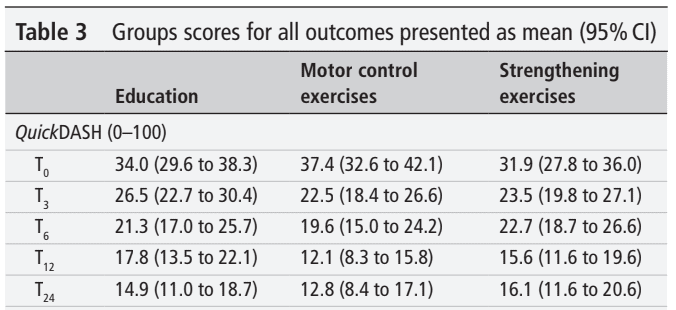
The results of the primary outcome measure analysis revealed no significant between-group differences. This means that none of the interventions was superior to education alone. Every week, participants improved their QuickDASH score by on average 0.8 points or 1.3 points when the improvement was calculated over the 24-week or 12-week intervention period respectively.
Questions and thoughts
The acromioclavicular distance was also evaluated. Though the power was not calculated on this outcome, the analysis revealed that despite the improvements in every group, the acromioclavicular distance did not change over the course of this study. This confirms further that compression of the rotator cuff tendons under the acromion is not responsible for RCRSP.
The inclusion criteria specified the maximum age of 75 years. The mean age in the education group, for example, was 47.9 +/- 15.3 years. The older the patient, the more likely degenerative changes lie at the root of the RCRSP problem. The analysis did adjust for age, but unfortunately, no further information was provided based on subgroups of age categories. It could have been interesting to see whether there was a difference in response in younger versus older adults.
An interesting, yet simple manner to check whether your patient captured the educational information you provided was by asking them to summarize what they learned. After watching the educational videos, the participants were asked what the most important message of the video itself was. This way, it was ensured participants captured the important bits of information they were provided with. A question as simple as that, but nonetheless of value. This is something that I would take from this study to use in practice myself.
Talk nerdy to me
No differences in outcomes were seen when participants were given loading exercises on top of education. As this study did not include a true control group, we cannot say that it is the educational part that leads to the improvement of function and symptoms, or just the natural history. This should be taken into account. Nonetheless, the included patients had RCRSP symptoms for more than 1,5-2 years, as was recorded by the baseline characteristics. Therefore, we could cautiously conclude that the improvements are likely not due to natural history itself.
This RCT was rigorously conducted. What was interesting for me was the high-load strengthening exercises (90% of 1RM) and in particular the absence of adverse events. Again, this points to exercise being safe, even when it is performed at high intensity. A very good approach to progressions was made. At each strengthening session, the participant’s force was reassessed and the resistance program was adapted accordingly. The authors noted that, despite their determination of the 90% of 1RM, this may have been influenced by pain and, or, kinesophobia and thus may not have reflected the true 90% 1RM. This is, in my opinion inevitable, and the weekly follow-up measures of the strength to adapt the loading intensity could have tackled this.
Adherence to the exercise approaches was good, with 86% and 82% respectively for the motor control exercises and strengthening exercises. No adverse effects were reported and so, we could conclude that both exercise options were feasible. The methodology specified for the motor control exercises that these progressed to whole-body functional movements once a pain-free execution was possible. Despite this, no information was provided on the percentages of participants attaining this pain-free stage.
Take home messages
The improvements in QuickDASH over the course of the intervention was approximately 1 point per week. The MCID of this patient-reported questionnaire is 8 points. You could therefore, based on these results, give a prognostication to your patient with RCRSP that it will take about 8 weeks before meaningful changes appear. This advice could be necessary to get your patient to stick to the rehab plan (whether it includes education alone or combined with strengthening or motor control exercises) and avoid them wanting a ‘quick fix’.
Both groups improved to the same extent as the education-only group. The most important message you can take from this study is that you have to educate your RCRSP patient very well, and you can add exercise on top of that. Both the high-load and low-load (more movement-quality related motor control exercises) led to the improvement of QuickDASH scores when added to education.
Reference
Additional references
TWO MYTHS BUSTED & 3 KNOWLEDGE BOMBS FOR FREE
What university doesn’t tell you about shoulder impingement syndrome and scapula dyskinesis and how to massively level up your shoulder game without paying a single cent!